Area postrema
| Area postrema | |
|---|---|
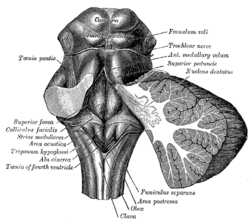 Rhomboid fossa. (Area postrema labeled at bottom center.) | |
 Human caudal brainstem posterior view description (Area postrema is #8) | |
| Details | |
| Part of | Medulla |
| Identifiers | |
| Acronym(s) | AP |
| MeSH | D031608 |
| NeuroNames | 772 |
| NeuroLex ID | birnlex_2636 |
| TA98 | A14.1.04.258 |
| TA2 | 6009 |
| FMA | 72607 |
| Anatomical terms of neuroanatomy | |
The area postrema, a paired structure in the
Structure
The area postrema is a paired protuberance found at the inferoposterior limit of the
The area postrema is considered a

Connections
The area postrema connects to the
Because the area postrema and a specialized region of NTS have permeable capillaries,[2] peptides and other hormonal signals in the blood have direct access to neurons of brain areas with vital roles in the autonomic control of the body.[2][6] As a result, the area postrema is considered a site of integration for various physiological signals in the blood as they enter the central nervous system.[2][3]
Function
Chemoreception
The area postrema, one of the circumventricular organs,[10] detects toxins in the blood and acts as a vomit-inducing center. The area postrema is a critical homeostatic integration center for humoral and neural signals by means of its function as a chemoreceptor trigger zone for vomiting in response to emetic drugs. It is a densely vascularized structure with subregional capillary specializations for high permeability for circulating blood signals, allowing it to detect various chemical messengers in the blood and cerebrospinal fluid.[4][6] Capillary blood flow appears to be uniquely slow in the area postrema, prolonging the contact time for blood-borne hormones to interact with neuronal receptors involved in regulation of blood pressure, body fluids, and emetic responses.[4][8]
Autonomic regulation
The
Clinical significance
Damage
Damage to the area postrema, caused primarily by lesioning or
Effect of dopamine
The area postrema also has a significant role in the discussion of Parkinson's disease. Drugs that treat Parkinson's disease using dopamine have a strong effect on the area postrema. These drugs stimulate dopamine transmission and attempt to normalize motor functions affected by Parkinson's. This works because nerve cells, in particular, in the basal ganglia, which has a crucial role in the regulation of movement and is the primary site for the pathology of Parkinson's, use dopamine as their neurotransmitter and are activated by medications that increase the concentrations of the dopamine or work to stimulate the dopamine receptors. Dopamine also manages to stimulate the area postrema, since this part of the brain contains a high density of dopamine receptors. The area postrema is very sensitive to changes in blood toxicity and senses the presence of poisonous or dangerous substances in the blood. As a defense mechanism, the area postrema induces vomiting to prevent further intoxication. The high density of dopamine receptors in the area postrema makes it very sensitive to the dopamine-enhancing drugs. Stimulation of the dopamine receptors in the area postrema activates these vomiting centers of the brain; this is why nausea is one of the most common side-effects of antiparkinsonian drugs.[14]
History
The area postrema was first named and located in the gross anatomy of the brain by Magnus Gustaf Retzius, a Swedish anatomist, anthropologist and professor of histology. In 1896, he published a two-volume monograph on the gross anatomy of the human brain in which the area postrema was mentioned.[citation needed] In 1975, evidence of neurons in the area postrema of several mammal species was published.[15]
Scientists became increasingly interested in the research of vomiting in the 1950s, perhaps in part due to society's heightened awareness of
In 1953, Borison and Wang determined that the chemosensor area acted as a vomiting trigger zone in the brain stem, which they named the chemoreceptor trigger zone (CTZ) for emesis. Using cats and dogs as model organisms, they found that the removal of this trigger zone from the brain allowed for the prevention of emesis in the animals directly following injection of certain chemicals into the blood, demonstrating the existence of a relationship between the trigger zone and the act of vomiting. The CTZ was anatomically located in the area postrema of the medulla oblongata. The area postrema had been anatomically identified and named nearly 60 years earlier, but its function had remained unknown until its role in emesis was later confirmed.[16]
Current research
Research has continued today around the world on the functions of the area postrema. Beyond its role in emesis, as studied intensely by the researchers of the mid-1900s, the activity of the area postrema has been closely linked to other autonomic functions such as regulation of food intake, body fluid homeostasis, and
Potential treatments
A 2002 study in Japan tested a drug that may be of use in curbing the emetic response to drugs that increase dopamine concentrations. The study investigated morphine-induced emesis in ferrets, explaining that morphine exposure triggered dopamine release in the medulla oblongata and in the area postrema by activating opiate receptors, which in turn caused vomiting by the ferrets. Yet a pre-treatment with 6-hydroxydopamine, a dopaminergic neurotoxin, significantly reduced the number of emetic episodes in the ferrets following morphine exposure. This neurotoxin reduced levels of dopamine, noradrenaline, and homovanillic acid, a metabolite of dopamine, and is known to destroy noradrenergic and dopaminergic neurons. Here, 6-hydroxydopamine was injected directly into the medulla oblongata but not in other parts of the brain. This study shows how the dopaminergic pathway in the medulla oblongata may be manipulated in order to reduce the nauseating side-effects associated with so many dopamine-increasing drugs.[20]
Continuing pathological studies
The area postrema is also indicated in an
There are also studies still currently underway to determine the effect of ablation of the area postrema on
The mechanism for this physiological reaction is still not fully understood, but the area postrema's ability to regulate cardiovascular function presents a very interesting direction for neuroendocrinology.References
- ^ PMID 31334969. Retrieved 4 December 2019.
- ^ PMID 2260724.
- ^ S2CID 42334122.
- ^ PMID 1954559.
- ^ S2CID 58947441.
- ^ S2CID 25603661.
- ISBN 978-0-443-04560-8.
- ^ S2CID 21792860.
- S2CID 28944289.
- S2CID 23652492.
- S2CID 12032912.
- ^ Dictionary of Biological Psychology By Philip Winn (2001) Routledge
- S2CID 21897766.
- ^ David E. Golan and Armen H. Tashjian "Principles of Pharmacology: the Pathophysiologic Basis of Drug Therapy"
- S2CID 950178.
- OCLC 24066772.
- S2CID 6422014.
- PMID 11996311.
- PMID 19460361.
- PMID 12233822.
- .
- PMID 8613209.
- S2CID 36991707.
