Benzodiazepine
| Benzodiazepines | |
|---|---|
N05BA | |
| Mode of action | GABAA receptor |
| Legal status | |
| In Wikidata | |
Benzodiazepines (BZD, BDZ, BZs), colloquially called "benzos", are a class of
Benzodiazepines are depressants that enhance the effect of the
Benzodiazepines are generally viewed as safe and effective for short-term use—about two to four weeks
Taken in overdose, benzodiazepines can cause dangerous
Medical uses

Benzodiazepines possess
Panic disorder
Because of their effectiveness, tolerability, and rapid onset of
The
Guidelines issued by the UK-based
Benzodiazepines are usually administered orally; however, very occasionally lorazepam or diazepam may be given intravenously for the treatment of panic attacks.[24]
Generalized anxiety disorder
Benzodiazepines have robust efficacy in the short-term management of
Likewise, Canadian Psychiatric Association (CPA) recommends benzodiazepines alprazolam, bromazepam, lorazepam, and diazepam only as a second-line choice, if the treatment with two different antidepressants was unsuccessful. Although they are second-line agents, benzodiazepines can be used for a limited time to relieve severe anxiety and agitation. CPA guidelines note that after 4–6 weeks the effect of benzodiazepines may decrease to the level of placebo, and that benzodiazepines are less effective than antidepressants in alleviating ruminative worry, the core symptom of GAD. However, in some cases, a prolonged treatment with benzodiazepines as the add-on to an antidepressant may be justified.[39]
A 2015 review found a larger effect with medications than talk therapy.
Anxiety
Benzodiazepines are sometimes used in the treatment of acute anxiety, as they bring about rapid and marked relief of symptoms in most individuals;[32] however, they are not recommended beyond 2–4 weeks of use due to risks of tolerance and dependence and a lack of long-term effectiveness. As for insomnia, they may also be used on an irregular/"as-needed" basis, such as in cases where said anxiety is at its worst. Compared to other pharmacological treatments, benzodiazepines are twice as likely to lead to a relapse of the underlying condition upon discontinuation. Psychological therapies and other pharmacological therapies are recommended for the long-term treatment of generalized anxiety disorder. Antidepressants have higher remission rates and are, in general, safe and effective in the short and long term.[32]
Insomnia
Benzodiazepines can be useful for short-term treatment of insomnia. Their use beyond 2 to 4 weeks is not recommended due to the risk of dependence. The Committee on Safety of Medicines report recommended that where long-term use of benzodiazepines for insomnia is indicated then treatment should be intermittent wherever possible.
The list of benzodiazepines approved for the treatment of insomnia is fairly similar among most countries, but which benzodiazepines are officially designated as first-line hypnotics prescribed for the treatment of insomnia varies between countries.[43] Longer-acting benzodiazepines such as nitrazepam and diazepam have residual effects that may persist into the next day and are, in general, not recommended.[42]
Since the release of
Older adults should not use benzodiazepines to treat insomnia unless other treatments have failed.
Seizures
Prolonged convulsive
When benzodiazepines were first introduced, they were enthusiastically adopted for treating all forms of
Alcohol withdrawal
Chlordiazepoxide is the most commonly used benzodiazepine for alcohol detoxification,[55] but diazepam may be used as an alternative. Both are used in the detoxification of individuals who are motivated to stop drinking, and are prescribed for a short period of time to reduce the risks of developing tolerance and dependence to the benzodiazepine medication itself.[24]: 275 The benzodiazepines with a longer half-life make detoxification more tolerable, and dangerous (and potentially lethal) alcohol withdrawal effects are less likely to occur. On the other hand, short-acting benzodiazepines may lead to breakthrough seizures, and are, therefore, not recommended for detoxification in an outpatient setting. Oxazepam and lorazepam are often used in patients at risk of drug accumulation, in particular, the elderly and those with cirrhosis, because they are metabolized differently from other benzodiazepines, through conjugation.[56][57]
Benzodiazepines are the preferred choice in the management of alcohol withdrawal syndrome, in particular, for the prevention and treatment of the dangerous complication of seizures and in subduing severe delirium.[58] Lorazepam is the only benzodiazepine with predictable intramuscular absorption and it is the most effective in preventing and controlling acute seizures.[59]
Other indications
Benzodiazepines are often prescribed for a wide range of conditions:
- They can sedate patients receiving respiratory depression, and it is recommended that benzodiazepine overdose treatment facilities should be available.[60] They have also been found to increase the likelihood of later PTSD after people have been removed from ventilators.[61]
- Benzodiazepines are indicated in the management of breathlessness (shortness of breath) in advanced diseases, in particular where other treatments have failed to adequately control symptoms.[62]
- Benzodiazepines are effective as medication given a couple of hours before surgery to relieve anxiety. They also produce dental phobia as well as some ophthalmic procedures like refractive surgery; although such use is controversial and only recommended for those who are very anxious.[64] Midazolam is the most commonly prescribed for this use because of its strong sedative actions and fast recovery time, as well as its water solubility, which reduces pain upon injection. Diazepam and lorazepam are sometimes used. Lorazepam has particularly marked amnesic properties that may make it more effective when amnesia is the desired effect.[24]: 693
- Benzodiazepines are well known for their strong muscle-relaxing properties and can be useful in the treatment of muscle spasms,[24]: 577–578 although tolerance often develops to their muscle relaxant effects.[15] Baclofen[65] or tizanidine are sometimes used as an alternative to benzodiazepines. Tizanidine has been found to have superior tolerability compared to diazepam and baclofen.[66]
- Benzodiazepines are also used to treat the acute panic caused by neuroleptics (antipsychotics) take effect. Lorazepam is most commonly used but clonazepam is sometimes prescribed for acute psychosis or mania;[69] their long-term use is not recommended due to risks of dependence.[24]: 204 Further research investigating the use of benzodiazepines alone and in combination with antipsychotic medications for treating acute psychosis is warranted.[70]
- Rapid eye movement behavior disorder responds well to low doses of clonazepam.[72][73] Restless legs syndrome can be treated using clonazepam as a third line treatment option as the use of clonazepam is still investigational.[74][75]
- Benzodiazepines are sometimes used for obsessive–compulsive disorder (OCD), although they are generally believed ineffective for this indication. Effectiveness was, however, found in one small study.[76] Benzodiazepines can be considered as a treatment option in treatment resistant cases.[77]
- Antipsychotics are generally a first-line treatment for delirium; however, when delirium is caused by alcohol or sedative hypnotic withdrawal, benzodiazepines are a first-line treatment.[78]
- There is some evidence that low doses of benzodiazepines reduce adverse effects of electroconvulsive therapy.[79]
Contraindications
Because of their muscle relaxant action, benzodiazepines may cause
Pregnancy
In the United States, the
Exposure to benzodiazepines during pregnancy has been associated with a slightly increased (from 0.06 to 0.07%) risk of
Elderly
The benefits of benzodiazepines are least and the risks are greatest in the elderly.
Long-term use of benzodiazepines is associated with increased risk of cognitive impairment and dementia, and reduction in prescribing levels is likely to reduce dementia risk.[13] The association of a history of benzodiazepine use and cognitive decline is unclear, with some studies reporting a lower risk of cognitive decline in former users, some finding no association and some indicating an increased risk of cognitive decline.[96]
Benzodiazepines are sometimes prescribed to treat behavioral symptoms of dementia. However, like antidepressants, they have little evidence of effectiveness, although antipsychotics have shown some benefit.[97][98] Cognitive impairing effects of benzodiazepines that occur frequently in the elderly can also worsen dementia.[99]
Adverse effects
The most common side-effects of benzodiazepines are related to their sedating and muscle-relaxing action. They include
The
Compared to other sedative-hypnotics, visits to the hospital involving benzodiazepines had a 66% greater odds of a serious adverse health outcome. This included hospitalization, patient transfer, or death, and visits involving a combination of benzodiazepines and non-benzodiapine receptor agonists had almost four-times increased odds of a serious health outcome.[30]
In September 2020, the U.S. Food and Drug Administration (FDA) required the boxed warning be updated for all benzodiazepine medicines to describe the risks of abuse, misuse, addiction, physical dependence, and withdrawal reactions consistently across all the medicines in the class.[109]
Cognitive effects
The short-term use of benzodiazepines adversely affects multiple areas of cognition, the most notable one being that it interferes with the formation and consolidation of memories of new material and may induce complete anterograde amnesia.[80] However, researchers hold contrary opinions regarding the effects of long-term administration. One view is that many of the short-term effects continue into the long-term and may even worsen, and are not resolved after stopping benzodiazepine usage. Another view maintains that cognitive deficits in chronic benzodiazepine users occur only for a short period after the dose, or that the anxiety disorder is the cause of these deficits.
While the definitive studies are lacking, the former view received support from a 2004 meta-analysis of 13 small studies.[107][110] This meta-analysis found that long-term use of benzodiazepines was associated with moderate to large adverse effects on all areas of cognition, with visuospatial memory being the most commonly detected impairment. Some of the other impairments reported were decreased IQ, visiomotor coordination, information processing, verbal learning and concentration. The authors of the meta-analysis[110] and a later reviewer[107] noted that the applicability of this meta-analysis is limited because the subjects were taken mostly from withdrawal clinics; the coexisting drug, alcohol use, and psychiatric disorders were not defined; and several of the included studies conducted the cognitive measurements during the withdrawal period.
Paradoxical effects
Long-term worsening of psychiatric symptoms
While benzodiazepines may have short-term benefits for anxiety, sleep and agitation in some patients, long-term (i.e., greater than 2–4 weeks) use can result in a worsening of the very symptoms the medications are meant to treat. Potential explanations include exacerbating cognitive problems that are already common in anxiety disorders, causing or worsening depression and suicidality,[116][117] disrupting sleep architecture by inhibiting deep stage sleep,[118] withdrawal symptoms or rebound symptoms in between doses mimicking or exacerbating underlying anxiety or sleep disorders,[116][117] inhibiting the benefits of psychotherapy by inhibiting memory consolidation and reducing fear extinction,[119][120][121] and reducing coping with trauma/stress and increasing vulnerability to future stress.[122] The latter two explanations may be why benzodiazepines are ineffective and/or potentially harmful in PTSD and phobias.[123] Anxiety, insomnia and irritability may be temporarily exacerbated during withdrawal, but psychiatric symptoms after discontinuation are usually less than even while taking benzodiazepines.[116][124] Functioning significantly improves within 1 year of discontinuation.[116][125]
Physical dependence, withdrawal and post-withdrawal syndromes
Tolerance
The main problem of the chronic use of benzodiazepines is the development of tolerance and dependence. Tolerance manifests itself as diminished pharmacological effect and develops relatively quickly to the sedative, hypnotic, anticonvulsant, and muscle relaxant actions of benzodiazepines. Tolerance to anti-anxiety effects develops more slowly with little evidence of continued effectiveness beyond four to six months of continued use.[15] In general, tolerance to the amnesic effects does not occur.[99] However, controversy exists as to tolerance to the anxiolytic effects with some evidence that benzodiazepines retain efficacy[126] and opposing evidence from a systematic review of the literature that tolerance frequently occurs[25][32] and some evidence that anxiety may worsen with long-term use.[15] The question of tolerance to the amnesic effects of benzodiazepines is, likewise, unclear.[127] Some evidence suggests that partial tolerance does develop, and that, "memory impairment is limited to a narrow window within 90 minutes after each dose".[128]
A major disadvantage of benzodiazepines is that tolerance to therapeutic effects develops relatively quickly while many adverse effects persist. Tolerance develops to hypnotic and myorelaxant effects within days to weeks, and to anticonvulsant and anxiolytic effects within weeks to months.[116] Therefore, benzodiazepines are unlikely to be effective long-term treatments for sleep and anxiety. While BZD therapeutic effects disappear with tolerance, depression and impulsivity with high suicidal risk commonly persist.[116] Several studies have confirmed that long-term benzodiazepines are not significantly different from placebo for sleep[129][130][131] or anxiety.[116][132][133][134] This may explain why patients commonly increase doses over time and many eventually take more than one type of benzodiazepine after the first loses effectiveness.[118][135][136] Additionally, because tolerance to benzodiazepine sedating effects develops more quickly than does tolerance to brainstem depressant effects, those taking more benzodiazepines to achieve desired effects may experience sudden respiratory depression, hypotension or death.[137] Most patients with anxiety disorders and PTSD have symptoms that persist for at least several months,[137] making tolerance to therapeutic effects a distinct problem for them and necessitating the need for more effective long-term treatment (e.g., psychotherapy, serotonergic antidepressants).
Withdrawal symptoms and management
Discontinuation of benzodiazepines or abrupt reduction of the dose, even after a relatively short course of treatment (two to four weeks), may result in two groups of symptoms—rebound and withdrawal. Rebound symptoms are the return of the symptoms for which the patient was treated but worse than before. Withdrawal symptoms are the new symptoms that occur when the benzodiazepine is stopped. They are the main sign of physical dependence.[128]
The most frequent symptoms of withdrawal from benzodiazepines are insomnia, gastric problems,
Symptoms may also occur during a gradual dosage reduction, but are typically less severe and may persist as part of a protracted withdrawal syndrome for months after cessation of benzodiazepines.[141] Approximately 10% of patients experience a notable protracted withdrawal syndrome, which can persist for many months or in some cases a year or longer. Protracted symptoms tend to resemble those seen during the first couple of months of withdrawal but usually are of a sub-acute level of severity. Such symptoms do gradually lessen over time, eventually disappearing altogether.[142]
Benzodiazepines have a reputation with patients and doctors for causing a severe and traumatic withdrawal; however, this is in large part due to the withdrawal process being poorly managed. Over-rapid withdrawal from benzodiazepines increases the severity of the withdrawal syndrome and increases the failure rate. A slow and gradual
Withdrawal is best managed by transferring the physically dependent patient to an equivalent dose of diazepam because it has the longest half-life of all of the benzodiazepines, is metabolised into long-acting active metabolites and is available in low-potency tablets, which can be quartered for smaller doses.
Withdrawal from long term benzodiazepines is beneficial for most individuals.[115] Withdrawal of benzodiazepines from long-term users, in general, leads to improved physical and mental health particularly in the elderly; although some long term users report continued benefit from taking benzodiazepines, this may be the result of suppression of withdrawal effects.[15][105]
Controversial associations
Beyond the well established link between benzodiazepines and psychomotor impairment resulting in motor vehicle accidents and falls leading to fracture; research in the 2000s and 2010s has raised the association between benzodiazepines (and
Dementia
A number of studies have drawn an association between long-term benzodiazepine use and neuro-degenerative disease, particularly Alzheimer's disease.
Infections
Some observational studies have detected significant associations between benzodiazepines and respiratory infections such as pneumonia[149][150] where others have not.[151] A large meta-analysis of pre-marketing randomized controlled trials on the pharmacologically related Z-Drugs suggest a small increase in infection risk as well.[152] An immunodeficiency effect from the action of benzodiazepines on GABA-A receptors has been postulated from animal studies.[153][154]
Cancer
A meta-analysis of observational studies has determined an association between benzodiazepine use and cancer, though the risk across different agents and different cancers varied significantly.[155] In terms of experimental basic science evidence, an analysis of carcinogenetic and genotoxicity data for various benzodiazepines has suggested a small possibility of carcinogenesis for a small number of benzodiazepines.[156]
Pancreatitis
The evidence suggesting a link between benzodiazepines (and Z-Drugs) and pancreatic inflammation is very sparse and limited to a few observational studies from Taiwan.[157][158] A criticism of confounding can be applied to these findings as with the other controversial associations above. Further well-designed research from other populations as well as a biologically plausible mechanism is required to confirm this association.
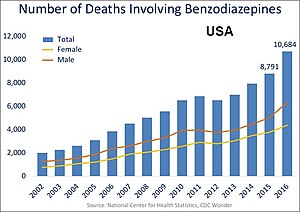
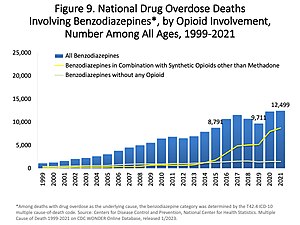
Overdose
Although benzodiazepines are much safer in overdose than their predecessors, the
A reversal agent for benzodiazepines exists,
Interactions
Individual benzodiazepines may have different interactions with certain drugs. Depending on their metabolism pathway, benzodiazepines can be divided roughly into two groups. The largest group consists of those that are metabolized by cytochrome P450 (CYP450) enzymes and possess significant potential for interactions with other drugs. The other group comprises those that are metabolized through glucuronidation, such as lorazepam, oxazepam, and temazepam, and, in general, have few drug interactions.[81]
Many drugs, including
Pharmacology
Pharmacodynamics
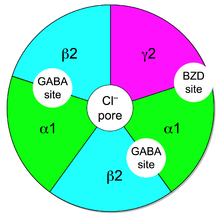
Benzodiazepines work by increasing the effectiveness of the endogenous chemical,
This reduces the communication between neurons and, therefore, has a calming effect on many of the functions of the brain.GABA controls the excitability of neurons by binding to the
The subset of GABAA receptors that also bind benzodiazepines are referred to as benzodiazepine receptors (BzR). The GABAA receptor is a
GABAA receptors participate in the regulation of synaptic pruning by prompting microglial spine engulfment.[177] Benzodiazepines have been shown to upregulate microglial spine engulfment and prompt overzealous eradication of synaptic connections.[178] This mechanism may help explain the increased risk of dementia associated with long-term benzodiazepine treatment.[179]
The benzodiazepine class of drugs also interact with
Pharmacokinetics
| Benzodiazepine | Half-life (range, hours) |
Speed of onset |
|---|---|---|
| Alprazolam | 6–15[184][185] | Intermediate[184] |
| Chlordiazepoxide | 10–30[184] | Intermediate[184] |
| Clonazepam | 19–60[184] | Slow[184] |
| Diazepam | 20–80[184] | Fast[184] |
| Flunitrazepam | 18–26 | Fast |
| Lorazepam | 10–20[184] | Intermediate[184] |
| Midazolam | 1.5–2.5[186] | Fast |
| Oxazepam | 5–10[184] | Slow[184] |
| Prazepam | 50–200[184] | Slow[184] |
| Triazolam | 1.5 | Fast |
A benzodiazepine can be placed into one of three groups by its
- Short-acting compounds have a median half-life of 1–12 hours. They have few residual effects if taken before bedtime, .
- Intermediate-acting compounds have a median half-life of 12–40 hours. They may have some residual effects in the first half of the day if used as a hypnotic. Rebound insomnia, however, is more common upon discontinuation of intermediate-acting benzodiazepines than longer-acting benzodiazepines. Examples are alprazolam, estazolam, flunitrazepam, clonazepam, lormetazepam, lorazepam, nitrazepam, and temazepam.
- Long-acting compounds have a half-life of 40–250 hours. They have a risk of accumulation in the elderly and in individuals with severely impaired liver function, but they have a reduced severity of rebound effects and withdrawal. Examples are diazepam, clorazepate, chlordiazepoxide, and flurazepam.
Chemistry

Benzodiazepines share a similar chemical structure, and their effects in humans are mainly produced by the
The term benzodiazepine is the
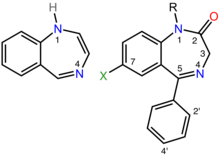
Benzodiazepine drugs are substituted 1,4-benzodiazepines, although the chemical term can refer to many other compounds that do not have useful pharmacological properties. Different benzodiazepine drugs have different side groups attached to this central structure. The different side groups affect the binding of the molecule to the GABAA receptor and so modulate the pharmacological properties.[171] Many of the pharmacologically active "classical" benzodiazepine drugs contain the 5-phenyl-1H-benzo[e] [1,4]diazepin-2(3H)-one substructure (see figure to the right).[190] Benzodiazepines have been found to mimic protein reverse turns structurally, which enable them with their biological activity in many cases.[191][192]
Nonbenzodiazepines also bind to the benzodiazepine binding site on the GABAA receptor and possess similar pharmacological properties. While the nonbenzodiazepines are by definition structurally unrelated to the benzodiazepines, both classes of drugs possess a common pharmacophore (see figure to the lower-right), which explains their binding to a common receptor site.[188]
Types
- 2-keto compounds:
- clorazepate, diazepam, flurazepam, halazepam, prazepam, and others[193][194]
- 3-hydroxy compounds:
- 7-nitro compounds:
- Triazolo compounds:
- Imidazo compounds:
- 1,5-benzodiazepines:
History
The first benzodiazepine,
The new group of drugs was initially greeted with optimism by the medical profession, but gradually concerns arose; in particular, the risk of dependence became evident in the 1980s. Benzodiazepines have a unique history in that they were responsible for the largest-ever
Although antidepressants with anxiolytic properties have been introduced, and there is increasing awareness of the adverse effects of benzodiazepines, prescriptions for short-term anxiety relief have not significantly dropped.[11] For treatment of insomnia, benzodiazepines are now less popular than nonbenzodiazepines, which include zolpidem, zaleplon and eszopiclone.[201] Nonbenzodiazepines are molecularly distinct, but nonetheless, they work on the same benzodiazepine receptors and produce similar sedative effects.[202]
Benzodiazepines have been detected in plant specimens and brain samples of animals not exposed to synthetic sources, including a human brain from the 1940s. However, it is unclear whether these compounds are biosynthesized by microbes or by plants and animals themselves. A microbial biosynthetic pathway has been proposed.[203]
Society and culture
Legal status
In the United States, benzodiazepines are Schedule IV drugs under the Federal Controlled Substances Act, even when not on the market (for example, nitrazepam and bromazepam). Flunitrazepam is subject to more stringent regulations in certain states and temazepam prescriptions require specially coded pads in certain states.[citation needed]
In Canada, possession of benzodiazepines is legal for personal use. All benzodiazepines are categorized as Schedule IV substances under the Controlled Drugs and Substances Act.[204]
In the United Kingdom, benzodiazepines are Class C controlled drugs, carrying the maximum penalty of 7 years imprisonment, an unlimited fine, or both for possession and a maximum penalty of 14 years imprisonment an unlimited fine or both for supplying benzodiazepines to others.[205][206]
In the Netherlands, since October 1993, benzodiazepines, including formulations containing less than 20 mg of temazepam, are all placed on List 2 of the Opium Law. A prescription is needed for possession of all benzodiazepines. Temazepam formulations containing 20 mg or greater of the drug are placed on List 1, thus requiring doctors to write prescriptions in the List 1 format.[207]
In East Asia and Southeast Asia, temazepam and nimetazepam are often heavily controlled and restricted. In certain countries, triazolam, flunitrazepam, flutoprazepam and midazolam are also restricted or controlled to certain degrees. In Hong Kong, all benzodiazepines are regulated under Schedule 1 of Hong Kong's Chapter 134 Dangerous Drugs Ordinance.[208] Previously only brotizolam, flunitrazepam and triazolam were classed as dangerous drugs.[209]
Internationally, benzodiazepines are categorized as Schedule IV controlled drugs, apart from flunitrazepam, which is a Schedule III drug under the Convention on Psychotropic Substances.[210]
Recreational use

Benzodiazepines are considered major addictive substances.
British law requires that temazepam (but not midazolam) be stored in safe custody. Safe custody requirements ensures that pharmacists and doctors holding stock of temazepam must store it in securely fixed double-locked steel safety cabinets and maintain a written register, which must be bound and contain separate entries for temazepam and must be written in ink with no use of correction fluid (although a written register is not required for temazepam in the United Kingdom). Disposal of expired stock must be witnessed by a designated inspector (either a local drug-enforcement police officer or official from health authority).[214][215] Benzodiazepine use ranges from occasional binges on large doses, to chronic and compulsive drug use of high doses.[216]
Benzodiazepines are commonly used recreationally by poly-drug users.
A 1999–2005 Australian police survey of detainees reported preliminary findings that self-reported users of benzodiazepines were less likely than non-user detainees to work full-time and more likely to receive government benefits, use methamphetamine or heroin, and be arrested or imprisoned.
Overall, anecdotal evidence suggests that temazepam may be the most psychologically habit-forming (addictive) benzodiazepine. Non-medical temazepam use reached epidemic proportions in some parts of the world, in particular, in Europe and Australia, and is a major addictive substance in many Southeast Asian countries. This led authorities of various countries to place temazepam under a more restrictive legal status. Some countries, such as Sweden, banned the drug outright.[221] Temazepam also has certain pharmacokinetic properties of absorption, distribution, elimination, and clearance that make it more apt to non-medical use compared to many other benzodiazepines.[222][223]
Veterinary use
Benzodiazepines are used in
References
- ^ ISBN 978-0-19-517668-1.
- PMID 32159714.
- ISBN 978-1-4625-0438-1.
- ^ ISBN 978-0-7234-3221-0.
- ^ PMID 18175099.
- ^ ISBN 978-0-415-43818-6.
- S2CID 1709063.
- ^ PMID 18922233.
- ^ "Benzodiazepines". Better Health Channel. 19 May 2023.
- ^ PMID 28257172.
- ^ S2CID 45155299.
- ^ S2CID 113206.
- ^ S2CID 49351844.
- S2CID 25777653.
- ^ S2CID 1709063.
- ^ ISBN 978-0-19-852783-1.
- S2CID 38797655.)
{{cite journal}}: CS1 maint: numeric names: authors list (link - ^ PMID 18378767.
- ^ PMID 9780123.
- ^ "FDA requires strong warnings for opioid analgesics, prescription opioid cough products, and benzodiazepine labeling related to serious risks and death from combined use". FDA. August 31, 2016. Retrieved 1 September 2016.
- ^ S2CID 20125264.
- ^ PMID 10707430.
- ^ S2CID 43443180.
- ^ ISBN 978-0-85369-845-6.
- ^ S2CID 43437233.
- PMID 1970816.
- PMID 16400293.
- S2CID 32761147.
- ^ "Benzodiazepines in chronic pain". February 2016. Archived from the original on 2016-09-23. Retrieved 2016-09-22.
- ^ PMID 28476551.
- PMID 15762816.
The frequent use of benzodiazepines for the treatment of anxiety is likely a reflection of their effectiveness, rapid onset of anxiolytic effect, and tolerability.
- ^ a b c d e f McIntosh A, Cohen A, Turnbull N, et al. (2004). "Clinical guidelines and evidence review for panic disorder and generalised anxiety disorder" (PDF). National Collaborating Centre for Primary Care. Archived from the original (PDF) on 2009-02-19. Retrieved 2009-06-16.
- S2CID 922780.
- ^ a b c "APA Practice Guideline for the Treatment of Patients With Panic Disorder, Second Edition" (PDF). Work Group on Panic Disorder. January 2009. Retrieved July 12, 2009.
- ^ Barbui C, Cipriani A (2009). "Proposal for the inclusion in the WHO Model List of Essential Medicines of a selective serotonin-reuptake inhibitor for Generalised Anxiety Disorder" (PDF). WHO Collaborating Centre for Research and Training in Mental Health. Archived from the original (PDF) on 2012-05-05. Retrieved 2009-06-23.
- S2CID 20715355.
- S2CID 1879448.
- ^ "Clinical Guideline 22 (amended). Anxiety: management of anxiety (panic disorder, with or without agoraphobia, and generalised anxiety disorder) in adults in primary, secondary and community care" (PDF). National Institute for Health and Clinical Excellence. 2007. pp. 23–25. Archived from the original (PDF) on 2012-05-14. Retrieved 2009-08-08.
- PMID 16933543. Archived from the originalon 2010-07-14. Retrieved 2009-08-08.
- ^ S2CID 24088074.
- ^ "Current problems" (PDF). www.mhra.gov.uk. 1988. Archived from the original (PDF) on 2014-12-06. Retrieved 2020-03-21.
- ^ a b c d "Technology Appraisal Guidance 77. Guidance on the use of zaleplon, zolpidem and zopiclone for the short-term management of insomnia" (PDF). National Institute for Clinical Excellence. April 2004. Archived from the original (PDF) on 2008-12-03. Retrieved 2009-07-26.
- ^ PMID 17853625.
- ISBN 978-0-8261-1094-7.
- ^ a b c Buscemi N, Vandermeer B, Friesen C, Bialy L, Tubman M, Ospina M, Klassen TP, Witmans M (June 2005). "Manifestations and Management of Chronic Insomnia in Adults. Summary, Evidence Report/Technology Assessment: Number 125" (PDF). Agency for Healthcare Research and Quality. Archived (PDF) from the original on 2022-10-09.
- PMID 26711081.
- ^ "Approval letter for Ambien" (PDF). Food and Drug Administration. Archived (PDF) from the original on 2022-10-09.
- ^ a b American Geriatrics Society. "Five Things Physicians and Patients Should Question". Choosing Wisely: An Initiative of the ABIM Foundation. Archived from the original on September 1, 2013. Retrieved August 1, 2013., which cites
- ^ S2CID 9296501.
- PMID 22376048.)
{{cite journal}}: CS1 maint: numeric names: authors list (link - ^ "Diagnosis and management of epilepsy in adults" (PDF). Scottish Intercollegiate Guidelines Network. 2005. pp. 17–19. Archived from the original (PDF) on 2009-01-26. Retrieved 2009-06-05.
- ^ a b Stokes T, Shaw EJ, Juarez-Garcia A, Camosso-Stefinovic J, Baker R (October 2004). Clinical Guidelines and Evidence Review for the Epilepsies: diagnosis and management in adults and children in primary and secondary care (PDF). London: Royal College of General Practitioners. pp. 61, 64–65. Archived (PDF) from the original on 2022-10-09. Retrieved 2009-06-02.
- ^ S2CID 20445985.
- ^ Stokes T, Shaw EJ, Juarez-Garcia A, Camosso-Stefinovic J, Baker R (October 2004). "Clinical Guidelines and Evidence Review for the Epilepsies: diagnosis and management in adults and children in primary and secondary care (Appendix B)" (PDF). London: Royal College of General Practitioners. p. 432. Archived from the original (PDF) on 2011-11-27. Retrieved 2009-06-02.
- PMID 9270461.
- S2CID 2724630.
- PMID 10507746.
- PMID 16623205.
- S2CID 1389910. Archived from the originalon 2020-01-15. Retrieved 2020-02-01.
- PMID 19576523.
- S2CID 11478971.
- PMID 27764523.
- S2CID 259982203.
- PMID 17607891.
- S2CID 12493035.
- S2CID 73086671.
- ISBN 978-0-19-852623-0.
- S2CID 73223621.
- PMID 15013244.
- PMID 23633309.
- PMID 17580590.
- S2CID 43692512.
- PMID 11471763.
- PMID 17876423.
- S2CID 91440. Archived from the original(PDF) on 2009-12-29. Retrieved 2010-01-19.
- ISBN 978-1-58562-309-9.
- S2CID 26691595.
- S2CID 94743.
- S2CID 6423840.
- ^ ISBN 978-0-683-30128-1.
- ^ ISBN 978-0-444-50998-7.
- ^ "Benzodiazepines, dependence and withdrawal symptoms". Committee on Safety of Medicines. 1988. Archived from the original (PDF) on 2012-02-22. Retrieved 2009-05-28.
- ^ ISBN 978-1-58829-211-7.
- ISBN 978-0-7817-7595-3.
- PMID 9748174.
- PMID 9614425.
- ^ Temazepam-Rxlist Pregnancy Category@
- PMID 11773648. Archived from the original(PDF) on 2011-07-27. Retrieved 2011-01-31.
- PMID 18035234.
- PMID 16860264.
- ^ "American Geriatrics Society 2015 updated Beers Criteria for potentially inappropriate medication use in older adults". Guideline Central. American Geriatrics Society. Retrieved 1 December 2018.
- PMID 22566242.
- PMID 15001721.
- ^ ISBN 978-0-470-02428-7.
- ISBN 978-0-7817-6196-3.
- S2CID 7774439.
- S2CID 2758628.
- S2CID 39610712.
- ^ PMID 10779253. Archived from the originalon 2008-05-12. Retrieved 2008-05-25.
- ^ ISBN 978-0-470-02821-6.
- S2CID 206134458.
- PMID 19389334.
- PMID 19418468.
- ^ "benzodiazepines-oral" at medicinenet.com
- ^ ISBN 978-0-19-852748-0.
- ISBN 978-0-8039-7477-7.
- ^ PMID 15762814. Archived from the original(PDF) on 2005-12-13. Retrieved 2009-06-14.
- PMID 33295972.
- ^
 This article incorporates text from this source, which is in the public domain: "FDA expands Boxed Warning to improve safe use of benzodiazepine drug". U.S. Food and Drug Administration (FDA). 23 September 2020. Retrieved 23 September 2020.
This article incorporates text from this source, which is in the public domain: "FDA expands Boxed Warning to improve safe use of benzodiazepine drug". U.S. Food and Drug Administration (FDA). 23 September 2020. Retrieved 23 September 2020.
- ^ S2CID 15340907.
- S2CID 24453988.
- ^ (PDF) from the original on 2022-10-09.
- S2CID 140765796.
- PMID 26256485.
- ^ ISBN 978-0-521-87997-2.
- ^ S2CID 19145509.
- ^ PMID 8803355.
- ^ ISBN 978-0-470-06571-6.
- PMID 9746445.
- PMID 24434093.
- PMID 9299803.
- S2CID 93347.
- OCLC 1250346653.
- S2CID 20586160.
- ^ Pary R, Lewis S (2008). "Prescribing benzodiazepines in clinical practice". Resident and Staff Physician. 54 (1): 8–17.
- S2CID 29469943.
- PMID 15762818. Archived from the original(PDF) on 2005-12-14. Retrieved 2009-06-22.
- ^ PMID 15078112. Archived from the original(PDF) on 2005-12-13. Retrieved 2009-06-22.
- S2CID 20586160.
- PMID 15550406.
- PMID 15003439.
- S2CID 142421768.
- S2CID 59516280.
- S2CID 39027026.
- S2CID 1709063.
- PMID 15531349.
- ^ ISBN 978-0-89042-555-8.
- ISBN 978-0-19-856667-0.
- PMID 12725868.
- PMID 29872302.
- ISBN 978-0-19-150476-1.
- PMID 1675688.
- ^ a b c d Benzodiazepines: how they work & how to withdraw (aka The Ashton Manual). Ashton CH. 2002. Retrieved 2009-05-27.
- ^ Lal R, Gupta S, Rao R, Kattimani S (2007). "Emergency management of substance overdose and withdrawal" (PDF). Substance Use Disorder. World Health Organization (WHO). p. 82. Archived from the original (PDF) on 2010-06-13. Retrieved 2009-06-06.
Generally, a longer-acting benzodiazepine such as chlordiazepoxide or diazepam is used and the initial dose titrated downward
- ^ Ford C, Law F (July 2014). "Guidance for the use and reduction of misuse of benzodiazepines and other hypnotics and anxiolytics in general practice" (PDF). smmgp.org.uk. Archived from the original (PDF) on 2017-07-06. Retrieved 2015-10-18.
- ISBN 978-1-4200-4743-1.
- PMID 28865038.
- PMID 26016483.
- S2CID 24289824. Archived from the original(PDF) on 2018-07-22. Retrieved 2019-07-13.
- S2CID 7021626.
- PMID 22091503.
- PMID 19968019.
- PMID 23478657.
- PMID 8847962.
- S2CID 25777653.
- PMID 17920927.
- PMID 26717383.
- S2CID 26126233.
- S2CID 27619795.
- ^ "Toxicity, benzodiazepine". eMedicine. Robin Mantooth. 28 January 2010. Retrieved 2010-10-02.
- ^ ISBN 978-0-19-852072-6.
- S2CID 13121885.
- PMID 7866122.
- S2CID 46001278.
- S2CID 39966201.
- PMID 1286503.
- PMID 1611650.
- ISBN 978-0-07-136001-2.
- ^ a b Overdose Death Rates. By National Institute on Drug Abuse (NIDA).
- ^ S2CID 35852993.
- ^ ISBN 978-0-12-088397-4.
- PMID 16376150.
- ]
- PMID 8783370.
- PMID 15157182.
- S2CID 32359279.
- S2CID 8422877.
- S2CID 247169270.
- PMID 30375757.
- S2CID 32002501.
- ^ PMID 9504140.
- PMID 9378234.
- ^ PMID 16780077.
- ^ PMID 15762817. Retrieved 5 September 2013.
- ^ "Alprazolam – FDA prescribing information, side effects and uses". Drugs.com. Retrieved 2019-08-28.
- ^ "Midazolam Injection" (PDF). Medsafe. New Zealand Ministry of Health. 2012-10-26. Archived from the original (PDF) on 2016-02-22. Retrieved 2016-04-06.
- ISBN 978-3-7643-7440-2.
- ^ ISBN 978-0-471-21384-0.
- ^ (PDF) from the original on 2022-10-09.
- CAS registry number:2898-08-01,3-dihydro-5-phenyl-2H-1,4-benzodiazepin-2-one; other names: Ro 05-2921, dechlorodemethyldiazepam.
- .
- S2CID 2777635.
- ^ a b c d e Juergens SM. "Understanding Benzodiazepines" (PDF). California Society of Addiction Medicine. Archived from the original (PDF) on 8 May 2012. Retrieved 25 April 2012.
- ^ PMID 2925017.
- PMID 34039.
During this cleanup operation, my co-worker, Earl Reeder, drew my attention to a few hundred milligrams of two products, a nicely crystalline base and its hydrochloride. Both the base, which had been prepared by treating the quinazoline N-oxide 11 with methylamine, and its hydrochloride had been made sometime in 1955. The products were not submitted for pharmacological testing at that time because of our involvement with other problems
- PMID 1971487.
- PMID 1389432.
- ^ Peart R (1999-06-01). "Memorandum by Dr Reg Peart". Minutes of Evidence. Select Committee on Health, House of Commons, UK Parliament. Retrieved 2009-05-27.
- ^ PMC 1676757.
- PMID 8870565.
- PMID 18265473.
- S2CID 43180871.
- S2CID 1125401.
- ^ "Controlled Drugs and Substances Act". Canadian Department of Justice. Retrieved 2009-05-27.
- ^ Blackpool NHS Primary Care Trust (1 May 2008). "Medicines Management Update" (PDF). United Kingdom National Health Service. Archived from the original (PDF) on 4 December 2010. Retrieved 2009-05-27.
- ^ "List of Drugs Currently Controlled Under The Misuse of Drugs Legislation" (PDF). Misuse of Drugs Act UK. British Government. Archived from the original (PDF) on 2007-02-05. Retrieved 2009-05-27.
- ^ "Opium Law" (PDF). Dutch Government. 29 November 2004. Archived from the original (PDF) on October 20, 2008. Retrieved 2009-05-27.
- Hong Kong Government. "Dangerous Drugs Ordinance – Schedule 1". Hong Kong Ordinances. Hong Kong: hklii.org. Archived from the originalon 2011-09-27. Retrieved 2015-12-10.
- PMID 8523479.
- ^ "List of psychotropic substances under international control" (PDF). incb.org. International Narcotics Control Board. August 2003. Archived from the original (PDF) on 2005-12-05. Retrieved 2008-12-17.
- ^ Chris Ford (2009). "What is possible with benzodiazepines". UK: Exchange Supplies, 2009 National Drug Treatment Conference. Archived from the original on 1 May 2010.
- ^ "List of psychotropic substances under international control" (PDF). International Narcotics Control Board. 2003. Archived from the original (PDF) on 2005-12-05. Retrieved 2008-12-17.
- ^ "Controlled drugs and drug dependence". United Kingdom: British National Formulary. 3 January 2020.(Note: The British National Formulary is only accessible in the UK. A cached copy is available from Google.)
- ^ Home Office (2005). Explanatory memorandum to the misuse of drugs and the misuse of drugs Archived December 16, 2010, at the Wayback Machine (supply to addicts) (amendment) regulations 2005. No. 2864. Accessed 20–10–03
- ^ "List of drugs currently controlled under the misuse of drugs legislation". UK Government Home Office. 2010-10-25. Archived from the original (PDF) on 2011-02-18. Retrieved 2011-01-30.
- ISBN 978-0-8493-1690-6.
- .
- PMID 9274553.
- ISSN 0817-8542. Archived from the original(PDF) on 2017-08-12. Retrieved 2009-06-10.
- S2CID 28981255.
- ^ "Benzodiazepine abuse". Benzo.org.uk. Retrieved 2011-11-28.
- PMID 1786493.
- S2CID 41959044.
- ^ ISBN 978-0-911910-50-6.
- PMID 2520134.
- PMID 8813750.
- ISBN 978-0-8138-1743-9.
External links
- National Institute on Drug Abuse: "NIDA for Teens: Prescription Depressant Medications".
- Ashton CH (2002). Benzodiazepines: how they work & how to withdraw (aka The Ashton Manual). Retrieved 2009-06-09.
- Ashton CH (2007). "Benzodiazepine equivalence table". Retrieved 2009-06-09.
- Fruchtengarten L (April 1998). Ruse M (ed.). "Benzodiazepines". Poisons Information Monograph (Group monograph) G008. International Programme on Chemical Safety INCHEM. Retrieved 2009-06-09.
- Longo LP, Johnson B (April 2000). "Addiction: Part I. Benzodiazepines – side effects, abuse risk and alternatives". PMID 10779253. Archived from the originalon 2008-05-12. Retrieved 2008-05-25.
- "The complete story of the benzodiazepines". The Eaton T. Fores Research Center. 2005. Archived from the original on June 5, 2009. Retrieved 2009-06-09.
- "Benzodiazepines". Drugs.com.
- Benzodiazepines – information from mental health charity The Royal College of Psychiatrists
- "Benzodiazepines". RxList.
- "benzodiazepines-oral" at medicinenet.com