Angiography
This article needs more primary sources. (November 2021) |  |
| Angiography | |
|---|---|
posterior cerebral circulation. | |
| ICD-9-CM | 88.40-88.68 |
| MeSH | D000792 |
| OPS-301 code | 3–60 |
Angiography or arteriography is a
The word itself comes from the Greek words ἀγγεῖον angeion 'vessel' and γράφειν graphein 'to write, record'. The film or image of the blood vessels is called an angiograph, or more commonly an angiogram. Though the word can describe both an arteriogram and a venogram, in everyday usage the terms angiogram and arteriogram are often used synonymously, whereas the term venogram is used more precisely.[1]
The term angiography has been applied to
History
The technique was first developed in 1927 by the
Technique
Depending on the type of angiogram, access to the blood vessels is gained most commonly through the
The X-ray images taken may either be still, displayed on an
After the procedure has been completed, if the femoral technique is applied, the site of arterial entry is either manually compressed, stapled shut, or sutured in order to prevent access-site complications.[5]
Uses
Coronary angiography
One of the most common angiograms performed is to visualize the
Coronary angiography can visualize coronary artery stenosis, or narrowing of the blood vessel. The degree of stenosis can be determined by comparing the width of the lumen of narrowed segments of blood vessel with wider segments of adjacent vessel.[5]
Cerebral angiography
Cerebral angiography provides images of blood vessels in and around the brain to detect abnormalities, including arteriovenous malformations and aneurysms.[6] One common cerebral angiographic procedure is neuro-vascular digital subtraction angiography.[7][8]
Pulmonary angiography
Pulmonary angiography is used to visualise the anatomy of pulmonary vessels.
Peripheral angiography
Angiography is also commonly performed to identify vessels narrowing in patients with leg claudication or cramps, caused by reduced blood flow down the legs and to the feet; in patients with renal stenosis (which commonly causes high blood pressure) and can be used in the head to find and repair stroke. These are all done routinely through the femoral artery, but can also be performed through the brachial or axillary (arm) artery. Any stenoses found may be treated by the use of balloon angioplasty, stenting, or atherectomy.
Fluorescein angiography
Fluorescein angiography is a medical procedure in which a fluorescent dye is injected into the bloodstream. The dye highlights the blood vessels in the back of the eye so they can be photographed. This test is often used to manage eye disorders.[9]
OCT angiography
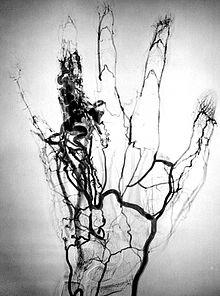
Microangiography
Microangiography is commonly used to visualize tiny blood vessels.
Post mortem CT angiography
Post mortem CT angiography for medicolegal cases is a method initially developed by a virtopsy group. Originating from that project, both watery[11] and oily[12] solutions have been evaluated.
While oily solutions[12] require special deposition equipment to collect waste water, watery[11] solutions seem to be regarded as less problematic. Watery solutions also were documented to enhance post mortem CT tissue differentiation whereas oily solutions were not. Conversely, oily solutions seem to only minimally disturb ensuing toxicological analysis, while watery solutions may significantly impede toxicological analysis, thus requiring blood sample preservation before post mortem CT angiography.[13]
Complications
Angiography is a relatively safe procedure. But it does have some minor and very few major complications. After an angiogram, a sudden shock can cause a little pain at the surgery area, but heart attacks and strokes usually do not occur, as they may in bypass surgery.
Cerebral angiography
Major complications in cerebral angiography such as in
Additional risks
The contrast medium that is used usually produces a sensation of warmth lasting only a few seconds, but may be felt in a greater degree in the area of injection. If the patient is allergic to the contrast medium, much more serious side effects are inevitable; however, with new contrast agents the risk of a severe reaction is less than one in 80,000 examinations. Additionally, damage to blood vessels can occur at the site of puncture/injection, and anywhere along the vessel during passage of the catheter. If digital subtraction angiography is used instead, the risks are considerably reduced because the catheter does not need to be passed as far into the blood vessels; thus lessening the chances of damage or blockage.
Infection
Thrombosis
There are six risk factors causing thrombosis after arterial puncture: low blood pressure, small arterial diameter, multiple puncture tries, long duration of cannulation, administration of vasopressor/inotropic agents,[16] and the usage of catheters with side holes.[17]
See also
- Acoustic angiography
- Angiosarcoma
- Cardiac catheterization
- Computed tomography angiography
- Contrast medium
- Echocardiogram
- Electrocardiogram
- Fluorescein angiography
- Image intensifier
- Interventional radiology
- Intravascular ultrasound
- Intravenous digital subtraction angiography
- Magnetic resonance angiography
- Peripheral artery occlusive disease
References
- ^ G. Timothy Johnson, M.D. (1986-01-23). "Arteriograms, Venograms Are Angiogram Territory". Chicago Tribune. Retrieved 12 September 2011.
- ISBN 9780199687817.
- S2CID 22225524.
- PMID 2912567.
- ^ )
- ISBN 9780191744358. Retrieved 24 August 2022.
- ^ Glick, Yair. "Digital subtraction angiography | Radiology Reference Article | Radiopaedia.org". Radiopaedia. Retrieved 2021-09-29.
- PMID 2334014.
- ^ "Fluorescein Angiography". EMPIRE RETINA CONSULTANTS. Retrieved 22 August 2016.
- PMID 28760677.
- ^ PMID 18430859.
- ^ PMID 17056884.
- PMID 22704555.
- ^ "Angiography – Complications". Health A-Z. NHS Choices. 2009-06-01. Retrieved 2010-03-24.
- PMID 21029949.
- PMID 15354915.
- PMID 32764790.
External links
- RadiologyInfo for patients: Angiography procedures
- Cardiac Catheterization from Angioplasty.Org
- C-Arms types Several types of C-Arms
- Coronary CT angiography by Eugene Lin


