Bloodletting
| Bloodletting | |
|---|---|
 Bloodletting in 1860 | |
| MeSH | D001815 |

Bloodletting (or blood-letting) is the withdrawal of
Today, the term
In the ancient world

Passages from the Ebers Papyrus may indicate that bloodletting by scarification was an accepted practice in Ancient Egypt.[9][10][11] Egyptian burials have been reported to contain bloodletting instruments.[12] According to some accounts, the Egyptians based the idea on their observations of the hippopotamus,[13] confusing its red secretions with blood and believing that it scratched itself to relieve distress.[14][15]
In Greece, bloodletting was in use in the 5th century BC during the lifetime of
"Bleeding" a patient to health was modeled on the process of
The popularity of bloodletting in the classical Mediterranean world was reinforced by the ideas of Galen, after he discovered that not only
Galen created a complex system of how much blood should be removed based on the patient's age, constitution, the season, the weather and the place. "Do-it-yourself" bleeding instructions following these systems were developed.. The more severe the disease, the more blood would be let. Fevers required copious amounts of bloodletting.
Cross-cultural bloodletting
Therapeutic uses of bloodletting were reported in 60 distinct cultures/ethnic groups in the eHRAF database, present in all inhabited continents. Bloodletting has also been reported in 15 of the 60 cultures in the probability sample files (PSF) list.[22] The PSF is a subset of eHRAF data that includes only one culture from each of 60 macro-culture areas around the world. The prevalence of bloodletting in PSF controls for pseudo replication linked to common ancestry, suggesting that bloodletting has independently emerged many times. Bloodletting is varied in its practices cross-culturally, for example, in native Alaskan culture bloodletting was practiced for different indications, using different tools, on different body areas, by different people, and it was explained by different medical theories.[23]
According to Helena Miton et al.'s [22] analysis of the eHRAF database and other sources, there are several cross-cultural patterns in bloodletting.
- Bloodletting is not self-administered. Out of 14 cultures in which the bloodletting practitioner was mentioned, the practitioner was always a third party. 13/14 of the cultures had practitioners with roles related to medicine, while one culture had a practitioner whose role was not related to medicine.
- Idea of bloodletting removing 'bad blood' that needs to be taken out was common, and was explicitly mentioned in 10/14 cultures studied with detailed descriptions of bloodletting.
- Bloodletting is not thought to be effective against illness caused supernaturally by humans (e.g. witchcraft). This is surprising, because in most cultures witchcraft and sorcery can be blamed for ailments.[24] But out of 14 cultures with detailed bloodletting descriptions, there was no evidence of bloodletting being used to cure witchcraft-related ailments, while bloodletting was recorded as a cure for ailments of other origins. The Azande culture has been recorded to believe that bloodletting does not work to cure human-related witchcraft ailments. [25]
- Bloodletting is usually administered directly to the effected area, e.g. if the patient has a headache, a cut is made on the forehead. Out of 14 cultures with information on the localization of bloodletting, 11 at least sometimes removed blood from the affected area, while 3 specifically removed blood from a different area from the area in pain. Europe is the only continent with more instances of non-colocalized than colocalized bloodletting.
In a
Bloodletting as a concept is thought to be a cultural attractor, or an intrinsically attractive / culturally transmissible concept. This could explain bloodletting's independent cross-cultural emergence and common cross-cultural traits.[22]
Middle Ages
The
Use through the 19th century


Bloodletting became a main technique of heroic medicine, a traumatic and destructive collection of medical practices that emerged in the 18th century.[27]
Even after the humoral system fell into disuse, the practice was continued by

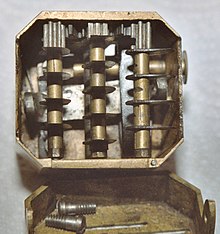


A number of different methods were employed. The most common was phlebotomy, or venesection (often called "breathing a vein"), in which blood was drawn from one or more of the larger external veins, such as those in the forearm or neck. In arteriotomy, an artery was punctured, although generally only in the temples. In scarification (not to be confused with
William Harvey disproved the basis of the practice in 1628,[2] and the introduction of scientific medicine, la méthode numérique, allowed Pierre Charles Alexandre Louis to demonstrate that phlebotomy was entirely ineffective in the treatment of pneumonia and various fevers in the 1830s. Nevertheless, in 1838, a lecturer at the Royal College of Physicians would still state that "blood-letting is a remedy which, when judiciously employed, it is hardly possible to estimate too highly",[28] and Louis was dogged by the sanguinary Broussais, who could recommend leeches fifty at a time. Some physicians resisted Louis' work because they "were not prepared to discard therapies 'validated by both tradition and their own experience on account of somebody else's numbers'."[29]
During this era, bloodletting was used to treat almost every disease. One British medical text recommended bloodletting for acne, asthma, cancer, cholera, coma, convulsions, diabetes, epilepsy, gangrene, gout, herpes, indigestion, insanity, jaundice, leprosy, ophthalmia, plague, pneumonia, scurvy, smallpox, stroke, tetanus, tuberculosis, and for some one hundred other diseases. Bloodletting was even used to treat most forms of hemorrhaging such as nosebleed, excessive menstruation, or hemorrhoidal bleeding. Before surgery or at the onset of childbirth, blood was removed to prevent inflammation. Before amputation, it was customary to remove a quantity of blood equal to the amount believed to circulate in the limb that was to be removed.[30]
There were also theories that bloodletting would cure "heartsickness" and "heartbreak". A French physician, Jacques Ferrand wrote a book in 1623 on the uses of bloodletting to cure a broken heart. He recommended bloodletting to the point of heart failure (literal).[31]
Leeches became especially popular in the early 19th century. In the 1830s, the French imported about 40 million leeches a year for medical purposes, and in the next decade, England imported 6 million leeches a year from France alone. Through the early decades of the century, hundreds of millions of leeches were used by physicians throughout Europe.[32]
Bloodletting was also popular in the young United States of America, where

One reason for the continued popularity of bloodletting (and purging) was that, while
Barbara Ehrenreich and Deirdre English write that the popularity of bloodletting and heroic medicine in general was because of a need to justify medical billing. Traditional healing techniques had been mostly practiced by women within a non-commercial family or village setting. As male doctors suppressed these techniques, they found it difficult to quantify various "amounts" of healing to charge for, and difficult to convince patients to pay for it. Because bloodletting seemed active and dramatic, it helped convince patients the doctor had something tangible to sell.[27]
Controversy and use into the 20th century
Bloodletting gradually declined in popularity over the course of the 19th century, becoming rather uncommon in most places, before its validity was thoroughly debated. In the medical community of
Some researchers used statistical methods for evaluating treatment effectiveness to discourage bloodletting.[35] But at the same time, publications by Philip Pye-Smith and others defended bloodletting on scientific grounds.[38]
Bloodletting persisted into the 20th century and was recommended in the 1923 edition of the textbook The Principles and Practice of Medicine.[40] The textbook was originally written by Sir William Osler and continued to be published in new editions under new authors following Osler's death in 1919.[41]
Phlebotomy
Bloodletting is used today in the treatment of a few diseases, including
In alternative medicine
Though bloodletting as a general health measure has been shown to be pseudoscience, it is still commonly indicated for a wide variety of conditions in the
Unani is based on a form of humorism, and so in that system, bloodletting is used to correct supposed humoral imbalance.See also
- Bloodstopping
- Blood donation
- Cupping therapy
- Hematology
- History of medicine
- Trepanation
- Humorism
- Fleams
- Panacea
References
- ^ "Bloodletting". British Science Museum. 2009. Archived from the original on 15 April 2009. Retrieved 12 July 2009.
- ^ ISBN 978-0226749365: The Ilex Press Limited, 2013.
- ^ Mestel, Rosie (6 August 2001). "Modern Bloodletting and Leeches". Los Angeles Times. Retrieved 12 July 2009.
- ^ "Why fair tests are needed". jameslindlibrary.org. 2009. Archived from the original on 2 January 2007. Retrieved 8 January 2017.
- ISBN 978-0-7668-2518-5. Retrieved 12 July 2009.
- ^ "The Basis of Therapeutic Phlebotomy". James C. Barton, M.D. 2009. Archived from the original on 8 April 2011. Retrieved 12 July 2009.
- ^ "Therapeutic Phlebotomy". Carteret General Hospital. 2009. Archived from the original on 7 July 2009. Retrieved 12 July 2009.
- ISBN 978-1135955298.
- PMID 21908152.
- S2CID 9589933.
- PMID 12800324.
- ^ Stern, Heinrich (1915). Theory and Practice of Bloodletting. New York: Rebman Company. p. 9. Retrieved 20 August 2018.
- hdl:10088/2440.
- ^ Kean, Sam (2018). "Sweating blood". Distillations. 4 (2): 5. Retrieved 20 August 2018.
- ISBN 978-0190655228. Retrieved 20 August 2018.
- ^ "Degeneration of Medicine and the Grisly Art of Slicing Open Arms". BBC. 29 November 2002. Retrieved 12 July 2009.
- ISBN 978-0-415-97334-2. Retrieved 12 July 2009.
- ISBN 0-19-513021-9.
- )
- )
- ^ ISBN 0-521-38135-5.
- ^ .
- PMID 11616622.
- JSTOR 3773194.
- S2CID 201473885, retrieved 17 July 2023
- ^ Talmud, b. Shabbat 129b
- ^ ISBN 1400078008.
- ^ Clutterbuck, Henry (1838). Dr Clutterbuck's Lectures On Bloodletting: Lecture 1. The London Medical Gazette.
- PMID 9204029.
- ^ Carter (2005) p. 6
- ^ Lydia Kang MD & Nate Pederson, Quackery: A Brief History of the Worst Ways to Cure Everything "Bleed Yourself to Bliss" (Workman Publishing Company; 2017)
- ^ Carter (2005) p. 7
- . quoted in Carter (2005):7–8
- ^ The Permanente Journal Volume 8 No. 2: The asphyxiating and exsanguinating death of president george washington Archived 22 October 2017 at the Wayback Machine, p. 79, Spring, 2004, retrieved on 11 November 2012
- ^ a b Greenstone, Gerry (January–February 2010). "The history of bloodletting". British Columbia Medical Journal. 52 (1). Retrieved 17 February 2017.
- S2CID 2028394.
- PMID 6997652.
- ^ .
Arguing that it was the physician's obligation to be active and to intervene when necessary, bloodletting proponents explicitly contrasted themselves with advocates of expectant treatment, whom they portrayed as passive, timid, and unwilling to do what was necessary to save their patients.
- PMC 2260507.
- ^ "Bloodletting". UCLA Library: Biomedical Library History and Special Collections for the Sciences. 12 January 2012. Archived from the original on 13 March 2012. Retrieved 5 January 2012.
- S2CID 41284621.
- ^ Tuttle, Kelly (2012). "Let it bleed". Science History Magazine. 30 (2): 17. Retrieved 20 August 2018.
- S2CID 19683918.
- S2CID 208791894.
- PMID 20228645.
- PMID 22736888.
- ^ Ayurveda – Panchakarma Archived 30 March 2013 at the Wayback Machine, holistic-online.com.
- ^ Ayurveda Archived 22 February 2014 at the Wayback Machine, Cancer.org.
- ^ Bleeding Peripheral Points: An Acupuncture Technique
- ^ Treating Herpes Zoster (Shingles) with Bloodletting Therapy: Acupuncture and Chinese Medicine Archived 2013-06-04 at the Wayback Machine
- PMID 21419074.
Books cited
- Carter, K. Codell; Barbara R. Carter (2005). Childbed fever. A scientific biography of Ignaz Semmelweis. Transaction Publishers. ISBN 978-1-4128-0467-7.
- Carter, K. Codell (2012). The Decline of Therapeutic Bloodletting and the Collapse of Traditional Medicine. New Brunswick & London: Transaction Publishers. ISBN 978-1-4128-4604-2.
- Kang, Lydia; Nate Pederson (2017). Quackery: A Brief History of the Worst Ways to Cure Everything. Workman Publishing Company.[ISBN missing]
Further reading
- McGrew, Roderick. Encyclopedia of Medical History (1985), brief history pp. 32–34[ISBN missing]
External links
- The History and Progression of Bloodletting
- Medical Antiques: Scarification and Bleeding
- Pictures of antique bloodletting instruments Archived 2 May 2012 at the Wayback Machine
- PBS's Red Gold: The Story of Blood
- Huge collection of antique bloodletting instruments
- "Breathing a Vein" Archived 14 September 2015 at the Wayback Machine phisick.com 14 Nov 2011
