Afamelanotide
This article may have been created or edited in return for undisclosed payments, a violation of Wikipedia's terms of use. It may require cleanup to comply with Wikipedia's content policies, particularly neutral point of view. (July 2018) |
This article's tone or style may not reflect the encyclopedic tone used on Wikipedia. (January 2020) |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˌæfəmɛˈlænoʊtaɪd/ ⓘ |
| Trade names | Scenesse |
| Other names | [Nle4,D-Phe7]α-MSH; NDP-α-MSH; NDP-MSH; Melanotan; Melanotan-1; Melanotan I; EPT1647; CUV1647; |
| AHFS/Drugs.com | Monograph |
| License data |
|
| Pregnancy category |
|
Subcutaneous | |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Elimination half-life | 30 minutes[3] |
| Identifiers | |
| |
JSmol) | |
| |
| |
| | |
Afamelanotide, sold under the brand name Scenesse, is a medication used to prevent phototoxicity and to reduce pain from light exposure for people with
The US Food and Drug Administration (FDA) considers it to be a first-in-class medication.[5]
Medical uses
In the European Union, afamelanotide is
In the United States, afamelanotide is
Adverse effects
Very common adverse effects include nausea and headache (may affect more than 10% of people). Common adverse effects include injection site reactions, back pain, upper respiratory tract infections, melanocyte naevus, decreased appetite, migraine, dizziness, weakness, fatigue, lethargy, sleepiness, feeling hot, stomach pain, diarrhea, vomiting, flushing and red skin, development of warts, spots and freckles and itchy skin (between 1% and 10% of people). Uncommon and rare adverse effects include cystitis, folliculitis, gastrointestinal infections, hypersensitivity reactions, changes in appetite, depression, insomnia, balance disorders, lethargy, restless leg syndrome, syncope, photophobia, presbyopia, tinnitus, confusion, palpitations, hypertension, hypercholesterolaemia and weight gain.[3]
Pharmacology
Afamelanotide is a synthetic
It has a short half-life of approximately 30 minutes. After administration with implantation into the skin, the majority of the drug is released within two days, with 90% released by the fifth day. By the tenth day, no drug is detectable in plasma.[3]
Drug distribution, metabolism and excretion were not understood as of 2017.[3]
Chemistry
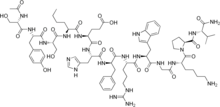
Afamelanotide has the
It is also known as [Nle4,D-Phe7]-α-MSH, which is abbreviated to NDP-MSH or NDP-α-MSH.
Afamelanotide is the international nonproprietary name.[6]
History
α-MSH was first isolated in the 1950s and its primary structure determined. By the 1960s, its role in promoting melanin diffusion was understood.[7]
In the 1980s, the University of Arizona synthesised more potent analogs of a-MSH, including afamelanotide. Afamelanotide was initially named melano-tan (or melanotan-I) due to its ability to tan skin with minimal sun exposure. Later, melanotan-II was synthesised.[8][9][10][11]
Following initial development at the University of Arizona as a sunless tanning agent, the Australian company Clinuvel conducted further clinical trials in that and other indications, and brought the drug to market in the European Union, the United States, and Australia.
To pursue the tanning agent, melanotan-I was licensed by Competitive Technologies, a technology transfer company operating on behalf of University of Arizona, to an Australian startup called Epitan,[12][11] which changed its name to Clinuvel in 2006.[13]
Early clinical trials showed that the peptide had to be injected about ten times a day due to its short half-life, so the company collaborated with Southern Research in the US to develop a depot formulation that would be injected under the skin, and release the peptide slowly. This was done by 2004.[12]
As of 2010, afamelanotide was in Phase III trials for
In May 2010, the Italian Medicines Agency (AIFA, or Agenzia Italiana del Farmaco) approved afamelanotide as a treatment for erythropoietic protoporphyria.[15]
In January 2015, afamelanotide was approved by the European Medicines Agency (EMA) for the treatment of phototoxicity in people with erythropoietic protoporphyria.[3]
There were three trials that evaluated afamelanotide in those with erythropoietic protoporphyria.[4]
In Trial 1, subjects received afamelanotide or vehicle implant every two months and were followed for 180 days.[4] Subjects recorded every day the number of hours spent in direct sunlight and whether they experienced any phototoxic pain that day.[4] The trial measured the total number of hours over 180 days spent in direct sunlight between 10 am and 6 pm on days with no pain.[4]
In Trial 2, subjects received afamelanotide or vehicle implants every two months and were followed for 270 days.[4] Subjects daily recorded the number of hours spent outdoors as well as whether "most of the day" was spent in direct sunlight, shade, or a combination of both, and whether they experienced any phototoxic pain that day.[4] The trial measured the total number of hours over 270 days spent outdoors between 10 am and 3 pm on days with no pain for which "most of the day" was spent in direct sunlight.[4]
In Trial 3, subjects were randomized to receive a total of three afamelanotide or vehicle implants administered subcutaneously every two months and were followed for 180 days.[4] Data from this trial were used primarily for assessment of side effects.[4]
The FDA approved afamelanotide based on evidence from three clinical trials (Trial 1/ NCT 01605136, Trial 2/ NCT00979745 and Trial 3/ NCT01097044) of 244 adults, 18–74 years of age with erythropoietic protoporphyria.[4] The trials were conducted at 22 sites in the US and Europe.[4]
In October 2019, afamelanotide was approved by the US Food and Drug Administration (FDA) as a medicine to reduce pain caused by light exposure (particularly sunlight) as experienced by people with erythropoietic protoporphyria.[16][4]
Society and culture
Usage in general public
A number of products are sold online and in gyms and beauty salons as "melanotan" or "melanotan-1" which discuss afamelanotide in their marketing.[17][18][19]
Without a prescription, these drugs are not legally sold in many jurisdictions and are potentially dangerous.[20][21][22][23]
Starting in 2007, health agencies in various countries began issuing warnings against their use.[24][25][26][27][28][29]
References
- ^ a b c d e "Scenesse- afamelanotide implant". DailyMed. U.S. National Library of Medicine. 15 May 2023. Archived from the original on 25 July 2022. Retrieved 15 June 2023.
- ^ a b c "Scenesse EPAR". European Medicines Agency (EMA). 17 September 2018. Archived from the original on 19 November 2019. Retrieved 18 November 2019.
- ^ a b c d e f g h "Scenesse: Summary of Product Characteristics" (PDF). European Medicines Agency (EMA). 27 January 2016. Archived (PDF) from the original on 6 April 2017. Retrieved 6 April 2017.
- ^ a b c d e f g h i j k l m "Drug Trials Snapshots: Scenesse". U.S. Food and Drug Administration (FDA). 8 October 2019. Archived from the original on 13 August 2020. Retrieved 26 January 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "New Drug Therapy Approvals 2019". U.S. Food and Drug Administration. 31 December 2019. Archived from the original on 16 September 2020. Retrieved 15 September 2020.
- ^ "International Nonproprietary Names for Pharmaceutical Substances (INN)" (PDF). World Health Organization (WHO). 2009. Archived (PDF) from the original on 14 April 2020. Retrieved 2 March 2009.
- S2CID 11465789.
- PMID 6777774.
- ^ Lan EL (1992). Preformulation studies of melanotan-II (PDF) (Ph.D. thesis). University of Arizona. Archived (PDF) from the original on 16 April 2021. Retrieved 16 April 2021.
- PMID 2555512.
- ^ S2CID 21025287.
- ^ a b "EpiTan focuses on Melanotan, a potential blockbuster". The Pharma Letter. 1 November 2004. Archived from the original on 30 July 2018. Retrieved 6 April 2017.
- ^ "Epitan changes name to Clinuvel, announces new clinical program". LabOnline. 27 February 2006. Archived from the original on 2 December 2020. Retrieved 6 April 2017.
- ^ a b Dean T (3 May 2010). "Biotechnology profile: Bright future for Clinuvel (ASX:CUV)". Australian Life Scientist. Archived from the original on 6 April 2017.
- ^ "Gazzetta Ufficiale: Sommario". Agenzia Nazionale Stampa Associata. 2010. Archived from the original on 29 February 2012. Retrieved 17 May 2010.
- ^ "FDA approves first treatment to increase pain-free light exposure in patients with a rare disorder" (Press release). 8 October 2019. Archived from the original on 9 October 2019.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ "Believe It Or Not 'Tanorexia' A Very Real Problem". WCBS-TV, CBS. 20 May 2009. Archived from the original on 21 May 2009. Retrieved 23 July 2009.
- ^ "Fools Gold". Cosmopolitan (Australia). 14 June 2009. Archived from the original on 12 September 2009. Retrieved 25 July 2009.
- ^ Madrigal A (29 January 2009). "Suntan Drug Greenlighted for Trials". Wired. Archived from the original on 5 May 2009. Retrieved 11 April 2009.
- ^ Betts M (31 October 2009). "Tanning drug a health risk". Herald Sun. Archived from the original on 29 December 2010. Retrieved 31 October 2009.
- S2CID 8203334.
- S2CID 27838904.
- ^ "Risky tan jab warnings 'ignored'". BBC News Online. 18 February 2009. Archived from the original on 21 February 2009. Retrieved 4 March 2009.
- ^ "Warning against the product Melanotan". Danish Medicines Agency. 2008. Retrieved 11 August 2008.
- ^ ""Tan jab" is an unlicensed medicine and may not be safe" (Press release). Medicines and Healthcare products Regulatory Agency (MHRA). 2008. Archived from the original on 5 December 2014. Retrieved 17 November 2008.
- ^ "US Lab Research Inc Warning letter". U.S. Food and Drug Administration (FDA). 29 January 2009. Archived from the original on 10 July 2009. Retrieved 23 July 2009.
- Irish Medicines Board. 2009. Archivedfrom the original on 1 August 2013. Retrieved 2 February 2009.
- ^ "Legemiddelverket advarer mot bruk av Melanotan" [The Norwegian Medicines Agency warns against the use of Melanotan] (in Norwegian). Norwegian Medicines Agency. 13 December 2007. Archived from the original on 17 April 2009. Retrieved 11 March 2009.
- Norwegian Medicines Agency. 23 January 2009. Archivedfrom the original on 17 April 2009. Retrieved 11 March 2009.
