Alcoholic hepatitis
| Alcoholic hepatitis | |
|---|---|
histopathologic finding associated with alcoholic hepatitis. H&E stain. | |
| Specialty | Gastroenterology |
| Complications | Cirrhosis, Kidney failure, Confusion, drowsiness and slurred speech (hepatic encephalopathy), Ascites, Enlarged veins (varices).[1] |
| Risk factors | Sex, Obesity, Genetic factors, Race and ethnicity, Binge drinking.[1] |
Alcoholic hepatitis is
Signs and symptoms
Alcoholic hepatitis is characterized by a number of symptoms, which may include feeling unwell, enlargement of the liver, development of fluid in the abdomen (ascites), and modest elevation of liver enzyme levels (as determined by liver function tests).[4] It may also present with Hepatic encephalopathy (brain dysfunction due to liver failure) causing symptoms such as confusion, decreased levels of consciousness, or asterixis,[5] (a characteristic flapping movement when the wrist is extended indicative of hepatic encephalopathy). Severe cases are characterized by profound jaundice, obtundation (ranging from drowsiness to unconsciousness), and progressive critical illness; the mortality rate is 50% within 30 days of onset despite best care.[3]
Alcoholic hepatitis is distinct from cirrhosis caused by long-term alcohol consumption. Alcoholic hepatitis can occur in patients with chronic alcoholic liver disease and alcoholic cirrhosis. Alcoholic hepatitis by itself does not lead to cirrhosis, but cirrhosis is more common in patients with long term alcohol consumption.[6] Some alcoholics develop acute hepatitis as an inflammatory reaction to the cells affected by fatty change.[6] This is not directly related to the dose of alcohol. Some people seem more prone to this reaction than others. This inflammatory reaction to the fatty change is called alcoholic steatohepatitis and the inflammation probably predisposes to liver fibrosis by activating hepatic stellate cells to produce collagen.[6]

Pathophysiology
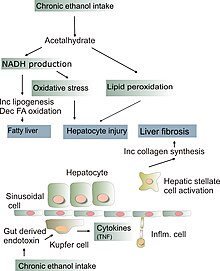
The pathological mechanisms in alcoholic hepatitis are incompletely understood but a combination of direct
Alcohol is also directly damaging to liver cells. Alcohol is metabolized to
The chronic inflammation seen in alcoholic hepatitis leads to a distinctive fibrotic response, with fibrogenic cell type activation. This occurs via an increased extracellular matrix deposition around hepatocytes and sinusoidal cells which causes a peri-cellular fibrosis known as "chickenwire fibrosis".[7] This peri-cellular chickenwire fibrosis leads to portal hypertension or an elevated blood pressure in the portal veins that drain blood from the intestines to the liver.[7] This causes many of the sequelae of chronic liver disease including esophageal varices (with associated variceal bleeding), ascites and splenomegaly.
The chronic inflammation seen in alcoholic hepatitis also leads to impaired hepatocyte differentiation, impairments in hepatocyte regeneration and hepatocyte de-differentiation into
Due to the release of
Some signs and pathological changes in liver histology include:
- hepatocytes. This sign is not limited to alcoholic liver disease, but is often characteristic.[6]
- protein; normally these proteins are exported into the bloodstream. Accompanied with ballooning, there is necrotic damage. The swelling is capable of blocking nearby biliary ducts, leading to diffuse cholestasis.[6]
- Kupffer cells, although in the setting of inflammation they become overloaded, allowing other white cells to spill into the parenchyma. These cells are particularly attracted to hepatocytes with Mallory bodies.[6]
If chronic liver disease is also present:
Epidemiology
- Alcoholic hepatitis occurs in approximately 1/3 of chronic alcohol drinkers.[9]
- 10-20% of patients with alcoholic hepatitis progress to alcoholic liver cirrhosis every year.[10]
- Patients with liver cirrhosis develop liver cancer at a rate of 1.5% per year.[11]
- In total, 70% of those with alcoholic hepatitis will go on to develop alcoholic liver cirrhosis in their lifetimes.[10]
- Infection risk is elevated in patients with alcoholic hepatitis (12–26%). It increases even higher with use of corticosteroids (50%)[12] when compared with the general population.
- Untreated alcoholic hepatitis mortality in one month of presentation may be as high as 40-50%.[4]
Diagnosis
The diagnosis is made in a patient with history of significant alcohol intake who develops worsening
Management
- Abstinence: Stopping further alcohol consumption is the number one factor for recovery in patients with alcoholic hepatitis.[16]
- Nutrition Supplementation: Protein and calorie deficiencies are seen frequently in patients with alcoholic hepatitis, and it negatively affects their outcomes. Improved nutrition has been shown to improve liver function and reduce incidences encephalopathy and infections.[4]
- Corticosteroids: These guidelines suggest that patients with a modified Maddrey's discriminant function score > 32 or hepatic encephalopathy should be considered for treatment with prednisolone 40 mg daily for four weeks followed by a taper.[15] Models such as the Lille Model can be used to monitor for improvement or to consider alternative treatment.
- Pentoxifylline: Systematic reviews comparing the treatment of pentoxifylline with corticosteroids show there is no benefit to treatment with pentoxifylline[4] Potential for combined therapy: A large prospective study of over 1000 patients investigated whether prednisolone and pentoxifylline produced benefits when used alone or in combination.[17] Pentoxifylline did not improve survival alone or in combination. Prednisolone gave a small reduction in mortality at 28 days but this did not reach significance, and there were no improvements in outcomes at 90 days or 1 year.[4]
- Intravenous N-acetylcysteine: When used in conjunction with corticosteroids, improves survival at 28 days by decreasing rates of infection and hepatorenal syndrome.[4]
- Liver Transplantation: Early liver transplantation is ideal and helps to save lives.[18] However, most transplant providers in the United States require a period of alcohol abstinence (typically six months) prior to transplant, but the ethics and science behind this are controversial.[18]
Prognosis
Females are more susceptible to alcohol-associated liver injury and are therefore at higher risk of alcohol-associated hepatitis.[7] Certain genetic variations in the PNPLA3-encoding gene, which codes for an enzyme involved in triglyceride metabolism in adipose tissue are thought to influence disease severity.[7] Other factors in alcoholic hepatitis associated with a poor prognosis include concomitant hepatic encephalopathy and acute kidney injury.[7]
See also
References
- ^ a b "Alcoholic hepatitis". mayoclinic.org. Mayo Clinic. Retrieved June 5, 2022.
- ^ "Alcoholic liver disease: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2 January 2017.
- ^ S2CID 53873388.
- ^ PMID 27254289.
- PMID 29624860.
- ^ ISBN 0-7216-7335-X.
- ^ S2CID 255251817.
- PMC 10666984.
- PMID 14745311.
- ^ S2CID 43829150. Archived from the original(PDF) on 2018-07-19. Retrieved 2020-03-15.
- S2CID 25687227.
- PMID 19445945.
- S2CID 23116073.
- PMID 35426628.
- ^ S2CID 1439776.
- PMID 28459138.
- S2CID 205097413.
- ^ PMID 29389821.
