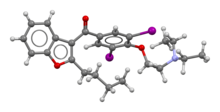
Amiodarone
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /ˌæmiˈoʊdəroʊn/ or /əˈmiːoʊdəˌroʊn/ |
| Trade names | Cordarone, Nexterone, Pacerone, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a687009 |
| License data |
|
| Pregnancy category |
|
intraosseous | |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 20–55% |
| Protein binding | 96% |
| Metabolism | Liver |
| Elimination half-life | 58 d (range 15–142 d) |
| Excretion | Primarily liver and bile |
| Identifiers | |
| |
JSmol) | |
| |
| |
| (verify) | |
Amiodarone is an
Common side effects include feeling tired, tremor, nausea, and constipation.
Amiodarone was first made in 1961 and came into medical use in 1962 for
Medical uses
Amiodarone has been used both in the treatment of acute life-threatening arrhythmias as well as the long-term suppression of arrhythmias.[13] Amiodarone is commonly used to treat different types of abnormal heart rhythms, such as atrial arrhythmias (supraventricular arrhythmias) and ventricular arrhythmias.[13]
Atrial arrhythmias and supraventricular arrhythmias are terms often used interchangeably to refer to abnormal heart rhythms originating from the upper chambers of the heart, known as the atria. These types of arrhythmias include conditions such as atrial fibrillation, atrial flutter, and paroxysmal supraventricular tachycardia (PSVT). They are collectively referred to as supraventricular or atrial arrhythmias because they occur above (supra) the ventricles in the electrical conduction system of the heart.[14]
Ventricular arrhythmias are abnormal heart rhythms that originate in the ventricles, which are the lower chambers of the heart. These arrhythmias can be potentially life-threatening and may disrupt the heart's ability to pump blood effectively.[14]
Amiodarone can be effective in treating conditions like ventricular fibrillation (a rapid and irregular heartbeat), ventricular tachycardia (fast heartbeat originating from the lower chambers), and cardiac arrest due to shock-resistant ventricular fibrillation.[13]
In cases where a patient is experiencing stable ventricular tachycardia, amiodarone may be used to try to stop the episode. However, recent studies suggest that other antiarrhythmic medications like procainamide may be more effective for this purpose.[13][15]
Amiodarone is also commonly used as the first-line therapy for patients who receive implantable cardioverter defibrillator (ICD) shocks due to ventricular arrhythmias. Combining amiodarone with beta-blockers has been shown to reduce the likelihood of experiencing appropriate shocks from an ICD.[13]
Cardiac arrest
Defibrillation is the treatment of choice for ventricular fibrillation and pulseless ventricular tachycardia resulting in cardiac arrest. While amiodarone has been used in shock-refractory cases, evidence of benefit is poor.[5] Amiodarone does not appear to improve survival or positive outcomes in those who had a cardiac arrest.[16]
Ventricular tachycardia
Amiodarone may be used in the treatment of ventricular tachycardia in certain instances.[17] Individuals with hemodynamically unstable ventricular tachycardia should not initially receive amiodarone. These individuals should be cardioverted.
Amiodarone can be used in individuals with hemodynamically stable ventricular tachycardia. In these cases, amiodarone can be used regardless of the individual's underlying heart function and the type of ventricular tachycardia; it can be used in individuals with
Atrial fibrillation
Individuals who have undergone
So-called 'acute onset atrial fibrillation', defined by the North American Society of Pacing and Electrophysiology (NASPE) in 2003, responds well to short-duration treatment with amiodarone.[15][24] This has been demonstrated in seventeen randomized controlled trials, of which five included a placebo arm. The incidence of severe side effects in this group is low.[25][26][27]
The benefit of amiodarone in the treatment of atrial fibrillation in the critical care population has yet to be determined but it may prove to be the agent of choice where the patient is hemodynamically unstable and unsuitable for DC cardioversion.
Contraindications
Women who are
It is contraindicated in individuals with
Individuals with baseline depressed lung function should be monitored closely if amiodarone therapy is to be initiated.
Formulations of amiodarone that contain benzyl alcohol should not be given to neonates, because the benzyl alcohol may cause the potentially fatal "gasping syndrome".[30]
Amiodarone can worsen the cardiac arrhythmia brought on by digitalis toxicity.
Contraindications of amiodarone also include:
- hypersensitivity to amiodarone or any of its components;[13]
- severe hepatic impairment;[13]
- sinus node dysfunction, including severe sinus bradycardia or sinoatrial block, since amiodarone can cause significant bradycardia and sinus nodal arrest;[13]
- second- or third-degree atrioventricular (AV) block, due to its negative chronotropic (affecting the heart rate) and dromotropic (affecting the conductivity) effects on the AV conduction system, unless a pacemaker is implanted;[13]
- thyrotoxicosis that cannot be controlled by conventional means, such as Graves' disease.[13]
There are no specific guidelines for endurance or high-intensity exercise while taking amiodarone. However, since amiodarone may cause bradycardia and QTc prolongation which can affect exercise capacity and increase the risk of arrhythmias during intense exercise, it would generally be advisable for patients taking this medication to consult their healthcare provider before engaging in high-intensity physical activities such as strenuous endurance exercises.[13]
Side effects
At oral doses of 400 mg per day or higher, amiodarone can have serious, varied
Some common side effects include:
- nausea and vomiting;[13]
- taste disturbances (changes in taste perception, often described as a metallic or bitter taste in the mouth);[13]
- photosensitivity of the skin, also known as photodermatitis, where exposure to sunlight or ultraviolet radiation may lead to skin reactions such as rashes or sunburn-like symptoms;[13]
- corneal microdeposits (deposits may accumulate on the cornea over time, resulting in blurred vision or visual halos—bright circles or rings around a light source, such as headlights; still, these corneal deposits typically do not affect vision significantly);[13][34]
- thyroid dysfunction[35] (in approximately 15-20% of patients, amiodarone treatment results in thyroid dysfunction, either amiodarone-induced hypothyroidism or amiodarone-induced thyrotoxicosis; the drug can lead to both hypo- and hyperthyroidism);[31]
- pulmonary toxicity[36][37][38][39] (lung problems such as pulmonary fibrosis or interstitial lung disease may occur rarely but have the potential for serious consequences if left untreated);[7][13]
- liver abnormalities (liver damage, including elevated liver enzymes (AST/ALT) and hepatotoxicity, although severe cases are rare);[13]
- bradycardia and heart block (since it slows down heart rate by affecting the sinus node function and AV conduction system, it can increase the risk of heart block);[13]
- QT Interval prolongation.[13]
Amiodarone can potentially cause renal toxicity, but solid studies on whether amiodarone may be toxic to the kidneys are lacking.[40]
Lung

Side effects of oral amiodarone at doses of 400 mg or higher include various
The most specific test of pulmonary toxicity due to amiodarone is a dramatically decreased
Thyroid
Induced abnormalities in thyroid function are common.[35][32] In approximately 15-20% of patients, amiodarone treatment results in thyroid dysfunction, either amiodarone-induced hypothyroidism or amiodarone-induced thyrotoxicosis.[42][43][31][17] Both under- and overactivity of the thyroid may occur.[32]
Amiodarone is structurally similar to
Thyroid function should be checked at least every six months.[48]
- Hypothyroidism (slowing of the thyroid) occurs frequently; in the SAFE trial, which compared amiodarone with other medications for the treatment of atrial fibrillation, biochemical hypothyroidism (as defined by a TSH level of 4.5–10 mU/L) occurred in 25.8% of the amiodarone-treated group as opposed to 6.6% of the control group (taking placebo or sotalol). Overt hypothyroidism (defined as TSH >10 mU/L) occurred at 5.0% compared to 0.3%; most of these (>90%) were detected within the first six months of amiodarone treatment.[49]
- Amiodarone induced thyrotoxicosis (AIT), can be caused due to the high iodine content in the drug via the Jod-Basedow effect. This is known as Type 1 AIT, and usually occurs in patients with an underlying predisposition to hyperthyroidism such as Graves' disease, within weeks to months after starting amiodarone. Type 1 AIT is usually treated with anti-thyroid drugs or thyroidectomy. Type 2 AIT is caused by a destructive thyroiditis due to a direct toxic effect of amiodarone on thyroid follicular epithelial cells.[42][50] Type 2 AIT can occur even years after starting amiodarone, is usually self-limited and responds to anti-inflammatory treatment such as corticosteroids.[50] In practice, often the type of AIT is undetermined or presumed as mixed with both treatments combined.[50] Thyroid uptake measurements (I-123 or I-131), which are used to differentiate causes of hyperthyroidism, are generally unreliable in patients who have been taking amiodarone. Because of the high iodine content of amiodarone, the thyroid gland is effectively saturated, thus preventing further uptake of isotopes of iodine. However, positive radioactive iodine can be used to rule in type 1AIT .[citation needed]
-
Amiodarone
-
Thyroxine
Eye
Corneal micro-deposits (cornea verticillata,[51] also called vortex or whorl keratopathy) are almost universally present (over 90%) in individuals taking amiodarone longer than 6 months, especially doses greater than 400 mg/day. These deposits typically do not cause any symptoms. About 1 in 10 individuals may complain of a bluish halo. Anterior subcapsular lens deposits are relatively common (50%) in higher doses (greater than 600 mg/day) after 6 months of treatment. Optic neuropathy, nonarteritic anterior ischemic optic neuropathy (N-AION), occurs in 1–2% of people and is not dosage dependent.[52] Bilateral optic disc swelling and mild and reversible visual field defects can also occur.
Loss of eyelashes has been linked to amiodarone use.[53]
Liver
Abnormal
In clinical observations, it has been noted that the administration of amiodarone, even at lower therapeutic doses, has been associated with the development of a condition mimicking alcoholic cirrhosis. This condition, often referred to as pseudo-alcoholic cirrhosis, presents with similar histopathological features to those observed in patients with alcoholic cirrhosis.[55][56] However, this extreme adverse event manifestation—pseudo-alcoholic cirrhosis caused by low dose amiodarone—is very rare.[33]
Skin
Long-term administration of amiodarone (usually more than eighteen months) is associated with a light-sensitive blue-grey discoloration of the skin, sometimes called ceruloderma; such patients should avoid exposure to the sun and use sunscreen that protects against ultraviolet-A and -B. The discoloration will slowly improve upon cessation of the medication, however, the skin color may not return completely.[57]
Pregnancy and breastfeeding
Use during pregnancy may result in a number of problems in the infant including thyroid problems, heart problems, neurological problems, and preterm birth.[58] Use during breastfeeding is generally not recommended though one dose may be okay.[58]
Other
Long-term use of amiodarone has been associated with
Amiodarone is sometimes responsible for epididymitis. Amiodarone accumulates in the head of the organ and can cause unilateral or bilateral inflammation. It tends to resolve if amiodarone is stopped.[60]
Some cases of gynecomastia have been reported in men on amiodarone.[61]
There is a possible association between amiodarone and an increased risk of cancer, especially in males, with a dose-dependent effect.[62]
Drug-drug interactions
The pharmacokinetics of numerous drugs, including many that are commonly administered to individuals with heart disease, are affected by amiodarone.[medical citation needed]
Amiodarone has particularly important interactions with the following drugs:
- class I antiarrhythmics (amiodarone should not be combined with other class I antiarrhythmic drugs, such as disopyramide, flecainide, procainamide, quinidine, etc., due to an increased risk of QTc prolongation and potential arrhythmias);[13]
- beta blockers and calcium channel blockers (combining amiodarone with beta-blockers or calcium channel blockers, such as sotalol, can further slow down heart rate and cause bradycardia or heart block);[13]
- digoxin (amiodarone inhibits a protein called P-glycoprotein (P-gp), which transports digoxin out of cells in the gut, liver, and kidneys, therefore, concurrent use of these medications increases digoxin levels in the body, potentially leading to digoxin toxicity)[13]
- statins (amiodarone can inhibit enzymes in the liver responsible for metabolizing certain statins, such as simvastatin, atorvastatin, etc., therefore interaction elevates plasma concentrations of these statins, increasing the risk of myopathy, that is muscle damage, or rhabdomyolysis, that is severe muscle breakdown);[13]
- international normalized ratio (INR)) measured more frequently. Dose reduction of warfarin is as follows: 40% reduction if the amiodarone dose is 400 mg daily, 35% reduction if the amiodarone dose is 300 mg;mg daily, 30% reduction if the amiodarone dose is 200 mg daily, and 25% reduction if amiodarone dose is 100 mg daily.[medical citation needed] The effect of amiodarone on the warfarin concentrations can be as early as a few days after initiation of treatment; however, the interaction may not peak for up to seven weeks;[medical citation needed]
Amiodarone inhibits the action of the cytochrome P450 isozyme family; such inhibition reduces the clearance of many drugs, including the following:[medical citation needed]
- ciclosporin,
- digoxin,
- flecainide,
- procainamide,
- quinidine,
- sildenafil,
- simvastatin,
- theophylline,
- warfarin.
In 2015, Gilead Sciences warned healthcare providers about people who began taking the hepatitis C drugs ledipasvir/sofosbuvir or sofosbuvir along with amiodarone, who developed abnormally slow heartbeats or died of cardiac arrest.[64]
Metabolism
Amiodarone is extensively metabolized in the liver by CYP3A4, a member of the cytochrome P450 superfamily of enzymes, therefore, amiodarone and can affect the metabolism of numerous other drugs that depend on cytochrome P450, such as digoxin, phenytoin, warfarin, etc.[15][65][66][43]
The major metabolite of amiodarone is desethylamiodarone (DEA), which also has antiarrhythmic properties.[15]
The metabolism of amiodarone is inhibited by grapefruit juice, leading to elevated serum levels of amiodarone.[medical citation needed]
On 8 August 2008, the US Food and Drug Administration (FDA) issued a warning of the risk of rhabdomyolysis, which can lead to kidney failure or death, when simvastatin is used with amiodarone. This interaction is dose-dependent with simvastatin doses exceeding 20 mg. This drug combination, especially with higher doses of simvastatin, should be avoided.[67] Amiodarone is extensively metabolized in the liver. The primary metabolic pathway of amiodarone is by cytochrome P450 (CYP) enzymes, particularly CYP3A4 and CYP2C8.[63][43] The metabolism of amiodaron can be characterized by two phases:
- phase I metabolism, when amiodarone undergoes oxidative processes mainly mediated by CYP3A4 and to a lesser extent by CYP2C8; these reactions result in the formation of several active metabolites, including desethylamiodarone (DEA) and di-desethylamiodarone (DDEA); DEA is the most abundant metabolite and exhibits similar pharmacological effects as amiodarone;[medical citation needed]
- phase II metabolism, when both amiodarone and its major metabolite DEA can undergo conjugation reactions with glucuronic acid;t his process increases water solubility of these compounds for their efficient elimination from the body.[medical citation needed]
Amiodarone has an exceptionally long half-life due to a combination of several factors:[13]
- high lipid solubility, given that amiodarone has high lipid solubility, which allows it to distribute throughout various tissues in the body rapidly; the extensive tissue distribution of amiodarone contributes to a large volume of distribution that leads to slow clearance from plasma compartments;
- extensive tissue binding, so that amiodarone extensively binds to different tissues, including fat deposits, muscles, heart tissue, and other organs; this binding creates reservoirs where drug release can occur slowly over time, resulting in an extended duration of action even after stopping the therapy;
- enterohepatic recycling, meaning that amiodarone undergoes enterohepatic recycling, where it is reabsorbed from the intestines after being excreted into bile, which contributes to its prolonged presence.[68]
Excretion
Excretion is primarily via the liver and the bile duct with almost no elimination via the kidney and it is not dialyzable.[1] Elimination half-life average of 58 days (ranging from 25 to 100 days [Remington: The Science and Practice of Pharmacy 21st edition]) for amiodarone and 36 days for the active metabolite, desethylamiodarone (DEA).[1] There is 10-50% transfer of amiodarone and DEA in the placenta as well as a presence in breast milk.[1] Accumulation of amiodarone and DEA occurs in adipose tissue and highly perfused organs (i.e. liver, lungs),[1] therefore, if an individual was taking amiodarone on a chronic basis if it is stopped it will remain in the system for weeks to months.[1]
Whereas amiodarone is primarily eliminated from the body through hepatic metabolism and biliary excretion, a very small portion of amiodarone and its metabolites are excreted unchanged in urine or feces.[63][43]
The liver plays a significant role in the elimination of amiodarone. After being extensively metabolized by cytochrome P450 enzymes, particularly CYP3A4 and CYP2C8, amiodarone is transported into bile via multidrug-resistant protein 2 (MRP2) transporter. Bile containing amiodarone and its metabolites is then released into the gastrointestinal tract.[medical citation needed]
Some of these compounds can be reabsorbed back into systemic circulation through enterohepatic recirculation, where they may undergo additional rounds of metabolism before eventually being excreted again into bile.[medical citation needed]
Although renal excretion contributes only minimally to the elimination of amiodarone, dose adjustment based on kidney function is generally not necessary. This is because most patients with normal renal function can adequately clear the drug through hepatic metabolism and biliary elimination pathways.[13]
Pharmacology
Amiodarone is categorized as a class III antiarrhythmic agent, and prolongs phase 3 of the cardiac action potential, the repolarization phase where there is normally decreased calcium permeability and increased potassium permeability. It has numerous other effects, however, including actions that are similar to those of antiarrhythmic classes Ia, II, and IV.[medical citation needed]
Amiodarone is a blocker of
Amiodarone slows the conduction rate and prolongs the refractory period of the SA and AV nodes.[70] It also prolongs the refractory periods of the ventricles, bundles of His, and the Purkinje fibers without exhibiting any effects on the conduction rate.[70] Amiodarone has been shown to prolong the myocardial cell action potential duration and refractory period and is a non-competitive β-adrenergic inhibitor.[71]
It also shows
Amiodarone chemically resembles
- potassium channel blockade, since amiodarone blocks potassium channels involved in cardiac repolarization during phase 3 of the action potential, so that this blockade prolongs the duration of cardiac action potentials, resulting in an increased refractory period and decreased excitability;[13]
- sodium channel blockade, characterized by inhibiting sodium ion influx through voltage-gated sodium channels, so that amiodarone reduces the conduction velocity of electrical impulses in cardiac tissue that leads to a slowed heart rate and improved rhythm control;[13]
- calcium channel blockade, by inhibiting L-type calcium channels in myocardial cells, decreasing intracellular calcium concentration during ventricular contraction;[13]
- noncompetitive adrenergic receptor antagonism, meaning that amiodarone has both alpha- and beta-adrenergic receptor antagonistic effects, which help reduce sympathetic stimulation on the heart.[13]
History
The original observation that amiodarone's progenitor molecule,
As a doctoral candidate at Oxford University, Bramah Singh determined that amiodarone and
Based on Singh's work, the Argentinian physician Mauricio Rosenbaum began using amiodarone to treat his patients who have supraventricular and ventricular arrhythmias, with impressive results. Based on papers written by Rosenbaum developing Singh's theories, physicians in the United States began prescribing amiodarone to their patients with potentially life-threatening arrhythmias in the late 1970s.[79][80]
The US Food and Drug Administration (FDA) was reluctant to officially approve the use of amiodarone since initial reports had shown an increased incidence of serious pulmonary side effects of the drug. In the mid-1980s, the European pharmaceutical companies began putting pressure on the FDA to approve amiodarone by threatening to cut the supply to American physicians if it was not approved. In December 1985, amiodarone was approved by the FDA for the treatment of arrhythmias.[2][81]
Name
Amiodarone may be an acronym[
Dosing
Amiodarone is available in oral and intravenous formulations.
Orally, it is available under the brand names Pacerone (produced by Upsher-Smith Laboratories, Inc.) and Cordarone (produced by Wyeth-Ayerst Laboratories).[1][2] It is also available under the brand name Aratac (produced by Alphapharm Pty Ltd) in Australia and New Zealand, and further in Australia under the brands Cardinorm and Rithmik as well as a number of generic brands. Also Arycor in South Africa (Produced by Winthrop Pharmaceuticals.). In South America, it is known as Atlansil and is produced by Roemmers.
In India, amiodarone is marketed (produced by Cipla Pharmaceutical) under the brand name Tachyra. It is also available in intravenous ampules and vials.
The dose of amiodarone administered is tailored to the individual and the dysrhythmia that is being treated. When administered orally, the bioavailability of amiodarone is quite variable. Absorption ranges from 22 to 95%, with better absorption when it is given with food.[15]
References
- ^ a b c d e f g "Pacerone- amiodarone hydrochloride tablet". DailyMed. Archived from the original on 29 December 2022. Retrieved 8 September 2021.
- ^ a b c "Cordarone (amiodarone) tablets, for oral use Initial U.S. Approval: 1985". DailyMed. 30 October 2018. Archived from the original on 29 December 2022. Retrieved 8 September 2021.
- ^ "Nexterone- Amiodarone HCl injection, solution". DailyMed. Archived from the original on 29 December 2022. Retrieved 8 September 2021.
- ^ a b c d e f g h i j k "Amiodarone Hydrochloride". The American Society of Health-System Pharmacists. Archived from the original on 19 September 2016. Retrieved 22 August 2016.
- ^ (PDF) from the original on 5 March 2020. Retrieved 17 December 2019.
- ^ ISBN 978-1-7242-7798-5.
- ^ S2CID 227253264.
- ISBN 978-0-08-086115-9. Archivedfrom the original on 8 September 2017.
- ^ ISBN 978-3-527-60749-5. Archivedfrom the original on 8 September 2017.
- hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- ^ "The Top 300 of 2021". ClinCalc. Archived from the original on 15 January 2024. Retrieved 14 January 2024.
- ^ "Amiodarone - Drug Usage Statistics". ClinCalc. Archived from the original on 18 January 2024. Retrieved 14 January 2024.
- ^ S2CID 212682149.
- ^ PMID 30675928.
- ^ from the original on 5 February 2024. Retrieved 5 February 2024.
- PMID 27434349.
- ^ PMID 36818930.
- ^ Resuscitation Council (UK) Peri-arrest arrhythmias – Tachycardia algorithm Archived 3 January 2016 at the Wayback Machine Retrieved 25 January 2016
- ^ "UpToDate". Archived from the original on 5 February 2024. Retrieved 5 February 2024.
- ^ "Atrial fibrillation after surgery: Common and undertreated?". October 2022. Archived from the original on 5 February 2024. Retrieved 5 February 2024.
- ^ "Amiodarone Reduction in Coronary Heart Trial". Archived from the original on 5 February 2024. Retrieved 5 February 2024.
- S2CID 24714524.
- ^ Neff MJ (April 2005). "Practice Guideline Briefs". American Family Physician. 71 (7): 1434. Archived from the original on 5 February 2024. Retrieved 5 February 2024.
- from the original on 5 February 2024. Retrieved 5 February 2024.
- from the original on 5 February 2024. Retrieved 5 February 2024.
- from the original on 5 February 2024. Retrieved 5 February 2024.
- ^ "Recommendations | Atrial fibrillation: Diagnosis and management | Guidance | NICE". 27 April 2021. Archived from the original on 5 February 2024. Retrieved 5 February 2024.
- ^ PMID 34289899.
- ^ "Critical Care Atrial Fibrillation Evaluation (CAFE)". Archived from the original on 5 February 2024. Retrieved 5 February 2024.
- from the original on 30 August 2012.
- ^ S2CID 262088052.
- ^ a b c d e "Amiodarone". Drugs.com. 18 May 2022. Archived from the original on 25 July 2022. Retrieved 25 July 2022.
- ^ PMID 32368381.
- PMID 31447894.)
{{cite journal}}: CS1 maint: DOI inactive as of March 2024 (link - ^ PMID 37547257.
- PMID 37123694.
- PMID 37249923.
- PMID 36553223.
- PMID 36176494.
- PMID 37743903.
- ^ a b "Amiodarone Side Effects". Drugs.com. 25 April 2021. Archived from the original on 24 February 2016. Retrieved 25 July 2022.
- ^ PMID 19584973.
- ^ NCBI NBK482154.
- PMID 25295624.
- ISBN 978-1-139-48612-5. Archivedfrom the original on 8 September 2017.
- ISSN 1872-3136.
- ISSN 0393-9375.
- PMID 29594056.
- from the original on 9 August 2020. Retrieved 27 August 2020.
- ^ S2CID 226275566.
- PMID 7116220.
- PMID 22385784.
- ISBN 978-93-5025-571-1. Archivedfrom the original on 8 September 2017.
- S2CID 37972060.
- PMID 12615569.
- PMID 16284489.
- S2CID 210333420.
- ^ a b "Amiodarone Pregnancy and Breastfeeding Warnings". Drugs.com. Archived from the original on 15 October 2020. Retrieved 8 December 2021.
- PMID 2989436.
- PMID 12580564.
- ^ [1] Archived 9 July 2009 at the Wayback Machine Gynecomastia: Its features, and when and how to treat it
- S2CID 24144312.
- ^ a b c "Cordarone (amiodarone HCl) tables" (PDF). FDA. 2010. Archived (PDF) from the original on 3 August 2023. Retrieved 22 March 2024.
- ^ West, Stephen. "Gilead Warns After Hepatitis Patient on Heart Drug Dies" Archived 22 March 2017 at the Wayback Machine. Published 21 March 2015.
- ^ "Amiodarone | Deranged Physiology". Archived from the original on 5 December 2023. Retrieved 22 March 2024.
- PMID 2673606.
- ^ "Information on Simvastatin/Amiodarone". Food and Drug Administration. Archived from the original on 21 September 2008. Retrieved 21 September 2008.
- PMID 33658939.
- ^ "Amiodarone". Drugbank. Archived from the original on 23 May 2019. Retrieved 28 May 2019.
- ^ ISBN 978-2-86439-125-8.
- ^ "FDA Drug Label". Archived from the original on 27 March 2017.
- PMID 26973526.
- ISBN 0-07-142280-3.[page needed]
- PMID 18610042.
- PMID 14026835.
- PMID 14020244.
- ^ ISBN 978-1-156-39374-1.
- PMID 5485142.
- PMID 793369.
- PMID 6613843.
- ^ "Drug Approval Package: Cordarone (Amiodarone Hydrochloride) Tablets. NDA #018972". U.S. Food and Drug Administration. Archived from the original on 21 February 2014. Retrieved 6 February 2014.
- ^ "Compound summary for CID 2157". pubchem.ncbi.nil.nih.gov. Archived from the original on 24 March 2016.


