Bone resorption
| Bone Resorption | |
|---|---|
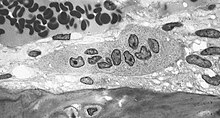 | |
| Light micrograph of an osteoclast displaying typical distinguishing characteristics: a large cell with multiple nuclei and a "foamy" cytosol. | |
| Specialty | Rheumatology |
Bone resorption is
The osteoclasts are multi-nucleated
The human body is in a constant state of
Bone resorption rates are much higher in post-menopausal older women due to estrogen deficiency related with
Regulation
Bone resorption is highly stimulated or inhibited by signals from other parts of the body, depending on the demand for calcium.
Calcium-sensing membrane receptors in the parathyroid gland monitor calcium levels in the extracellular fluid. Low levels of calcium stimulates the release of parathyroid hormone (PTH) from chief cells of the parathyroid gland.[4] In addition to its effects on kidney and intestine, PTH increases the number and activity of osteoclasts. The increase in activity of already existing osteoclasts is the initial effect of PTH, and begins in minutes and increases over a few hours.[4] Continued elevation of PTH levels increases the abundance of osteoclasts. This leads to a greater resorption of calcium and phosphate ions.[4]
High levels of calcium in the blood, on the other hand, leads to decreased PTH release from the parathyroid gland, decreasing the number and activity of osteoclasts, resulting in less bone resorption. Vitamin D increases absorption of calcium and phosphate in the intestinal tract, leading to elevated levels of plasma calcium,[4] and thus lower bone resorption.
Calcitriol (1,25-dihydroxycholecalciferol) is the active form of vitamin D3.[10] It has numerous functions involved in blood calcium levels. Recent research indicates that calcitriol leads to a reduction in osteoclast formation, and bone resorption.[11][12] It follows that an increase in vitamin D3 intake should lead to a decrease in bone resorption — it has been shown that oral administration of vitamin D does not linearly correlate to increased serum levels of calcifediol,[13] the precursor to calcitriol.
Calcitonin is a hormone secreted by the thyroid in humans. Calcitonin decreases osteoclast activity, and decreases the formation of new osteoclasts, resulting in decreased resorption.[4] Calcitonin has a greater effect in young children than in adults, and plays a smaller role in bone remodeling than PTH.[4]
In some cases where bone resorption outpaces ossification, the bone is broken down much faster than it can be renewed. The bone becomes more porous and fragile, exposing people to the risk of fractures. Depending on where in the body bone resorption occurs, additional problems like tooth loss can arise. This can be caused by conditions such as
Some people who experience increased bone resorption and decreased bone formation are
Alcoholism
The effects of alcohol on
Growth hormone is an important regulator of bone growth and remodeling in adults, and it acts via insulin-like growth factor I (
Increasing alcohol consumption is linked with decreasing testosterone and serum estradiol levels, which in turn lead to the activation of RANK (a TNF receptor) protein that promote osteoclast formation.[16] Oxidative stress results when ethanol induces NOX expression, resulting in ROS production in osteoblasts which can ultimately result in cell senescence.[17] Direct effects of chronic alcoholism are apparent in osteoblasts, osteoclasts and osteocytes. Ethanol suppresses the activity and differentiation of osteoblasts.
At the same time, it has a direct effect on osteoclast activity. This results in an increased bone resorption rate and a decreased bone mineral density due to increased pit numbers and pit areas in the bone.[18][19][20] Research has shown that viable osteocytes (another type of bone cell) may prevent osteoclastogenesis, whereas apoptotic osteocytes tend to induce osteoclast stimulation. Stimulation of osteocyte apoptosis by alcohol exposure may explain decreased bone mineral density in chronic drinkers.[20][6]
Clinical importance
Bone resorption is an integral part of both physiological and pathological processes.[21]
Pathological bone resorption could be limited (local) which is induced by local inflammation,[22] for example, trauma or infection, resorption activated local factors, including growth factors, cytokines, prostaglandins, etc., are simultaneously triggered. This bone resorption could also be observed in patients with many metabolic skeleton diseases, especially osteopenia and osteoporosis, endocrine diseases, rheumatic disorders, and other cases, as well as in patients with genetic disorders.
Physiological bone resorption is an integral part of bone functioning, while the bone is constantly growing thanks to two processes — breakdown and formation of bone tissue.[23] Locally, it could be manifested in tooth eruption when the movement of a tooth follicle is followed by an active resorption of jaw bone tissue. Resorption of old bone and formation of a new one are balanced in a well-developed skeleton. However, resorption starts taking a large part in remodeling processes with age. Dentistry sees resorption as dissolution or breakdown of a tooth structure. This could be inflammation and dentine or cement loss.
Bone tissue is a dynamic system with active metabolism.[24] Bone tissue remodelling or bone remodeling is a successive chain of old bone matrix removal and its replacement with a new one.[25] These processes make a child’s skeleton grow and extend, while childhood is characterized by bone tissue growth rather than its resorption.
See also
- Bone remodeling
- Nuclear factor-kappa B
References
- ^ Bone+Resorption at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- PMID 10968780.
- PMID 18662512.
- ^ ISBN 978-1-4160-4574-8.
- ^ PMID 18988698.
- ^ PMID 21689804.
- PMID 20936937.
- )
- PMID 25374469.
- S2CID 58721779.
- PMID 23569273.
- PMID 23389957.
- S2CID 9326591.
- PMID 16077253.
- ^ S2CID 11502836.
- PMID 17559547.
- S2CID 27152788.
- PMID 32040934.
- PMID 21254230.
- ^ S2CID 22428635.
- PMID 16505794.
- PMID 33584321.
- )
- PMID 35953935.
- ISBN 9780123694430.
Bone remodeling describes the process whereby old bone is continuously replaced by new tissue.
