Gastrointestinal perforation
| Gastrointestinal perforation | |
|---|---|
| Other names | Ruptured bowel, antibiotics[2] |
Gastrointestinal perforation, also known as gastrointestinal rupture,[1] is a hole in the wall of the gastrointestinal tract. The gastrointestinal tract is composed of hollow digestive organs leading from the mouth to the anus.[3] Symptoms of gastrointestinal perforation commonly include severe abdominal pain, nausea, and vomiting.[2] Complications include a painful inflammation of the inner lining of the abdominal wall and sepsis.
Perforation may be caused by
Perforation anywhere along the gastrointestinal tract typically requires
Signs and symptoms
Gastrointestinal perforation results in sudden, severe abdominal pain at the site of perforation, which then spreads across the abdomen.[5] The pain is intensified by movement. Nausea, vomiting, hematemesis, and increased heart rate are common early symptoms. Later symptoms include fever and or chills.[6] On examination, the abdomen is rigid and tender.[1] After some time, the bowel stops moving, and the abdomen becomes silent and distended.
The symptoms of esophageal rupture may include sudden onset of chest pain.
Complications
A hole in the intestinal tracts allows intestinal contents to enter the abdominal cavity.[2] The entry of bacteria from the gastrointestinal tract into the abdomen results in peritonitis or in the formation of an abscess.[2]
Patients may develop sepsis, a life-threatening response to infection, which may appear as an increased heart rate, increased breathing rate, fever, and confusion.[2] This may progress to multi-level organ dysfunction, including acute respiratory and kidney failure.[5]
Posterior gastric wall perforation may lead to bleeding due to the involvement of gastroduodenal artery that lies behind the first part of the duodenum.[7] The death rate in this case is 20%.[7]
Causes
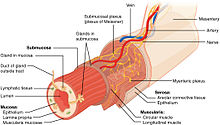
Gastrointestinal perforation is defined by a full-thickness injury to all layers of the gastrointestinal wall, resulting in a hole in the hollow GI tract (esophagus, stomach, small intestine, or large intestine). A hole can occur due to direct mechanical injury or progressive damage to the bowel wall due to various disease states.
Trauma or accidental perforations during medical procedures
Penetrating trauma such as from a knife or gunshot wound can puncture the bowel wall. Additionally, blunt trauma, such as in a motor vehicle accident may abruptly increase the pressure within the bowel, resulting in bowel rupture. Perforation can also be a very rare complication of certain medical procedures such as upper gastrointestinal endoscopy and colonoscopy.[8]
Infection or inflammatory disease
Bowel obstruction
Eating multiple
Erosion
A
Indirect causes
An often overlooked indirect cause of obstruction leading to perforation is the chronic use of opioids, which can create severe constipation and damage to the colon, often termed stercoral perforation.[18]
Diagnosis
A hole in the gastrointestinal tract causes leakage of gas into the abdominal cavity. In intestinal perforation, gas may be visible under the
White blood cells and blood lactate levels may also be elevated, particularly in the case of advanced disease including peritonitis and sepsis.[20]
Differential diagnoses of gastrointestinal perforation includes other causes of an
Treatment
Conservative treatment (avoiding surgery) may be sufficient in the case of a contained perforation. It is indicated only if the person has normal vital signs and is clinically stable.[21]
Regardless of whether surgery is performed, all patients are offered pain therapy and placed on bowel rest (avoiding all food and fluids by mouth),
References
- ^ ISBN 9781451188509. Archivedfrom the original on 17 August 2016. Retrieved 4 August 2016.
- ^ PMID 18387378.
- PMID 18387378.
- ISBN 978-1455738076. Archivedfrom the original on 2016-08-17.
- ^ PMID 26692573.
- ^ Ansari, Parswa. "Acute Perforation". Merck Manuals. Archived from the original on July 10, 2016. Retrieved June 30, 2016.
- ^ S2CID 4547048.
- PMID 20101766.
- ^ "Definition & Facts for Appendicitis - NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved 2023-11-15.
- PMID 18387378.
- ISBN 978-1-4051-7025-3, retrieved 2023-11-15
- ISBN 9783319405254.
- PMID 18387378.
- PMID 30137838, retrieved 2023-11-15
- PMID 11161072.
- PMID 24267289.
- PMID 12869880.
- PMID 29232630.
- PMID 26692573.
- PMID 22202128.
- ^ PMID 24449533.
- S2CID 38323381.
- ^ "Gastrointestinal perforation Information | Mount Sinai - New York". Mount Sinai Health System. Retrieved 2023-11-03.
- PMID 15846719.
- ISBN 9781420015263. Archivedfrom the original on 2016-08-17.
