Bone fracture
| Bone fracture | |
|---|---|
| Other names | broken bone, bone break |
MRI | |
A bone fracture (abbreviated FRX or Fx, Fx, or #) is a medical condition in which there is a partial or complete break in the continuity of any
Signs and symptoms
Although bone tissue contains no
- Breaking in the continuity of the periosteum, with or without similar discontinuity in endosteum, as both contain multiple pain receptors.
- soft tissues caused by ruptured bone marrowevokes pressure pain.
- Involuntary muscle spasmstrying to hold bone fragments in place.
Damage to adjacent structures such as nerves, muscles or blood vessels, spinal cord, and nerve roots (for spine fractures), or cranial contents (for skull fractures) may cause other specific signs and symptoms.[4]
Complications
Some fractures may lead to serious complications including a condition known as compartment syndrome. If not treated, eventually, compartment syndrome may require amputation of the affected limb. Other complications may include non-union, where the fractured bone fails to heal, or malunion, where the fractured bone heals in a deformed manner. One form of malunion is the malrotation of a bone, which is especially common after femoral and tibial fractures.[5] Complications of fractures may be classified into three broad groups, depending upon their time of occurrence. These are as follows –
- Immediate complications – occurs at the time of the fracture.
- Early complications – occurring in the initial few days after the fracture.
- Late complications – occurring a long time after the fracture.
| Immediate | Early | Late |
|---|---|---|
Systemic
|
Systemic
|
Imperfect union of the fracture
|
Local
|
Local
|
Others
|
Pathophysiology

The natural process of healing a fracture starts when the injured bone and surrounding tissues bleed, forming a fracture
At this stage, some of the fibroblasts begin to lay down
Several factors may help or hinder the bone healing process. For example, tobacco smoking hinders the process of bone healing,[7] and adequate nutrition (including calcium intake) will help the bone healing process. Weight-bearing stress on bone, after the bone has healed sufficiently to bear the weight, also builds bone strength.
Although there are theoretical concerns about
Effects of smoking
Smokers generally have lower bone density than non-smokers, so they have a much higher risk of fractures. There is also evidence that smoking delays bone healing.[9]
Diagnosis
A bone fracture may be diagnosed based on the history given and the physical examination performed.
Classification

(a) closed fracture
(b) open fracture
(c) transverse fracture
(d) spiral fracture
(e) comminuted fracture
(f) impacted fracture
(g) greenstick fracture
(h) oblique fracture


In orthopedic medicine, fractures are classified in various ways. Historically they are named after the physician who first described the fracture conditions, however, there are more systematic classifications as well.[citation needed]
They may be divided into stable versus unstable depending on the likelihood that they may shift further.[citation needed]
Mechanism
- Traumaticfracture – a fracture due to sustained trauma. e.g., fractures caused by a fall, road traffic accident, fight, etc.
- Pathologic fracture – a fracture through a bone that has been made weak by some underlying disease is called pathological fracture. e.g., a fracture through a bone weakened by metastasis. Osteoporosis is the most common cause of pathological fracture.
- Periprosthetic fracture – a fracture at the point of mechanical weakness at the end of an implant.
Soft-tissue involvement
- Closed/simple fractures are those in which the overlying skin is intact[10]
- Open/compound fractures involve wounds that communicate with the fracture, or where fracture hematoma is exposed, and may thus expose bone to contamination. Open injuries carry a higher risk of infection. Reports indicate an incidence of infection after internal fixation of closed fracture of 1-2%, rising to 30% in open fractures.[11]
- Clean fracture
- Contaminated fracture
Displacement
- Non-displaced
- Displaced
- Translated, or ad latus, with sideways displacement.[12]
- Angulated
- Rotated
- Shortened, a reduction in overall bone length when displaced fracture fragments overlap
Fracture pattern
- Linear fracture – a fracture that is parallel to the bone's long axis
- Transverse fracture – a fracture that is at a right angle to the bone's long axis
- Oblique fracture – a fracture that is diagonal to a bone's long axis (more than 30°)
- Spiral fracture – a fracture where at least one part of the bone has been twisted
- wedge fracture – usually occurs in the vertebrae, for example when the front portion of a vertebra in the spine collapses due to osteoporosis(a medical condition which causes bones to become brittle and susceptible to fracture, with or without trauma)
- Impacted fracture – a fracture caused when bone fragments are driven into each other
- Avulsion fracture – a fracture where a fragment of bone is separated from the main mass
Fragments
- Incomplete fracture – a fracture in which the bone fragments are still partially joined, in such cases, there is a crack in the osseous tissue that does not completely traverse the width of the bone.
- Complete fracture – a fracture in which bone fragments separate completely.
- Comminuted fracture – a fracture in which the bone has broken into several pieces.
Anatomical location
An anatomical classification may begin with specifying the involved body part, such as the head or arm, followed by more specific localization. Fractures that have additional definition criteria than merely localization often may be classified as subtypes of fractures, such as a
- Skull fracture
- Basilar skull fracture
- Blowout fracture – a fracture of the walls or floor of the orbit
- Mandibular fracture
- Nasal fracture
- maxillary boneand surrounding structures in a usually bilateral and either horizontal, pyramidal, or transverse way.
- Spinal fracture
- Cervical fracture
- Fracture of C1, including Jefferson fracture
- Fracture of C2, including Hangman's fracture
- Flexion teardrop fracture – a fracture of the anteroinferior aspect of a cervical vertebral
- spinous process of a vertebraoccurring at any of the lower cervical or upper thoracic vertebrae
- Burst fracture – in which a vertebra breaks from a high-energy axial load
- wedge fracturesdue to larger compression anteriorly
- Chance fracture – compression injury to the anterior portion of a vertebral body with concomitant distraction injury to posterior elements
- Holdsworth fracture – an unstable fracture dislocation of the thoraco lumbar junction of the spine
- Cervical fracture
- Rib fracture
- Sternal fracture
- Shoulder fracture
- Arm fracture
- Humerus fracture (fracture of upper arm)
- Supracondylar fracture
- entrapment of the radial nerve
- Forearm fracture
- Ulnar fracture
- head of the radius
- anterior dislocation of the radial head
- Radius fracture
- interosseous membrane[13]
- Distal radius fracture
- distal radioulnar joint
- Colles' fracture – a distal fracture of the radius with dorsal (posterior) displacement of the wrist and hand
- Smith's fracture – a distal fracture of the radius with volar (ventral) displacement of the wrist and hand
- radiocarpal joint
- Humerus fracture (fracture of upper arm)
- Hand fracture
- Scaphoid fracture
- metacarpalbone
- Bennett's fracture – a fracture of the base of the first metacarpal bone which extends into the carpometacarpal (CMC) joint [14]
- metacarpal
- Broken finger – a fracture of the carpal phalanges
- Pelvic fracture
- Fracture of the hip bone
- Duverney fracture – an isolated pelvic fracture involving only the iliac wing
- Femoral fracture
- Hip fracture (anatomically a fracture of the femur bone and not the hip bone)
- Patella fracture
- Crus fracture
- Tibia fracture
- Pilon fracture
- Tibial plateau fracture
- Segond fracture – an avulsion fracture of the lateral tibial condyle
- Gosselin fracture – a fractures of the tibial plafond into anterior and posterior fragments [15]
- Toddler's fracture – an undisplaced and spiral fracture of the distal third to distal half of the tibia [16]
- Fibular fracture
- Maisonneuve fracture – a spiral fracture of the proximal third of the fibula associated with a tear of the distal tibiofibular syndesmosis and the interosseous membrane
- anterior tibiofibular ligament[15]
- external rotation of the ankle [17]
- Combined tibia and fibula fracture
- medial malleolus, and the distal posterior aspect of the tibia
- Bimalleolar fracture – involving the lateral malleolus and the medial malleolus
- Pott's fracture
- Foot fracture
- fifth metatarsal
- March fracture – a fracture of the distal third of one of the metatarsals occurring because of recurrent stress
- Cuneiform fracture – a fracture of one of the three cuneiform bones typically due to direct blow, axial load, or avulsion [19]
- Calcaneal fracture – a fracture of the calcaneus (heel bone)
- Broken toe – a fracture of the pedal phalanges
OTA/AO classification
The Orthopaedic Trauma Association Committee for Coding and Classification published its classification system [20] in 1996, adopting a similar system to the 1987 AO Foundation system.[21] In 2007, they extended their system,[22] unifying the two systems regarding wrist, hand, foot, and ankle fractures.
Classifications named after people
A number of classifications are named after the person (
- "Denis classification" for spinal fractures [23]
- "radius and ulna)
- "Gustilo open fracture classification" [24]
- "Letournel and Judet Classification" for Acetabular fractures [25]
- "Neer classification" for humerus fractures [26][27]
Prevention
Both high- and low-force trauma can cause bone fracture injuries.
A common cause of low-force trauma is an at-home fall.
Some sports have a relatively high risk of bone fractures as a common
Taking calcium and vitamin D supplements can help strengthen your bones.[32] Vitamin D supplements combined with additional calcium marginally reduces the risk of hip fractures and other types of fracture in older adults; however, vitamin D supplementation alone did not reduce the risk of fractures.[33]
Patterns
| Photo | Type | Description | Causes | Effects |
|---|---|---|---|---|
 |
Linear fracture | Parallel to the bone's long axis | ||
 |
Transverse fracture | At a right angle to the bone's long axis | May occur when the bone is bent,[34]and snaps in the middle. | |
 |
Oblique fracture | Diagonal to a bone's long axis (more than 30°) | ||
 |
Spiral fracture or torsion fracture | At least one part of the bone has been twisted (image shows an arm-wrestler) | Torsion on the bone[34] | May rotate, and must be reduced to heal properly
|
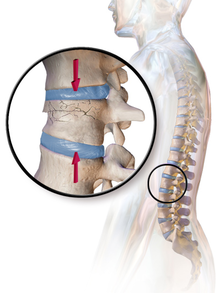 |
wedge fracture
|
Usually occurs in the vertebrae, for example when the front portion of a vertebra in the spine collapses due to osteoporosis (a medical condition which causes bones to become brittle and susceptible to fracture, with or without trauma) | ||
| Impacted fracture | Bone fragments are driven into each other | |||
 |
Avulsion fracture | A fragment of bone is separated from the main mass (image shows a Busch fracture) | ||
 |
Comminuted fracture
|
The bone is shattered | often from crushing injuries[34] |
Treatment



Treatment of bone fractures are broadly classified as surgical or conservative, the latter basically referring to any non-surgical procedure, such as pain management, immobilization or other non-surgical stabilization. A similar classification is open versus closed treatment, in which open treatment refers to any treatment in which the fracture site is opened surgically, regardless of whether the fracture is an open or closed fracture.[35]
Pain management
In arm fractures in children, ibuprofen has been found to be as effective as a combination of paracetamol and codeine.[36] In the EMS setting it might be applicable to administer 1mg/kg of iv ketamine to achieve a dissociated state.
Immobilization
Since
Occasionally smaller bones, such as phalanges of the
Splinting results in the same outcome as casting in children who have a distal radius fracture with little shifting.[38]
Surgery
Surgical methods of treating fractures have their own risks and benefits, but usually, surgery is performed only if conservative treatment has failed, is very likely to fail, or is likely to result in a poor functional outcome.[39] With some fractures such as hip fractures (usually caused by osteoporosis), surgery is offered routinely because non-operative treatment results in prolonged immobilisation, which commonly results in complications including chest infections, pressure sores, deconditioning, deep vein thrombosis (DVT), and pulmonary embolism, which are more dangerous than surgery.[40] When a joint surface is damaged by a fracture, surgery is also commonly recommended to make an accurate anatomical reduction and restore the smoothness of the joint.
Occasionally, bone grafting is used to treat a fracture.[41]
Sometimes bones are reinforced with metal. locally and may cause systemic effects as well.
Bone stimulation
Bone stimulation with either
Physical therapy
Physical therapy exercises (either home-based or physiotherapist-led) to improve functional mobility and strength, gait training for hip fractures, and other physical exercise are also often suggested to help recover physical capacities after a fracture has healed.[46][47]
Children
In children, whose bones are still developing, there are risks of either a growth plate injury or a greenstick fracture.
- A greenstick fracture occurs due to mechanical failure on the tension side. That is since the bone is not so brittle as it would be in an adult, it does not completely fracture, but rather exhibits bowing without complete disruption of the bone's cortex in the surface opposite the applied force.
- Growth plate injuries, as in Salter-Harris fractures, require careful treatment and accurate reduction to make sure that the bone continues to grow normally.
- Plastic deformation of the bone, in which the bone permanently bends, but does not break, also is possible in children. These injuries may require an osteotomy (bone cut) to realign the bone if it is fixed and cannot be realigned by closed methods.
- Certain fractures mainly occur in children, including fracture of the clavicle and supracondylar fracture of the humerus.[citation needed]
See also
- Stress fracture
- Distraction osteogenesis
- Rickets
- Catagmatic
- Orthopedic plaster casts
References
- ^ Katherine, Abel (2013). Official CPC Certification Study Guide. American Medical Association. p. 108.
- ISBN 978-0-323-40163-0.
- ^ MedicineNet – Fracture Archived 2008-12-21 at the Wayback Machine Medical Author: Benjamin C. Wedro, MD, FAAEM.
- ^ Danielle Campagne (September 2022). "Overview of Fractures". mdmanuals.com.
- ^ "Compartment Syndrome". The Lecturio Medical Concept Library. Retrieved 25 June 2021.
- ^ Silva, Joana Cavaco (11 July 2018). "Bone fracture repair: Procedures, risks, and healing time". Medical News Today. William Morrison, M.D. (medical reviewer). Retrieved 21 April 2022.
- PMID 20303894.
- PMID 22272177.
- S2CID 19890259.
- ^ "Simple fracture | pathology". Encyclopedia Britannica. Retrieved 19 May 2021.
- S2CID 12894601.
- ^ Roberto Schubert. "Fractures of the extremities (general rules and nomenclature)". Radiopaedia. Retrieved 21 February 2018.
- ^ Essex Lopresti fracture Archived 2009-10-01 at the Wayback Machine at Wheeless' Textbook of Orthopaedics online
- ^ "Bennett's fracture-subluxation". GPnotebook.
- ^ PMID 10835130.
- PMID 10532655.
- PMID 6630259.[permanent dead link]
- ^ TheFreeDictionary Lisfranc's fracture Citing: Mosby's Medical Dictionary, 8th edition. Copyright 2009
- S2CID 225705519.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - PMID 8814583.
- ^ Müller ME, Nazarian S, Koch P (1987). Classification AO des fractures. Tome I. Les os longs. Berlin: Springer-Verlag.[page needed]
- S2CID 24535478.
- ^ "Denis classification of spinal fractures". GPnotebook.
- ISBN 978-3-13-117442-0.
- ^ "Fractures of the Acetabulum". wheelessonline.com. Archived from the original on 26 September 2009.
- PMID 9155417.
- ^ Proximal Humerus Fractures at eMedicine
- ^ "Hip Fractures". The Lecturio Medical Concept Library. Retrieved 24 July 2021.
- ^ a b "Open Fractures - OrthoInfo - AAOS". Retrieved 3 December 2018.
- ^ PMID 22204774.
- ^ PMID 28958365.
- ^ a b c d "Preventing Falls and Related Fractures | NIH Osteoporosis and Related Bone Diseases National Resource Center". www.bones.nih.gov. Retrieved 3 December 2018.
- PMID 24729336.
- ^ PMID 32491557– via PubMed.
- ^ "Overview of Bone Fractures". The Lecturio Medical Concept Library. Retrieved 25 July 2021.
- PMID 19692147.
- S2CID 31890854.
- PMID 20823169.
- ^ "Fractures". Johns Hopkins Medicine. 28 February 2020. Retrieved 25 July 2021.
- ^ "Hip Fractures". The Lecturio Medical Concept Library. Retrieved 24 July 2021.
- ISBN 9780721683317.
- ^ "Fractures". Johns Hopkins Medicine. 28 February 2020. Retrieved 25 July 2021.
- ^ PMID 28532896.
- PMID 19838359.
- PMID 36866917.
- PMID 35421234.
- PMID 36070134.
External links
- Authoritative information in orthopaedic surgery American Association of Orthopedic Surgeons (AAOS)
- Radiographic Atlas of Fracture
