Adenoid cystic carcinoma
| Adenoid cystic carcinoma | |
|---|---|
| Other names | Adenocyst, Malignant cylindroma, Adenocystic, Adenoidcystic |
 | |
| Micrograph of an adenoid cystic carcinoma of a salivary gland (right of image): Normal serous glands, typical of the parotid gland, are also seen (left of image), H&E stain. | |
| Specialty | Oncology |
Adenoid cystic carcinoma is a rare type of
It is the third-most common malignant salivary gland tumor overall (after
Cause
Activation of the oncogenic transcription factor gene MYB is the key genomic event of ACC and seen in the vast majority of cases.[4][5] Most commonly, MYB is activated through gene fusion with the transcription factor encoding NFIB gene as a result of a t(6;9) translocation.[4] Alternatively, MYB is activated by copy number gain or by juxtaposition of enhancer elements in the vicinity of the MYB gene.[6] In a subset of ACCs, the closely related MYBL1 gene is fused to NFIB or to other fusion partners.[7][8]
MYB drives proliferation of ACC cells and regulates genes involved in cell cycle control, DNA replication and repair, and RNA processing.[9] Thus, the MYB oncogene is a potential diagnostic and therapeutic target in ACC.
ACC has a relatively quiet genome with few recurrent copy number alterations or point mutations,[6][10][11][12] consistent with the view that MYB and MYBL1 are the main oncogenic drivers of the disease.
Treatment
Primary treatment for this cancer, regardless of body site, is surgical removal with clean
Images
-
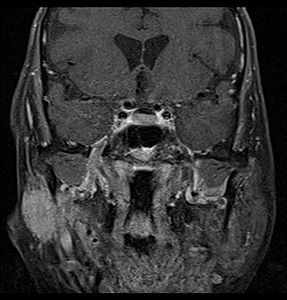
Coronal MRI showing right parotid adenoid cystic carcinoma with perineural spread of tumor: The tumor originates in the right parotid gland and spreads along the trigeminal nerve via the auricuotemporal branch extending intracranially through the foramen ovale at the skull base towards Meckel's cave.
-
Coronal MRI showing right parotid adenoid cystic carcinoma with perineural spread of tumor along the facial nerve extending to the stylomastoid foramen
-
Histopathological image of adenoid cystic carcinoma of the salivary gland infiltrating a nerve (center), H&E stain
-
Histopathological image of adenoid cystic carcinoma of the salivary gland, immunostain for S-100 protein
-
Micrograph of adenoid cystic carcinoma,Pap stain
-
Adenoid cystic carcinoma with comedonecrosis
-
Relative incidence of submandibular tumors, with adenoid cystic carcinoma being the second most common.[17]
-
Relative incidence of parotid tumors, with adenoid cystic carcinoma being relatively rare.[17]
See also
References
- PMID 20203221.
- S2CID 5935648.
- PMID 10037280.
- ^ PMID 19841262.
- PMID 27101980.
- ^ S2CID 25742114.
- PMID 26631070.
- PMID 26631609.
- PMID 28954282.
- PMID 23685749.
- PMID 23778141.
- PMID 26862087.
- PMID 3114190.
- PMID 8949762.
- PMID 10701733.
- PMID 10897760.
- ^ a b Lee SC (23 December 2021). "Salivary Gland Neoplasms". Medscape. Updated: Jan 13, 2021
Diagrams by Mikael Häggström, MD
Further reading
- Neville, Damm, Allen, Bouquot. Oral and Maxillofacial Pathology. 2nd edition.






![Relative incidence of submandibular tumors, with adenoid cystic carcinoma being the second most common.[17]](http://upload.wikimedia.org/wikipedia/commons/thumb/a/a7/Relative_incidence_of_submandibular_tumors.png/519px-Relative_incidence_of_submandibular_tumors.png)
![Relative incidence of parotid tumors, with adenoid cystic carcinoma being relatively rare.[17]](http://upload.wikimedia.org/wikipedia/commons/thumb/b/b1/Relative_incidence_of_parotid_tumors.png/517px-Relative_incidence_of_parotid_tumors.png)