Allodynia
| Allodynia | |
|---|---|
 | |
| Specialty | Neurology |
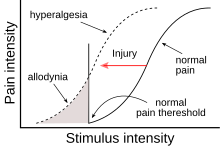
Allodynia is a condition in which
(odúnē) 'pain'.Types
There are different kinds or types of allodynia:
- Mechanical allodynia (also known as tactile allodynia)
- Thermal (hot or cold) allodynia – pain from normally mild skin temperatures in the affected area
- Movement allodynia – pain triggered by normal movement of joints or muscles
Causes
Allodynia is a clinical feature of many painful conditions, such as
Pathophysiology
Cellular level
The cell types involved in
Despite this anatomical separation, mechanoreceptors can influence the output of nociceptors by making connections with the same interneurons, the activation of which can reduce or eliminate the sensation of pain. Another way to modulate the transmission of pain information is via descending fibers from the brain. These fibers act through different interneurons to block the transmission of information from the nociceptors to secondary neurons.[6]
Both of these mechanisms for pain modulation have been implicated in the pathology of allodynia. Several studies suggest that injury to the spinal cord might lead to loss and re-organization of the nociceptors, mechanoreceptors and interneurons, leading to the transmission of pain information by mechanoreceptors[7][8] A different study reports the appearance of descending fibers at the injury site.[9] All of these changes ultimately affect the circuitry inside the spinal cord, and the altered balance of signals probably leads to the intense sensation of pain associated with allodynia.
Different cell types have also been linked to allodynia. For example, there are reports that microglia in the thalamus might contribute to allodynia by changing the properties of the secondary nociceptors.[10] The same effect is achieved in the spinal cord by the recruitment of immune system cells such as monocytes/macrophages and T lymphocytes.[11]
Molecular level
There is a strong body of evidence that the so-called sensitization of the central nervous system contributes to the emergence of allodynia. Sensitization refers to the increased response of neurons following repetitive stimulation. In addition to repeated activity, the increased levels of certain compounds lead to sensitization. The work of many researchers has led to the elucidation of pathways that can result in neuronal sensitization both in the thalamus and dorsal horns. Both pathways depend on the production of chemokines and other molecules important in the inflammatory response.[citation needed]
An important molecule in the thalamus appears to be
The mechanism responsible for sensitization of the central nervous system at the level of the spinal cord is different from the one in the thalamus.
Treatment
Medications
Numerous compounds alleviate the pain from allodynia. Some are specific for certain types of allodynia while others are general. They include:[18]
- Dynamic mechanical allodynia – compounds targeting different ion channels; opioids
- Mexiletine
- Lidocaine (IV/topical)
- Tramadol
- Morphine (IV)
- Alfentanil (IV)
- Ketamine (IV)
- Methylprednisone (intrathecal)
- Adenosine
- Glycine antagonist
- Desipramine
- Venlafaxine
- Pregabalin
- Static mechanical allodynia – sodium channel blockers, opioids
- Lidocaine (IV)
- Alfentanil (IV)
- Adenosine (IV)
- Ketamine (IV)
- Glycine antagonist
- Venlafaxine
- Gabapentin (may also be helpful in cold and dynamic allodynias)
- Cold allodynia
- Lamotrigine
- Lidocaine (IV)
The list of compounds that can be used to treat allodynia is even longer than this. For example, many
Other compounds act on molecules important for the transmission of an action potential from one neuron to another. Examples of these include interfering with receptors for neurotransmitters or the enzymes that remove neurotransmitters not bound to receptors.
Notable people
- Howard Hughes is thought to have had allodynia in his later years; he seldom bathed, wore clothes, or cut his nails and hair, possibly due to the pain these typically normal actions would cause him.[21]
References
- PMID 30725814, retrieved 2020-03-04
- S2CID 1822523.
- S2CID 9163847.
- ^ Landerholm, A. (2010). Neuropathic pain: Somatosensory Functions related to Spontaneous Ongoing Pain, Mechanical Allodynia and Pain Relief. Thesis. Stockholm: Karolinska Institutet http://diss.kib.ki.se/2010/978-91-7457-025-0/thesis.pdf
- S2CID 22387113.
- ISBN 978-0-87893-725-7.
- S2CID 22331115.
- S2CID 28700511.
- S2CID 37627042.
- ^ PMID 17699671.
- ^ S2CID 54415092.
- S2CID 24110610.
- PMID 17204142.
- PMID 17337250.
- PMID 17056121.
- PMID 15788779.
- PMID 16214069.
- PMID 17244104.
- PMID 17651900.
- ISBN 978-0-8493-8667-1.
- ^ Tennant, Forest (July–August 2007). "Howard Hughes & Pseudoaddiction" (PDF). Practical Pain Management. 6 (7). Montclair, New Jersey: PPM Communications, Inc.: 12–29. Archived from the original (PDF) on September 25, 2007. Retrieved January 7, 2011.
