Adverse childhood experiences
Adverse childhood experiences (ACEs) include childhood
Definition and types
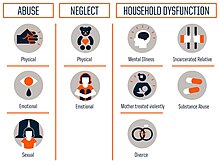
The concept of adverse childhood experiences refers to various traumatic events or circumstances affecting children before the age of 18 and causing mental or physical harm.[9] There are 10 types of ACEs:
- Physical abuse: Any intentional act that causes physical harm through bodily contact.
- Sexual abuse: Any forceful, unwanted, or otherwise abusive sexual behavior.
- Psychological abuse: Any intentional act that causes psychological harm, such as gaslighting, bullying, or guilt-tripping.
- Physical neglect: Failure to help meet the basic biological needs of a child, such as food, water, and shelter.
- Psychological neglect: Failure to help meet the basic emotional needs of a child, such as attention and affection.
- Witnessing domestic abuse: Observing violence occurring between individuals in a domestic setting, such as between parents or other family members.
- Witnessing drug or alcohol abuse: Having a close family member who misused drugs or alcohol.
- Mental health problems: Having a close family member or otherwise important individual experience mental health problems.
- Imprisonment: Having a close family member or otherwise important individual serve time in prison.
- Parental separation or divorce: Parents or guardians separating or divorcing on account of a relationship breakdown.[9]
The different adverse childhood experiences are not isolated and in many cases multiple ACEs impact someone at the same time.
Prevalence
Adverse childhood experiences are common across all parts of societies, in 2009 the CDC started collecting data on the prevalence of ACEs as part of the Behavioral Risk Factor Surveillance System (BRFSS).[10] In the first year data was collected across five US states and included over 24,000 people. The prevalence of each ACE ranged from a high of 29.1% for household substance abuse to a low of having an incarcerated family member (7.2%). Approximately one quarter (25.9%) of respondents reported verbal abuse, 14.8% reported physical abuse, and 12.2% reported sexual abuse. For ACEs measuring family dysfunction, 26.6% reported separated or divorced parents; 19.4% reported that they had lived with someone who was depressed, mentally ill, or suicidal; and 16.3% reported witnessing domestic violence. Men and women reported similar prevalences for each ACE, with the exception of sexual abuse (17.2% for women and 6.7% for men), living with a mentally ill household member (22.0% for women and 16.7% for men), and living with a substance-abusing family member (30.6% for women and 27.5% for men). Younger respondents more often reported living with an incarcerated and/or mentally ill household member. For each ACE, a sharp decrease was observed in prevalence reported by adults aged ≥55 years. For example, the prevalence of reported physical abuse was 16.9% among adults aged 18--24 years compared with 9.6% among those aged ≥55 years.[11]
Non-Hispanic black respondents reported the lowest prevalence of each ACE category among all racial/ethnic groups, with the exception of having had an incarcerated family member, parental separation or divorce, and witnessing domestic violence. Hispanics reported a higher prevalence than non-Hispanic whites of physical abuse, witnessing domestic violence, and having an incarcerated family member (p<0.05). Those respondents with less than a high school education compared with those with more than a high school education had a greater prevalence of physical abuse, an incarcerated family member, substance abuse, and separation/divorce. Among the five states, little variation was observed.
Approximately 41% of respondents reported having no ACEs, 22% reported one ACE, and 8.7% reported five or more ACEs. Men (6.9%) were less likely to report five or more ACEs compared with women (10.3%). Respondents aged ≥55 years reported the fewest ACEs, but the younger age groups did not differ from one another. Non-Hispanic blacks were less likely to report five or more ACEs (4.9%) compared with non-Hispanic whites (8.9%), Hispanics (9.1%), and other non-Hispanics (11.7%). However, non-Hispanic black respondents were not significantly more likely to report zero ACEs compared with other racial/ethnic groups. Respondents with the lowest educational attainment were significantly more likely to report five or more ACEs compared with those with higher education levels (14.9% versus 8.7% among high school graduates and 7.7% in those with more than a high school education). Overall, little state-by-state variation was observed in the number of ACEs reported by each respondent.[11][12][13]
There are no reliable global estimates for the prevalence of child maltreatment. Data for many countries, especially low- and middle-income countries, are lacking. Current estimates vary widely depending on the country and the method of research used. Approximately 20% of women and 5–10% of men report being sexually abused as children, while 25–50% of all children report being physically abused.[14][15]
Health outcomes due to ACEs
Childhood
With one in four children experiencing or witnessing a potentially traumatic event, the relationship between ACEs and poor health outcomes has been established for years.
Adulthood
Adults with ACE exposure report having worse mental and physical health, more serious symptoms related to illnesses, and poorer life outcomes.[36][37] Across numerous studies these effects go beyond behavioral and medical issues, and include damage to DNA,[37] higher levels of stress hormones,[38] and reduced immune function.[39] The effects of ACEs goes beyond just physical and behavioral health with studies reporting that people with high ACEs scores showed less trust in government COVID-19 information and policies.[40]
It is thought that all adult depression results from something happening in childhood. That could be things like aversive childhood experiences that lead to depression, or if something that happens in adulthood that leads to depression tends to stem from something that happened in childhood as well. It seems that the main things that led children to have adult depression is that of their parent's mental health issues and childhood neglect.[41] [irrelevant citation]
Biological changes
Due to many of the early life stressors caused by exposure to ACEs there are noted changes the body in people with ACE exposures compared to people with little to no ACE exposure.
Physical health
ACEs have been linked to numerous negative health and lifestyle issues into adulthood across multiple countries and regions including the United States,[52] the European Union,[53] South Africa,[54] and Asia.[55] Across all these groups researchers have reported seeing the adoption of higher rates of unhealthy lifestyle behavior including sexual risk taking,[56] smoking,[57] heavy drinking,[58] and obesity.[59][60] The associations between these lifestyle issues and ACEs shows a dose response relationship with people having four or more ACEs have significantly more of these lifestyle problems.[61][62] Physical health problems arise in people with ACEs with a similar dose response relationship.[56] Chronic illnesses such as asthma,[63] arthritis,[56] cardiovascular disease,[64] cancer,[65] diabetes,[66] stroke,[67] and migraines[68] show increased symptom severity in step was exposure to ACEs.[56]
Mental health
Mental health issues have been well known in the face of childhood trauma and exposure to ACEs is no different. According to a large study conducted in 21 countries nearly one in three mental health conditions in adulthood are directly related to an adverse childhood experience.[69]
Multiple mental health conditions found to have a dose response relationship with symptom severity and prevalence including depression,[70][71] attention-deficit/hyperactivity disorder,[72] anxiety[73][74] suicidality,[75] bipolar disorder and schizophrenia.[76] Depressive symptoms in adulthood showed one of the strongest dose response relationships with ACEs, with an ACE score of one increasing the risk of depressive symptoms by 50% and an ACE score of four or more showing a fourfold increase.[77] Later research also demonstrated that ACE scores are related to increased rates and severity of psychiatric and mental disorders, as well as higher rates of prescription psychotropic medication use.[22]
Special populations
Additionally, epigenetic transmission may occur due to stress during pregnancy or during interactions between mother and newborns. Maternal stress, depression, and exposure to partner violence have all been shown to have epigenetic effects on infants.[25][78]
Implementing practices
Globally knowledge about the prevalence and consequences of adverse childhood experiences has shifted policy makers and mental health practitioners towards increasing, trauma-informed and resilience-building practices.[79][80][81] This work has been over 20 years in the making bringing together research are implemented in communities, education settings,[82] public health departments, social services, faith-based organizations and criminal justice.[83][84]
Communities
As knowledge about the prevalence and consequences of ACEs increases, more communities seek to integrate trauma-informed and resilience-building practices into their agencies and systems.[85]
Indigenous populations show similar patterns of mental and physical health challenges as other minority groups.[86] Interventions have been developed in American Indian tribal communities and have demonstrated that social support and cultural involvement can ameliorate the negative physical health effects of ACEs.[87]
There is a paucity of empirical research documenting the experiences of communities who have attempted to implement information about ACEs and trauma-informed practice into widespread public action. A study on Pottstown, Pennsylvania's process demonstrated the challenges associated with community implementation. The Pottstown Trauma-Informed Community Connection (PTICC) initiative evolved from a series of prior collectives that all had similar goals of creating community resilience in order to prevent and treat ACEs. Over the course of the two-year study, over 230 individuals from nearly 100 organizations attended one training offered by the PTICC, raising the number of engaged public sectors from 2 to 14. Participation in training and events was fairly steady and this was largely due to community networking.[88]
However, the PTICC faced several challenges similar to those predicted by the Building Community Resilience model. These barriers included availability of resources over time, competition for power within the group, and the lack of systemic change needed to support long-term goals. Still, Pottstown has built a trauma-informed community foundation and offers lessons to other communities who have similar goals: start with a dedicated small team, identify community connectors, secure long-term financial backing, and conduct data-informed evaluations throughout.[88]
Other community examples exist, such as Tarpon Springs, Florida which became the first trauma-informed community in 2011.[89][90] Trauma-informed initiatives in Tarpon Springs include trauma-awareness training for the local housing authority, changes in programs for ex-offenders, and new approaches to educating students with learning difficulties.[91]
Education
ACEs exposure is widespread globally, one study from the National Survey of Children's Health in the United States reported that approximately 68% of children 0–17 years old had experienced one or more ACEs.[92] The impact of ACEs on children can manifest in difficulties focusing, self regulating, trusting others, and can lead to negative cognitive effects. One study found that a child with 4 or more ACEs was 32 times more likely to be labeled with a behavioral or cognitive problem than a child with no ACEs.[93] Another study found that students with at least three ACEs are three times as likely to experience academic failure, six times as likely to have behavioral problems, and five times as likely to have attendance problems.[94] The trauma-informed school movement aims to train teachers and staff to help children self-regulate, and to help families that are having problems that result in children's normal response to trauma. It also seeks to provide behavioral consequences that will not re-traumatize a child.[95]
Trauma-informed education refers to the specific use of knowledge about trauma and its expression to modify support for children to improve their developmental success.[96] The National Child Traumatic Stress Network (NCTSN) describes a trauma-informed school system as a place where school community members work to provide trauma awareness, knowledge and skills to respond to potentially negative outcomes following traumatic stress.[97] The NCTSN published a study that discussed the Attachment, Self-Regulation, and Competency (ARC) model, which other researchers have based their subsequent studies of trauma-informed education practices off of.[93][98] Trauma-sensitive or trauma-informed schooling has become increasingly popular in Washington, Massachusetts, and California in the last 10 years.[92]
In their 2002 survey, the AAUW reported that, of students who had been harassed, 38% were harassed by teachers or other school employees. One survey that was conducted with psychology students reports that 10% had sexual interactions with their educators; in turn, 13% of educators reported sexual interaction with their students.
Literacy
ACEs in childhood and adolescence can affect literacy development in many ways. Children who have faced trauma encounter more learning challenges in school and higher levels of stress internally.[101] Building literacy skills can be negatively impacted both by the lack of literacy experiences in the home, missing parts of early-childhood education, and by actually altering brain development. There are techniques that can be employed by educators and clinicians to try and remediate the effects of the adverse experiences and move children forward in their literacy and educational development.[102]
ACEs affect parts of the brain that involve memory, executive functioning, and attention.[103] The parts of the brain and hormones that register fear and stress are in overdrive, whereas the prefrontal cortex, which regulates executive functions, is compromised. This impacts impulse control, focus, and critical thinking.[104] Memory is also a struggle as there is less capacity to process new input.[101] The stress of ACEs creates a state of "fight, flight, or freeze" which leaves children unavailable for learning.[101] The ability to process new information or collaborate with peers in school is eclipsed by the brain's necessity to survive the stress experienced in their environment outside of school.[103] The inconsistency and instability of the home environment alters the many cognitive processes necessary for effective literacy acquisition.
Young people who are refugees experience trauma whether they were part of the immigration process or were born in the country (where they currently attend school) where the family settled[citation needed]. During this resettlement phase[105] many of the second-generation refugee child's problems come to light. The disruption in education and instability in the home, as a result of the family's journey, can lead to gaps in exposures to literacy in the home [citation needed]. Literacy experiences outside of school include parents reading with kids and borrowing or buying books for the home.[104] Early-childhood literacy education includes explicit teaching of reading and writing skills, building phonological awareness, and academic vocabulary.[104] Resettlement affects children's phonemic awareness and exposure to academic vocabulary since many families are unable to fully provide these out of school experiences.[105] If the child was non-English speaking, then they are acquiring English as a new language. There already exists an achievement gap between native-English speakers in the United States and students who are learning English as their second (or third or fourth) language.[105]
The resulting literacy issues from trauma, reflected in low reading scores, puts children with ACEs at-risk for grade retention. As students, they are almost twice as likely to leave high school without graduating.[106] While there are many years from when a young child starts kindergarten and an adolescent enters high school, there is a link between weak emergent literacy leading to eventually dropping out of high school.[106] It is crucial to intervene as early as possible.
Trauma-informed educators and clinicians can help remediate both young children and adolescents in school. With a knowledge and sensitivity of ACEs and their effects, proper and effective interventions can be implemented.[107] This can also begin to create a stable environment in which children can learn and create stable attachments.[104] Physical movement in the form of "brain energizers" can help regulate children's brains and alleviate stress when done 1–2 times during the school day. In one study, both behavior and literacy skills were assessed to see how effective the physical movement, or "brain energizers" were.[101] Literacy scores for a classroom that used the brain energizers (which ranged from movement activities found online to other movement activities selected by the teacher and students), improved by 117% from beginning to end of year.[101] In a school setting, the person who has experienced trauma and the person who is in the moment with the person trying to talk or write about it can connect, even when language fails to adequately describe the depth and complexity of the emotions felt.[108] While there is an inherent discomfort in this, educators can embrace this discomfort and give children a space to express this, as best they can, in the classroom. Those who are able to develop more "resilience" might be able to function better in school, but this is dependent on the ratio of protective factors[103] compared to ACEs.
Social services
Social service providers—including welfare systems, housing authorities, homeless shelters, and domestic violence centers – are adopting trauma-informed approaches that help to prevent ACEs or minimize their impact. Utilizing tools that screen for trauma can help a social service worker direct their clients to interventions that meet their specific needs.[109] Trauma-informed practices can also help social service providers look at how trauma impacts the whole family.[110]
Trauma-informed approaches can improve child welfare services by openly discussing trauma and addressing parental trauma.[according to whom?][111] The New Hampshire Division for Children Youth and Families (DCYF) is taking a trauma-informed approach to their foster care services by educating staff about childhood trauma, screening children entering foster care for trauma, using trauma-informed language to mitigate further traumatization, mentoring birth parents and involving them in collaborative parenting, and training foster parents to be trauma-informed.[109]
Housing authorities are also becoming trauma-informed. Supportive housing can sometimes recreate control and power dynamics associated with clients' early trauma.[112] This can be reduced through trauma-informed practices, such as training staff to be respectful of clients' space by scheduling appointments and not letting themselves into clients' private spaces, and also understanding that an aggressive response may be trauma-related coping strategies.[112] Up to 50% of people with housing insecurity experienced at least four ACEs.[113]
A study in the UK looked at the views of young people exposed to ACEs on what support they needed from social services. The study grouped the findings into three categories: emotional support, practical support and service delivery. Emotional support included interacting with other young people for support and a sense solidarity, and supportive relationships with adults that are based on empathy, active listening and non-judgement. Practical support meant information about the available services, practical advice about everyday challenges and respite from these challenges through recreation. Young people expected service delivery to be continuous and dependable, and they needed flexibility and control over the support processes.[114][115] The needs of young people with ACEs were found not to match the types of support they are offered.[116]
Health care services
Screening for or talking about ACEs with parents and children can help to foster healthy physical and psychological development and can help doctors understand the circumstances that children and their parents are facing. By screening for ACEs in children, pediatric doctors and nurses can better understand behavioral problems. Some doctors have questioned whether some behaviors resulting in attention deficit hyperactivity disorder (ADHD) diagnoses are in fact reactions to trauma. Children who have experienced four or more ACEs are three times as likely to take ADHD medication when compared with children with less than four ACEs.[117] Screening parents for their ACEs allows doctors to provide the appropriate support to parents who have experienced trauma, helping them to build resilience, foster attachment with their children, and prevent a family cycle of ACEs.[118][119]
For people whose adverse childhood experiences were of abuse or neglect cognitive behavioural therapy has been studied and shown to be effective.[120]
Public health
Objections to screening for ACEs include the lack of randomized controlled trials that show that such measures can be used to actually improve health outcomes, the scale collapses items and has limited item coverage, there are no standard protocols for how to use the information gathered, and that revisiting negative childhood experiences could be emotionally traumatic.[121][122] Other obstacles to adoption include that the technique is not taught in medical schools, is not billable, and the nature of the conversation makes some doctors personally uncomfortable.[121] Some public health centers see ACEs as an important way (especially for mothers and children)[123] to target health interventions for individuals during sensitive periods of development.
Resilience and resources
Resilience is the ability to adapt or cope in the face of significant adversity and threats such as health problems, stress experienced in the workplace or home.[124] Resiliency can moderate the relationship of the effects of ACEs and health problem in adulthood.[125][33] Being able use emotion regulation resources such as cognitive reappraisal and mindfulness people are able to protect themselves from the potential negative effects of stressors. These skills can be taught to people but people living with ACEs score lower on measures of resilience and emotion regulation.[33][126]
Resilience and access to other resources are protective factors against the effects of exposure to ACEs.[87][127][128] Increasing resilience in children can help provide a buffer for those who have been exposed to trauma and have a higher ACE score.[33] People and children who have fostered resiliency have the skills and abilities to embrace behaviors that can foster growth.[129] In childhood, resiliency and attachment security can be fostered from having a caring adult in a child's life.[130][131]
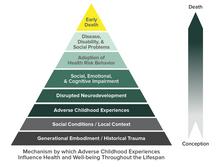
Adverse childhood experiences study
The Adverse Childhood Experiences (ACE) Study was a collaborative effort between Kaiser Permanente (San Diego, CA) and the Centers for Disease Control and Prevention (Atlanta, GA) designed to examine the long-term relationship between adverse childhood experiences (ACEs) and a variety of health behaviours and health outcomes in adulthood. An underlying thesis of the ACE Study is that stressful or traumatic childhood experiences have negative neurodevelopmental impacts that persist over the lifespan and that increase the risk of a variety of health and social problems.[77][1]
The ACE Study was based at Kaiser Permanente's San Diego Health Appraisal Clinic, a primary care clinic where each year more than 50,000 adult members of the Kaiser Permanente Health Maintenance Organization receive an annual, standardized, biopsychosocial medical examination.[132] Each member who visits the Health Appraisal Clinic completes a standardized medical questionnaire.[77] The medical history is completed by a health care provider who also performs a general physical examination and reviews laboratory test results with the patient.[77] Appointments for most members are obtained by self-referral with 20% referred by their health care provider.[77] A review of Kaiser Permanente members aged 25 years or older in San Diego and continuously enrolled between 1992 and 1995 revealed that 81% of those members had been evaluated at the Health Appraisal Clinic.[77] All Kaiser members who completed medical examinations at the Health Appraisal Clinic between August and November of 1995, between January and March of 1996 (Wave I: 13,494 persons), and between April and October of 1997 (Wave II: 13,330 persons) were eligible to participate in the ACE Study.[133] Within two weeks after a member's visit to the Health Appraisal Clinic, a Study questionnaire was mailed asking questions about health behaviours and adverse childhood experiences. A total of 17,421 (68%) persons responded; 84 persons had incomplete information on race and educational attainment leaving 17,337 persons available in the baseline cohort.[133]
In the 1980s, the dropout rate of participants at Kaiser Permanente's obesity clinic in San Diego, California, was about 50%; despite all of the dropouts successfully losing weight under the program.[134] Vincent Felitti, head of Kaiser Permanente's Department of Preventive Medicine in San Diego, conducted interviews with people who had left the program, and discovered that a majority of 286 people he interviewed had experienced childhood sexual abuse. The interview findings suggested to Felitti that weight gain might be a coping mechanism for depression, anxiety, and fear.[134]
Felitti and Robert Anda from the
![]() This article incorporates text from this source, which is by David W Brown, Robert F Anda, Vincent J Felitti, Valerie J Edwards, Ann Marie Malarcher, Janet B Croft, and Wayne H Giles available under the CC BY 2.0 license.
This article incorporates text from this source, which is by David W Brown, Robert F Anda, Vincent J Felitti, Valerie J Edwards, Ann Marie Malarcher, Janet B Croft, and Wayne H Giles available under the CC BY 2.0 license.
Findings
According to the United States' Substance Abuse and Mental Health Services Administration, the ACE study found that:
- Adverse childhood experiences are common. For example, 28% of study participants reported physical abuse and 21% reported sexual abuse. Many also reported experiencing a divorce or parental separation, or having a parent with a mental and/or substance use disorder.[141]
- Adverse childhood experiences often occur together. Almost 40% of the original sample reported two or more ACEs and 12.5% experienced four or more. Because ACEs occur in clusters, many subsequent studies have examined the cumulative effects of ACEs rather than the individual effects of each.[141]
- Adverse childhood experiences have a comorbid, or co-occurring.[141]
About two-thirds of individuals reported at least one adverse childhood experience; 87% of individuals who reported one ACE reported at least one additional ACE. [143] Compared to an ACE score of zero, having four adverse childhood experiences was associated with a seven-fold (700%) increase in alcoholism, a doubling of risk of being diagnosed with cancer, and a four-fold increase in emphysema; an ACE score above six was associated with a 30-fold (3000%) increase in attempted suicide.
The ACE study's results suggest that maltreatment and household dysfunction in childhood contribute to health problems decades later. These include chronic diseases—such as heart disease, cancer, stroke, and diabetes—that are the most common causes of death and disability in the United States.[144] These findings are important because they provided a link between the effects of child maltreatment and negative effects later in life which had not been established as clearly before this study.
Subsequent surveys
The ACE Study has produced more than 50 articles that look at the prevalence and consequences of ACEs.[145][146] It has been influential in several areas. Subsequent studies have confirmed the high frequency of adverse childhood experiences.[147]
The original study questions have been used to develop a 10-item screening questionnaire.[148][149] Numerous subsequent surveys have confirmed that adverse childhood experiences are frequent.
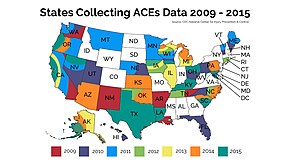
The Behavioral Risk Factor Surveillance System (BRFSS) which is run by the CDC,[150] is an annual survey conducted in waves by groups of individual state and territory health departments. An expanded ACE survey instrument was included in several states found each state.[148] Adverse childhood experiences were even more frequent in studies in urban Philadelphia[151] and in a survey of young mothers (mostly younger than 19).[152] Surveys of adverse childhood experiences have been conducted in multiple EU member countries.[153][154][155]
See also
- Adverse childhood experiences among Hispanic and Latino Americans
- Adverse Childhood Experiences International Questionnaire
- Stress in early childhood
- Social determinants of health
- Verbal abuse
References
- ^ PMID 20085623.
- S2CID 14102617.
- S2CID 25568605.
- S2CID 22071180.
- S2CID 251774877.
- S2CID 205216619.
- S2CID 3217580.
- PMID 20394691.
- ^ a b Asmussen K, Fischer F, Drayton E, McBride T (February 2020). Adverse childhood experiences. What we know, what we don't know, and what should happen next (PDF) (Report). Early Intervention Foundation m.
- ^ "About the CDC-Kaiser ACE Study". Centers for Disease Control and Prevention. 2022-03-17. Retrieved 2022-07-14.
- ^ PMID 21160456.
- PMID 32907569.
- ^ Matilda A, Angela D (September 2015). The Impact of Adverse Experiences in the Home on Children and Young People (PDF) (Report). UCL Institute of Health Equity.
- ^ Krug et al., "World report on violence and health" Archived 2015-08-22 at the Wayback Machine, World Health Organization, 2002.
- S2CID 30813632.
- JSTOR 350477.
- PMID 6686471.
- PMID 31372522.
- S2CID 535692.
- PMID 25972726.
- ^ "The Science of ACEs & Toxic Stress". ACEs Aware. Retrieved 2021-10-16.
- ^ PMID 16311898.
- S2CID 3840754.
- ^ Teicher MH. "Windows of Vulnerability: Understanding how early stress alters trajectories of brain development and sets the stage for the emergence of mental disorders" (PDF). The Balanced Mind. Retrieved 30 March 2014.
- ^ S2CID 205937864.
- ^ Sorrow A (May 30, 2013). "Study uncovers cost of resiliency in kids". medicalxpress.com. Retrieved 30 March 2014.
- PMID 24342859.
- PMID 22018084.
- PMID 20192799.
- PMID 27568065.
- S2CID 13879564.
- S2CID 246827058.
- ^ PMID 35053652.
- S2CID 247926110.
- ^ Allphin M (2020-01-01). "A Meta-analysis on Non-Cognitive Predictors of College Student Academic Performance". Williams Honors College, Honors Research Projects.
- S2CID 238254022.
- ^ S2CID 229175067.
- S2CID 245856379.
- PMID 35742178.
- PMID 35105582.
- ^ "Children and Mental Health: Is This Just a Stage?". National Institute of Mental Health (NIMH). Retrieved 2022-11-17.
- PMID 30233435.
- ^ S2CID 212656815.
- PMID 32839328.
- PMID 32848947.
- S2CID 39417214.
- PMID 30123142.
- S2CID 12012982.
- PMID 26831814.
- PMID 23247614.
- S2CID 27336625.
- PMID 31697656.
- PMID 34756168.
- PMID 31890957.
- S2CID 201965787.
- ^ S2CID 3217580.
- S2CID 237508856.
- S2CID 245907315.
- PMID 33506595.
- ^ S2CID 219123694.
- PMID 31990910.
- PMID 26500379.
- PMID 32128046.
- S2CID 240525653.
- ^ S2CID 234361307.
- PMID 33722874.
- PMID 31446402.
- S2CID 25651656.
- PMID 21037215.
- PMID 25306195.
- S2CID 237092920.
- PMID 28003143.
- S2CID 206255564.
- S2CID 201786187.
- PMID 33734795.
- S2CID 201644851.
- ^ PMID 9635069.
- . Retrieved 10 December 2021.
- S2CID 212831040.
- S2CID 214395921.
- S2CID 213941455.
- S2CID 247643462.
- PMID 31758184.
- S2CID 214232764.
- S2CID 247835374.
- PMID 35600513.
- ^ PMID 30232110.
- ^ PMID 31486086.
- ^ Stevens JE (25 September 2012). "Community Projects". ACEs Connection.
- ^ "PEACE4TARPON Trauma Informed Community Initiative". 30 March 2014.
- ^ Stevens JE (13 February 2012). "Tarpon Springs, FL, may be first trauma-informed city in U.S." ACEs Too High.
- ^ S2CID 4717363.
- ^ a b Plumb JL, Bush KA, Kersevich SE (2016). "Trauma-Sensitive Schools: An Evidence Based Approach". School Social Work Journal. 40 (2): 37–60.
- ^ Stevens JE (28 February 2012). "Spokane, WA, students' trauma prompts search for solutions". ACEs Too High.
- ^ Stevens JE (31 May 2012). "Massachusetts, Washington State lead U.S. trauma-sensitive school movement". ACEs Too High.
- ^ Blodgett C (2013). "A Review of Community Efforts to Mitigate and Prevent Adverse Childhood Experiences and Trauma" (PDF). Washington State University Health Education Center: Spokane, WA.
- ^ National Child Traumatic Stress Network, Schools Committee. (2017). "Creating, Supporting, and Sustaining Trauma-Informed Schools: A System Framework" (PDF). Los Angeles, CA and Durham, NC: National Center for Child Traumatic Stress.
- S2CID 146359339.
- ^ "Sex Between Students & Professors". Retrieved 25 November 2016.
- ^ "Has Media Ignored Sex Abuse In School?". www.cbsnews.com. Archived from the original on 30 October 2013. Retrieved January 15, 2009.[title missing]
- ^ S2CID 234852891.
- ^ Allen, LaRue; Kelly, Bridget B.; Success, Committee on the Science of Children Birth to Age 8: Deepening and Broadening the Foundation for; Board on Children, Youth; Medicine, Institute of; Council, National Research (23 July 2015). Child Development and Early Learning. National Academies Press (US). Retrieved 5 December 2022.
{{cite book}}: CS1 maint: numeric names: authors list (link) - ^ S2CID 222319153.
- ^ S2CID 229405882.
- ^ S2CID 74414328.
- ^ S2CID 21779441.
- ^ Guerrero, A; Herman, A; Teutsch, C; Dudovitz, R (2022). "Improving knowledge and attitudes about child trauma among parents and staff in head start programs". Maternal and Child Health Journal: 1–10 – via EBSCOhost.
- S2CID 143651343.
- ^ a b Meister C (July 2012). "Addressing Child Traumatic Stress in Child Welfare" (PDF). Common Ground. XXVI (1): 9.
- ^ "Family-Informed Trauma Treatment Center". 15 July 2014.
- ^ Stevens JE (30 July 2012). "'Starve the beast,' say these cities – but don't cut people off; reduce need for services instead". ACEs Too High.
- ^ a b Bebout R (Winter 2010–2011). "Waiting on the welcome mat: How to be at home with trauma-informed care". camh Cross Currents. Archived from the original on 2016-01-27.
- ^ ACEs 360. "ACEs 360-New York". Archived from the original on 2014-04-08.
{{cite web}}: CS1 maint: numeric names: authors list (link) - S2CID 244103874.
- PMID 32895586.
- ^ Lester S, Lorenc T, et al. (2019). What helps to support people affected by Adverse Childhood Experiences? A Review of Evidence (PDF). EPPI-Centre, Social Science Research Unit, UCL Institute of Education, University College London.
- ^ Ruiz R (7 July 2014). "How Childhood Trauma Could Be Mistaken for ADHD". The Atlantic.
- ^ Stevens JE (29 July 2014). "To prevent childhood trauma, pediatricians screen children and their parents…and sometimes, just parents…for childhood trauma". ACEs Too High.
- ^ American Academy of Pediatrics. "Promoting Children's Health and Resiliency: A Strengthening Families Approach" (PDF). Center for the Study of Social Policy. Archived from the original (PDF) on 2014-09-03.
- PMID 32397975.
- ^ a b "10 Questions Some Doctors Are Afraid to Ask". NPR.org.
- S2CID 209520160.
- ^ Hellerstedt WL (Spring 2013). "Adverse Childhood Experience: Public Health Surveillance Measures". Healthy Generations. pp. 16–19. Archived from the original (PDF) on 27 January 2016.
- PMID 25476960.
- S2CID 6101456.
- S2CID 4539685.
- PMID 25846195.
- PMID 29567455.
- .
- PMID 28335746.
- S2CID 232194137.
- PMID 10553792.
- ^ PMID 11814159.
- ^ a b c Stevens JE (8 October 2012). "The Adverse Childhood Experiences Study — the Largest Public Health Study You Never Heard Of". The Huffington Post.
- ^ "Prevalence of Individual Adverse Childhood Experiences". cdc.gov. Atlanta, Georgia: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Violence Prevention. May 2014. Archived from the original on 4 April 2016.
- ^ a b c Anda RF, Felitti VJ (April 2003). "Origins and Essence of the Study" (PDF). ACE Reporter. Retrieved 25 March 2014.
- ^ "The ACE Pyramid". Atlanta, Georgia: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Violence Prevention. May 2014. Archived from the original on 16 January 2016.
- ^ "About the CDC-Kaiser ACE Study". Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Violence Prevention. Archived from the original on 28 February 2015.
- ^ "Revised ACEs Pyramid" (PDF).
- ^ "American Psychologist Article". American Psychologist.
- ^ a b c "Adverse Childhood Experiences". samhsa.gov. Rockville, Maryland, US: Substance Abuse and Mental Health Services Administration. Archived from the original on 9 October 2016. Retrieved 29 January 2016.
- S2CID 10726299.
- ^ Middlebrooks JS, Audage NC (2008). The Effects of Childhood Stress on Health Across the Lifespan (PDF). Atlanta, Georgia: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Archived from the original (PDF) on 2016-02-05. Retrieved 2016-01-29.
- ISBN 978-9241594363.)
{{cite book}}: CS1 maint: location missing publisher (link - S2CID 201653078.
- ^ "Publications by Health Outcome". cdc.gov. Atlanta, Georgia: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Violence Prevention. May 2014. Archived from the original on 6 April 2016.
- S2CID 249114918.
- ^ PMID 21160456.
- ^ Anda R (2007). "Finding Your ACE Score" (PDF). Acestudy.org. Archived from the original (PDF) on 1 April 2016.
- ^ Gudmunson CG, Ryherd LM, Bougher K, Downey JC, Zhang D, et al. (Central Iowa ACEs Steering Committee). "Adverse Childhood Experiences in Iowa: A New Way of Understanding Lifelong Health: Findings From the 2012 Behavioral Risk Factor Surveillance System" (PDF).
- ^ "The Philadelphia Urban ACE Study". 2013. Retrieved 29 March 2014.
- ^ Stevens JE (November 2, 2012). "Survey finds teen, young mothers using Crittenton services have alarmingly high ACE scores". ACEs Too High!. Retrieved 29 March 2014.
- ^ Baban A, Cosma A, Balazsi R, Sethi D, Olsavszky V (2013). "Survey of Adverse Childhood Experiences among Romanian university students" (PDF). World Health Organization.
- ^ "Adverse childhood experiences survey among young people in the Czech Republic". World Health Organization. December 23, 2012. Retrieved 29 March 2014.
- ^ Raleva M, Jordanova Peshevska D, Sethi D (2013). "Survey of Adverse Childhood Experiences Among Young People in the Former Yugoslav Republic of Macedonia" (PDF). World Health Organization. Retrieved 29 March 2014.
Further reading
External links
- Adverse Childhood Experiences Resources Centers for Disease Control and Prevention
- ACEs and Toxic Stress FAQ, Harvard Center on the Developing Child
- Veto Violence
