Biomaterial
A biomaterial is a substance that has been engineered to interact with biological systems for a medical purpose – either a therapeutic (treat, augment, repair, or replace a tissue function of the body) or a diagnostic one. The corresponding field of study, called biomaterials science or biomaterials engineering, is about fifty years old.[needs update] It has experienced steady growth over its history, with many companies investing large amounts of money into the development of new products. Biomaterials science encompasses elements of medicine, biology, chemistry, tissue engineering and materials science.
A biomaterial is different from a biological material, such as bone, that is produced by a biological system. However, "biomaterial" and "biological material" are often used interchangeably. Further, the word "bioterial" has been proposed as a potential alternate word for biologically-produced materials such as bone, or fungal biocomposites.[citation needed] Additionally, care should be exercised in defining a biomaterial as biocompatible, since it is application-specific. A biomaterial that is biocompatible or suitable for one application may not be biocompatible in another.[1]
Material exploited in contact with living tissues, organisms, or microorganisms.[2][a][b][c]
Introduction
Biomaterials can be derived either from nature or
Bioactivity
The ability of an engineered biomaterial to induce a physiological response that is supportive of the biomaterial's function and performance is known as bioactivity. Most commonly, in bioactive glasses and bioactive ceramics this term refers to the ability of implanted materials to bond well with surrounding tissue in either osteo conductive or osseo productive roles.[4] Bone implant materials are often designed to promote bone growth while dissolving into surrounding body fluid.[5] Thus for many biomaterials good biocompatibility along with good strength and dissolution rates are desirable. Commonly, bioactivity of biomaterials is gauged by the surface biomineralization in which a native layer of hydroxyapatite is formed at the surface. These days, the development of clinically useful biomaterials is greatly enhanced by the advent of computational routines that can predict the molecular effects of biomaterials in a therapeutic setting based on limited in vitro experimentation.[6]
Self-assembly
Molecular self assembly is found widely in biological systems and provides the basis of a wide variety of complex biological structures. This includes an emerging class of mechanically superior biomaterials based on microstructural features and designs found in nature. Thus, self-assembly is also emerging as a new strategy in chemical synthesis and
Structural hierarchy
Nearly all materials could be seen as hierarchically structured, since the changes in spatial scale bring about different mechanisms of deformation and damage.
In another level of complexity, the hydroxyapatite crystals are mineral platelets that have a diameter of approximately 70 to 100 nm and thickness of 1 nm. They originally nucleate at the gaps between collagen fibrils.[12]
Similarly, the hierarchy of abalone shell begins at the nanolevel, with an organic layer having a thickness of 20 to 30 nm. This layer proceeds with single crystals of aragonite (a polymorph of CaCO3) consisting of "bricks" with dimensions of 0.5 and finishing with layers approximately 0.3 mm (mesostructure).[13]
Crabs are arthropods, whose carapace is made of a mineralized hard component (exhibits brittle fracture) and a softer organic component composed primarily of chitin. The brittle component is arranged in a helical pattern. Each of these mineral "rods" (1 μm diameter) contains chitin–protein fibrils with approximately 60 nm diameter. These fibrils are made of 3 nm diameter canals that link the interior and exterior of the shell.
Applications
Biomaterials are used in:
- Joint replacements
- Bone plates [14]
- Intraocular lenses (IOLs) for eye surgery
- Bone cement
- Artificial ligaments and tendons
- Dental implantsfor tooth fixation
- Blood vessel prostheses
- Heart valves
- Skin repair devices (artificial tissue)
- Cochlear replacements
- Contact lenses
- Breast implants
- Drug delivery mechanisms
- Sustainable materials
- Vascular grafts
- Stents
- Nerve conduits
- Surgical sutures, clips, and staples for wound closure[15]
- Pins and screws for fracture stabilisation[16]
- Surgical mesh[17][18]
Biomaterials must be compatible with the body, and there are often issues of biocompatibility, which must be resolved before a product can be placed on the market and used in a clinical setting. Because of this, biomaterials are usually subjected to the same requirements as those undergone by new drug therapies.[19][20] All manufacturing companies are also required to ensure traceability of all of their products, so that if a defective product is discovered, others in the same batch may be traced.
Bone grafts
Calcium sulfate (its α- and β-hemihydrates) is a well known biocompatible material that is widely used as a bone graft substitute in dentistry or as its binder.[21][22]
Heart valves
In the United States, 49% of the 250,000 valve replacement procedures performed annually involve a mechanical valve implant. The most widely used valve is a bileaflet disc heart valve or St. Jude valve. The mechanics involve two semicircular discs moving back and forth, with both allowing the flow of blood as well as the ability to form a seal against backflow. The valve is coated with pyrolytic carbon and secured to the surrounding tissue with a mesh of woven fabric called Dacron (du Pont's trade name for polyethylene terephthalate). The mesh allows for the body's tissue to grow, while incorporating the valve.[23] [verification needed]
Skin repair
Most of the time, artificial tissue is grown from the patient's own cells. However, when the damage is so extreme that it is impossible to use the patient's own cells, artificial tissue cells are grown. The difficulty is in finding a scaffold that the cells can grow and organize on. The characteristics of the scaffold must be that it is biocompatible, cells can adhere to the scaffold, mechanically strong and
Properties
As discussed previously, biomaterials are used in medical devices to treat, assist, or replace a function within the human body. The application of a specific biomaterial must combine the necessary composition, material properties, structure, and desired in vivo reaction in order to perform the desired function. Categorizations of different desired properties are defined in order to maximize functional results.[24][25]
Host response
Host response is defined as the "response of the host organism (local and systemic) to the implanted material or device". Most materials will have a reaction when in contact with the human body. The success of a biomaterial relies on the host tissue's reaction with the foreign material. Specific reactions between the host tissue and the biomaterial can be generated through the biocompatibility of the material.[25][26]
Biomaterial and tissue interactions
The
Tissue injury caused by device implantation causes inflammatory and healing responses during FBR. The inflammatory response occurs within two time periods: the acute phase, and the chronic phase. The acute phase occurs during the initial hours to days of implantation, and is identified by fluid and protein exudation[28] along with a neutrophilic reaction.[29] During the acute phase, the body attempts to clean and heal the wound by delivering excess blood, proteins, and monocytes are called to the site.[30] Continued inflammation leads to the chronic phase, which can be categorized by the presence of monocytes, macrophages, and lymphocytes.[29] In addition, blood vessels and connective tissue form in order to heal the wounded area.[31]
Compatibility
Toxicity
A biomaterial should perform its intended function within the living body without negatively affecting other bodily tissues and organs. In order to prevent unwanted organ and tissue interactions, biomaterials should be
Biodegradable biomaterials
Biodegradable biomaterials refers to materials that are degradable through natural
Biocompatible plastics
Some of the most commonly-used
Surface and bulk properties
Two properties that have a large effect on the functionality of a biomaterial is the surface and bulk properties.[41]
Bulk properties refers to the physical and chemical properties that compose the biomaterial for its entire lifetime. They can be specifically generated to mimic the physiochemical properties of the tissue that the material is replacing. They are mechanical properties that are generated from a material's atomic and molecular construction.
Important bulk properties:[42]
- Chemical Composition
- Microstructure
- Elasticity
- Tensile Strength
- Density
- Hardness
- Electrical Conductivity
- Thermal Conductivity
Surface properties refers to the chemical and topographical features on the surface of the biomaterial that will have direct interaction with the host blood/tissue.[43] Surface engineering and modification allows clinicians to better control the interactions of a biomaterial with the host living system.
Important surface properties:[44]
- Wettability(surface energy)
- Surface chemistry
- Surface textures (smooth/rough)
- Topographical factors including: size, shape, alignment, structure determine the roughness of a material.[45]
- Surface Tension
- Surface Charge
Mechanical properties
In addition to a material being certified as
For implanted biomaterials that may experience
For medical devices that are implanted or attached to the skin, another important property requiring consideration is the
Structure
The molecular composition of a biomaterial determines the physical and chemical properties of a biomaterial. These compositions create complex structures that allow the biomaterial to function, and therefore are necessary to define and understand in order to develop a biomaterial. biomaterials can be designed to replicate natural organisms, a process known as biomimetics.[49] The structure of a biomaterial can be observed at different at different levels to better understand a materials properties and function.
Atomic structure

The arrangement of
The sub atomic level observes the electrical structure of an individual atom to define its interactions with other atoms and molecules. The molecular structure observes the arrangement of atoms within the material. Finally the ultra-structure observes the 3-D structure created from the atomic and molecular structures of the material. The solid-state of a material is characterized by the intramolecular bonds between the atoms and molecules that comprise the material. Types of intramolecular bonds include: ionic bonds, covalent bonds, and metallic bonds. These bonds will dictate the physical and chemical properties of the material, as well as determine the type of material (ceramic, metal, or polymer).
Microstructure
The
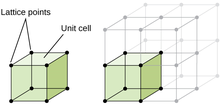
Crystalline structure
Defects of crystalline structure
During the formation of a crystalline structure, different impurities, irregularities, and other defects can form. These imperfections can form through deformation of the solid, rapid cooling, or high energy radiation.[56] Types of defects include point defects, line defects, as well as edge dislocation.
Macrostructure
Macrostructure refers to the overall geometric properties that will influence the force at failure, stiffness, bending, stress distribution, and the weight of the material. It requires little to no magnification to reveal the macrostructure of a material. Observing the macrostructure reveals properties such as cavities, porosity, gas bubbles, stratification, and fissures.[57] The material's strength and elastic modulus are both independent of the macrostructure.
Natural biomaterials
Biomaterials can be constructed using only materials sourced from plants and animals in order to alter, replace, or repair human tissue/organs. Use of natural biomaterials were used as early as ancient Egypt, where indigenous people used animal skin as sutures. A more modern example is a hip replacement using ivory material which was first recorded in Germany 1891.[58]
Valuable criteria for viable natural biomaterials:
- Biodegradable
- Biocompatible
- Able to promote cell attachment and growth
- Non-toxic
Examples of natural biomaterials:
Biopolymers
Biopolymers are polymers produced by living organisms. Cellulose and starch, proteins and peptides, and DNA and RNA are all examples of biopolymers, in which the monomeric units, respectively, are sugars, amino acids, and nucleotides.[61] Cellulose is both the most common biopolymer and the most common organic compound on Earth. About 33% of all plant matter is cellulose.[62][63] On a similar manner, silk (proteinaceous biopolymer) has garnered tremendous research interest in a myriad of domains including tissue engineering and regenerative medicine, microfluidics, drug delivery.[64][65]
See also
- Bionics
- Hydrogel
- Polymeric surface
- Surface modification of biomaterials with proteins
- Synthetic biodegradable polymer
- List of biomaterials
Footnotes
- ^ The notion of exploitation includes utility for applications and for fundamental research to understand reciprocal perturbations as well.[2]
- ^ The definition "non-viable material used in a medical device, intended to interact with biological systems" recommended in ref.[3] cannot be extended to the environmental field where people mean "material of natural origin".[2]
- ^ This general term should not be confused with the terms biopolymer or biomacromolecule. The use of "polymeric biomaterial" is recommended when one deals with polymer or polymer device of therapeutic or biological interest.[2]
References
- ISBN 9783540777823. Archivedfrom the original on 9 December 2017. Retrieved 29 February 2016.
- ^ S2CID 98107080.
- ^ Williams, D. F., ed. (2004). Definitions in Biomaterials, Proceedings of a Consensus Conference of the European Society for Biomaterials. Amsterdam: Elsevier.
- .
- S2CID 105932012.
- PMID 33117780.
- PMID 1962191.
- PMID 11031294.
- PMID 27877935.
- S2CID 254094123.
- PMC 2222831.
- )
- ISBN 978-1-4614-6255-2.
- PMID 27770965.
- S2CID 20278355.
- S2CID 24385943.
- PMID 26229409.
- S2CID 33728690.
- .
- .
- PMID 34070157.
- PMID 16393128.
- ^ ISBN 978-0-13-084090-5.
- S2CID 240851982.
- ^ ISBN 978-0-12-800500-2.
- PMID 18440630.
- PMID 20143194.
- ^ "Exudate: MedlinePlus Medical Encyclopedia". United States National Library of Medicine. Retrieved July 11, 2023.
- ^ a b Rn, Mitchell (2003). "Acute and chronic inflammation". Robbins Basic Pathology.
- PMID 3279314.
- PMID 2015044.
- S2CID 73489194.
- ^ Kammula, Raju G.; Morris, Janine M. (May 1, 2001). "Considerations for the Biocompatibility Evaluation of Medical Devices". Medical Device & Diagnostic Industry.
- PMID 26894284.
- ISBN 9780323328890. Retrieved 2022-05-06.
- PMID 26694936.
- PMID 32123302.
- ^ PMID 30288019.
- PMID 30288019.
- ISBN 978-1-4822-4838-8.
- ^ "what is a surface, why is surface analysis important". www.kratos.com. Retrieved 2022-05-06.
- ISBN 978-0-12-816137-1. Retrieved 2022-07-26.
- S2CID 46254118.
- ISBN 978-0-12-415995-2.
- ^ "How surface roughness and wettability affects biocompatibility". www.biolinscientific.com. Retrieved 2022-05-06.
- ^ PMID 25610850.
- S2CID 10104005.
- S2CID 205264592.
- ISBN 978-0-12-238662-6.
- ^ Partlow, William (2022-03-13). "1 - Biomaterials". Beyond Discovery. Retrieved 2022-05-06.
- ^ "Microstructure". CES Information Guide - Materials Science Engineering. depts.washington.edu. Retrieved 2022-05-06.
- ISBN 9782842992866. Retrieved 2022-05-06.
- ^ "Crystalline Structure: Definition, Structure & Bonding". Study.com. Retrieved 2022-05-06.
- ^ "10.6 Lattice Structures in Crystalline Solids – Chemistry". opentextbc.ca. Retrieved 2022-05-06.
- ^ "Bravais Lattice - 14 Possible Crystal Structures with Illustrations". BYJUS. Retrieved 2022-05-06.
- ^ "crystal defect | Definition, Types, & Facts | Britannica". www.britannica.com. Retrieved 2022-05-06.
- ^ "Macrostructure". TheFreeDictionary.com. Retrieved 2022-05-06.
- ^ "Natural Biomaterials by Isabel Hand - OpenWetWare". openwetware.org. Retrieved 2022-05-06.
- ^ "Kelp (Laminaria digitata) – Irish Seaweeds". Retrieved 2022-05-06.
- PMID 25066525.
- PMID 19229265.
- PMID 9271562.
- PMID 15861454.
- S2CID 208833880.
- S2CID 132470283.
