Bradycardia
| Bradycardia | |
|---|---|
| Other names | Bradyarrhythmia, brachycardia |
electrocardiogram | |
| Frequency | 15% (males), 7% (females) |
Bradycardia, also called bradyarrhythmia, is a
Bradycardia may be associated with symptoms of
The management of bradycardia is generally reserved for patients with symptoms, regardless of minimum heart rate during sleep or the presence of concomitant heart rhythm abnormalities (See:
The term "relative bradycardia" can refer to a heart rate lower than expected in a particular disease state, often a febrile illness.[10] "Chronotropic incompetence" (CI) refers to an inadequate rise in heart rate during periods of increased demand, often due to exercise, and is an important sign of SND and an indication for pacemaker implantation.[8][7]
The word "bradycardia" is from the Greek βραδύς bradys "slow", and καρδία kardia "heart".[11]
Normal cardiac conduction
The heart is a specialized muscle containing repeating units of cardiomyocytes, or heart muscle cells. Like most cells, cardiomyocytes maintain a highly regulated negative voltage at rest and are capable of propagating action potentials, much like neurons.[12] While at rest, the negative cellular voltage of a cardiomyocyte can be raised above a certain threshold (so-called depolarization) by an incoming action potential, causing the myocyte to contract. When these contractions occur in a coordinated fashion, the atria and ventricles of the heart will pump, delivering blood to the rest of the body.[12]
Normally, the origination of the action potential causing cardiomyocyte contraction originates from the sinoatrial node (SA node). This collection of specialized conduction tissue is located in the right atrium, near the entrance of the superior vena cava.[13] The SA node contains pacemaker cells that demonstrate "automaticity" and can generate impulses that travel through the heart and create a steady heartbeat.[13]
At the beginning of the cardiac cycle, the SA node generates an electrical action potential that spreads across the right and left atria, causing the atrial contraction of the cardiac cycle.[13] This electrical impulse carries on to the atrioventricular node (AV node), another specialized grouping of cells located in the base of the right atrium, which is the only anatomically normal electrical connection between the atria and ventricles. Impulses coursing through the AV node are slowed before carrying on to the ventricles,[14] allowing for appropriate filling of the ventricles before contraction. The SA and AV nodes are both closely regulated by the autonomic nervous system's fibres, allowing for adjustment of cardiac output by the central nervous system in times of increased metabolic demand.
Following slowed conduction through the atrioventricular node, the action potential produced initially at the SA node now flows through the His-Purkinje system. The bundle of His originates in the AV node and rapidly splits into a left and right branch, each destined for a different ventricle. Finally, these bundle branches terminate in the small Purkinje fibers that innervate myocardial tissue. The His-Purkinje system conducts action potentials much faster than can be propagated between myocardial cells, allowing the entire ventricular myocardium to contract in less time, improving pump function.[13]
Classification

Most pathological causes of bradycardia result from damage to this normal cardiac conduction system at various levels: the sinoatrial node, the atrioventricular node, or damage to conduction tissue between or after these nodes.
Sinus node
Bradycardia caused by the alterations of sinus node activity is divided into three types.
Sinus bradycardia
Sinus bradycardia is a sinus rhythm of less than 50 BPM.[15] Cardiac action potentials are generated from the SA node and propagated through an otherwise normal conduction system, but they occur at a slow rate. It is a common condition found in both healthy individuals and those considered well-conditioned athletes.[1] Studies have found that 50–85% of conditioned athletes have benign sinus bradycardia, as compared to 23% of the general population studied.[16] The heart muscle of athletes has a higher stroke volume, requiring fewer contractions to circulate the same volume of blood.[17] Asymptomatic sinus bradycardia decreases in prevalence with age.
Sinus arrhythmia
Sinus arrhythmias are heart rhythm abnormalities characterized by variations in the cardiac cycle length over 120 milliseconds (longest cycle - shortest cycle).[7] These are the most common type of arrhythmia in the general population and usually have no significant consequences. They typically occur in the young, athletes or after administration of medications such as morphine. The types of sinus arrhythmia are separated into the respiratory and non-respiratory categories.[7]
Respiratory sinus arrhythmia
Respiratory sinus arrhythmia refers to the physiologically normal variation in heart rate due to breathing. During inspiration, vagus nerve activity decreases, reducing parasympathetic innervation of the sinoatrial node and causing an increase in heart rate. During expiration, heart rates fall due to the converse occurring.[7]
Non-respiratory sinus arrhythmia
Non-respiratory causes of sinus arrhythmia include sinus pause, sinus arrest, and sinoatrial exit block. Sinus pause and arrest involve slowing or arresting of automatic impulse generation from the sinus node. This can lead to asystole or cardiac arrest if ventricular escape rhythms do not create backup sources of cardiac action potentials.[7]
Sinoatrial exit block is a similar non-respiratory phenomenon of temporarily lost sinoatrial impulses. However, in contrast to a sinus pause, the action potential is still generated at the SA node but is either unable to leave or delayed from leaving the node, preventing or delaying atrial depolarization and subsequent ventricular systole. Therefore, the length of the pause in heartbeats is usually a multiple of the P-P interval, as seen on electrocardiography. Like a sinus pause, a sinoatrial exit block can be symptomatic, especially with prolonged pause length.[7]
Sinus node dysfunction
A syndrome of intrinsic disease of the sinus node, referred to as sick sinus syndrome or
Atrioventricular node
Bradycardia can also result from the inhibition of the flow of action potentials through the atrioventricular (AV) node. While this can be normal in young patients due to excessive vagus nerve tone, symptomatic bradycardia due to AV node dysfunction in older people is commonly due to structural heart disease, myocardial ischemia, or age-related fibrosis.[19]
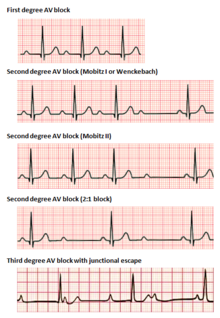
Atrioventricular block
Atrioventricular blocks are divided into three categories, ranked by severity. AV block is diagnosed via surface ECG, which is usually sufficient to locate the causal lesion of the block without the need for an invasive electrophysiology study.[7]
In 1st degree AV block, electrical impulses originating in the SA node (or other ectopic focus above the ventricles) are conducted with significant delay through the AV node. This condition is diagnosed via ECG, with PR intervals in excess of 200 milliseconds.[7] The PR interval represents the length of time between the start of atrial depolarization and the start of ventricular depolarization, representing the flow of electrical impulses between the SA and AV nodes. Despite the term "block," no impulses are fully lost in this conduction but are merely delayed. The location of the causal lesion can be anywhere between the AV node and the His-Purkinje system but is most commonly found in the AV node itself.[20] Generally, isolated PR prolongation in 1st degree AV block is not associated with increased mortality or hospitalization.[21]
2nd degree AV block is characterized by intermittently lost conduction of impulses between the SA node and the ventricles. 2nd degree block is classified into two types. Mobitz type 1 block, otherwise known by the eponym Wenckebach, classically demonstrates grouped patterns of heartbeats on ECG. Throughout the group, the PR interval gradually lengthens until a dropped conduction occurs, resulting in no QRS complex seen on surface ECG following the last P wave. After a delay, the grouping repeats, with the PR interval shortening again to baseline.[22] Type 1 2nd degree AV block due to disease in the AV node (as opposed to in the His-purkinje system) rarely needs intervention with pacemaker implantation.[22]
2nd degree, Mobitz type 2 AV block is another phenomenon of intermittently dropped QRS complexes after characteristic groupings of beats seen on surface ECG. The PR and RR intervals are consistent in this condition, followed by a sudden AV block and dropped QRS complex.[22] Because type 2 blocks are typically due to lesions below the AV node, the ability for ventricular escape rhythms to maintain cardiac output is compromised. Permanent pacemaker implantation is often required.[19]
Junctional rhythms
An
An AV-junctional escape beat is a delayed heartbeat originating from an
Ventricular
Infantile
For infants, bradycardia is defined as a heart rate less than 100 BPM (normal is around 120–160 BPM). Premature babies are more likely than full-term babies to have apnea and bradycardia spells; their cause is not clearly understood. The spells may be related to centers inside the brain that regulate breathing which may not be fully developed. Touching the baby gently or rocking the incubator slightly will almost always get the baby to start breathing again, which increases the heart rate. The
Causes
Bradycardia arrhythmia may have many causes, both cardiac and non-cardiac.
Non-cardiac causes are usually secondary and can involve
Cardiac causes include acute or chronic
In general, two types of problems result in bradycardias: disorders of the SA node and disorders of the AV node.[29]
With SA node dysfunction (sometimes called sick sinus syndrome), there may be disordered automaticity or impaired conduction of the impulse from the SA node into the surrounding atrial tissue (an "exit block"). Second-degree sinoatrial blocks can be detected only by use of a 12-lead ECG.
AV conduction disturbances (AV block;
Diagnosis
A diagnosis of bradycardia in adults is based on a heart rate of less than 60 BPM,[1] although some studies use a heart rate of less than 50 BPM.[33] This is usually determined either by palpation or ECG.[1] If symptoms occur, a determining electrolytes may help determine the underlying cause.[31]
Management
The treatment of bradycardia depends on whether the person is stable or unstable.[1][33]
Stable
Emergency treatment is not needed if the person is asymptomatic or minimally symptomatic.[33]
Unstable
If a person is unstable, the initial recommended treatment is intravenous
In children, giving oxygen, supporting their breathing, and
Epidemiology
This section needs expansion with: discussion regarding the threshold of 60 bpm. You can help by adding to it. (December 2018) |
In clinical practice, elderly people over age 65 and young athletes of both sexes may have sinus bradycardia.
Society and culture
Records
- Daniel Green holds the world record for the slowest heartbeat in a healthy human, with a heart rate measured in 2014 of 26 BPM.[37]
- Martin Brady holds the Guinness world record for the slowest heart rate, with a certified rate over a minute duration of 27 BPM.[38]
- During his career, professional cyclist Miguel Indurain had a resting heart rate of 28 BPM.[39]
See also
- Bezold–Jarisch reflex – Processes which cause hypopnea
References
- ^ PMID 29630253. Retrieved 16 January 2022.
- ISBN 978-0-323-82467-5.
- PMID 25194872.
- ^ Rijnbeek, Peter R. (2012). "Normal ECG values". Rotterdam, The Netherlands.
- PMID 30586772.
- ^ PMID 31311698.
- ^ ISBN 978-0-323-82467-5.
- ^ PMID 30586772.
- PMID 9832095.
- PMID 30048576.
- ISBN 9780471681830.
- ^ a b Loscalzo, Joseph; Keaney, John F.; MacRae, Calum A. (2022). "Basic Biology of the Cardiovascular System". Harrison's Principles of Internal Medicine (21st ed.). McGraw Hill.
- ^ a b c d Sauer, William H.; Koplan, Bruce A.; Zei, Paul C. (2022). "Principles of Clinical Cardiac Electrophysiology". Harrison's Principles of Internal Medicine (21st ed.). McGraw Hill.
- PMID 20180918.
- PMID 30586772.
- PMID 1591784.
- ^ ISBN 978-0-7817-5125-4.
- PMID 27166347.
- ^ a b Sauer, William H.; Koplan, Bruce A. (2022). "The Bradyarrhythmias: Disorders of the Atrioventricular Node". Harrison's Principles of Internal Medicine (21st ed.). McGraw Hill.
- S2CID 239091592.
- PMID 23677846.
- ^ S2CID 239091592.
- ^ "AV Junctional Rhythm Disturbances (for Professionals)". American Heart Association. 4 December 2008. Retrieved 15 December 2009.
- ^ a b "Arrhythmias and Conduction Disorders". The Merck Manuals: Online Medical Library. Merck Sharp and Dohme Corp. January 2008. Retrieved 16 December 2009.
- ^ PMID 14503433.
- PMID 30048576.
- PMID 10577999.
- ^ a b "What is Bradycardia?". WebMD. Retrieved 5 July 2021.
- ^ "Bradyarrhythmias". The Lecturio Medical Concept Library. Retrieved 5 July 2021.
- ^ PMID 16308110.
- ^ a b "What is Bradycardia?". WebMD. Retrieved 5 July 2021.
- PMID 23997188.
- ^ PMID 20956224.
- PMID 26473000.
- PMID 26472999.
- ^ Yechiam Ostchega; et al. (24 August 2011). "Resting Pulse Rate Reference Data for Children, Adolescents, and Adults: United States, 1999–2008" (PDF). National Health Statistics Reports. Centers for Disease Control. Archived (PDF) from the original on 10 October 2022. Retrieved 15 December 2018.
- ^ "Slowest heart rate: Daniel Green breaks Guinness World Records record". World Record Academy. 29 November 2014. Retrieved 5 August 2015.
- ^ "Lowest heart rate". Guinness World Records. 11 August 2005. Retrieved 5 August 2015.
- ^ Lovgren, Stefan (20 August 2004). "Olympic Gold Begins With Good Genes, Experts Say". National Geographic News. Archived from the original on 20 August 2004. Retrieved 8 September 2014.
