Brain metastasis
A brain metastasis is a
Symptoms and signs
Because different parts of the brain are responsible for different functions, symptoms vary depending on the site of metastasis within the brain. However, brain metastases should be considered in any cancer patient who presents with neurological or behavioral changes.[6]
Brain metastases can cause a wide variety of symptoms which can also be present in minor, more common conditions. Neurological symptoms are often caused by
The most common neurological symptoms include:- New onset headaches: headaches occur in roughly half of brain metastasis patients, especially in those with many tumors.[6]
- Paresthesias: patients often present with (hemiparesis), or weakness on only one side of the body, which is often a result of damage to neighboring brain tissue.[7]
- Ataxia: when metastasis occurs to the cerebellum, patients will experience various difficulties with spatial awareness and coordination.[9]
- Seizures: when present, often indicates disease involvement of the cerebral cortex.[10]
Causes
The most common sources of brain metastases in a
- Lung cancer, 48%
- Breast cancer, 15%
- Genitourinary tract cancers, 11%
- Osteosarcoma, 10%
- Melanoma, 9%
- Head and neck cancer, 6%
- Neuroblastoma, 5%
- pancreatic carcinoma, 3%
- Lymphoma, 1%
Lung cancer and melanoma are most likely to present with multiple metastasis, whereas breast, colon, and renal cancers are more likely to present with a single metastasis.[3]
Diagnosis

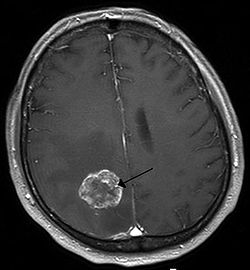
Brain imaging (
The diagnosis of brain metastases typically follows a diagnosis of a primary cancer.[10] Occasionally, brain metastases will be diagnosed concurrently with a primary tumor or before the primary tumor is found.
In the setting of brain metastasis due to malignant melanoma, MRI imaging showed high T1 and low T2 intensity due to the deposition of melanin in the brain. In susceptibility weighted imaging (SWI), it usually shows abnormal SWI hypointensity in larger proportion than brain metastasis caused by breast carcinoma.[12]
Treatment
Treatment for brain metastases is primarily
Symptomatic care
Symptomatic care should be given to all patients with brain metastases, as they often cause severe, debilitating symptoms. Treatment consists mainly of:
- emesis. Dexamethasone is the corticosteroid of choice.[10] Although neurological symptoms may improve within 24 to 72 hours of starting corticosteroids, cerebral edema may not improve for up to a week.[15] In addition, patients may experience adverse side effects from these drugs, such as myopathy and opportunistic infections, which can be alleviated by decreasing the dose.[15]
- Anticonvulsants – Anticonvulsants should be used for patients with brain metastases who experience seizures, as there is a risk of status epilepticus and death.[16] Newer generation anticonvulsants including Lamotrigine and Topiramate are recommended due to their relatively limited side effects.[16] It is not recommended to prophylactically give anti-seizure medications when a seizure has not yet been experienced by a patient with brain metastasis.[16]
Radiotherapy
Surgery
Brain metastases are often managed surgically if they are accessible. Surgical resection followed by
Chemotherapy
Immunotherapy
Prognosis
The prognosis for brain metastases is variable; it depends on the type of primary cancer, the age of the patient, the absence or presence of extracranial metastases, and the number of metastatic sites in the brain.
Epidemiology
It is estimated that the worldwide
More cases of brain metastases were found in
Both population studies and autopsy studies have historically been used to calculate the incidence of brain metastases. However, many researchers have stated that population studies may express inaccurate data for brain metastases, given that surgeons have, in the past, been hesitant to take in patients with the condition. As a result, population studies regarding brain metastases have historically been inaccurate and incomplete.[39][40]
Advances in systemic treatments of brain metastases, such as
See also
References
- ^ S2CID 236256085.
- ^ a b c d Tse V (10 November 2009). "Brain Metastasis". Medscape. Retrieved 13 January 2010.
- ^ a b "Metastatic Brain Tumors" (PDF). Archived from the original (PDF) on 29 August 2017. Retrieved 13 August 2017.
- ^ "Tumor Types - National Brain Tumor Society". National Brain Tumor Society. Retrieved 1 August 2017.[permanent dead link]
- ^ "Radiation Therapy for Brain Metastases: What are brain metastases?". Archived from the original on 2010-04-06. Retrieved 2010-03-17.
- ^ a b c d e f g h i j Loeffler JS. Wen PY, Eichler AF (eds.). "Epidemiology, clinical manifestations, and diagnosis of brain metastases". UpToDate. Retrieved 2 August 2017.
- ^ PMID 11589063. Archived from the originalon 2022-10-04. Retrieved 2017-08-13.
- ^ "Metastatic Brain Tumors". American Association of Neurological Surgeons. Retrieved 3 August 2017.
- ^ "Metastatic Brain Tumors". Memorial Sloan Kettering Cancer Center. Retrieved 3 August 2017.
- ^ PMID 10442342.
- ^ Ts V (10 November 2009). "Brain Metastasis - Morbidity/Mortality". Medscape. Retrieved 13 January 2010.
- PMID 29307364.
- PMID 30053879.
- PMID 36435874.
- ^ a b Drappatz J. Wen PY, Eichler AF (eds.). "Management of Vasogenic Edema in Patients with Primary and Metastatic Brain Tumors". UpToDate. Retrieved 2 August 2017.
- ^ a b c Drappatz J. Avila EK, Schachter SC, Wen PY, Dashe JF (eds.). "Seizures in Patients with Primary and Metastatic Brain Tumors". UpToDate. Retrieved 2 August 2017.
- ^ Loeffler JS. Wen PY, Eichler AF (eds.). "Overview of the Treatment of Brain Metastases". UpToDate. Retrieved 2 August 2017.
- ^ "What are the real benefits versus risks of preventative brain radiation for patients with non-small cell lung cancer?" (PDF). Archived from the original (PDF) on 2010-06-13. Retrieved 2010-03-17.
- ^ "IIS7". Archived from the original on 2010-01-29. Retrieved 2010-01-16.
- PMID 22696370.
- ^ "Definition of intrathecal chemotherapy". 2011-02-02. Retrieved 2017-08-13.
- PMID 24998288.
- ^ "FDA approves new oral therapy to treat ALK-positive lung cancer". FDA. 11 December 2015. Retrieved 4 August 2017.
- S2CID 3782427.
- S2CID 250343194.
- PMID 36435874.
- PMID 38386085.
- ISBN 9780470753064
- OCLC 805657369.
- PMID 15254054.
- PMID 23717790.
- PMID 9010115.
- PMID 8708681.
- PMID 21244695.
- S2CID 19575548.
- PMID 10098435.
- S2CID 23306094.
- PMID 15254054.
- S2CID 20786479.
- S2CID 43324791.
- PMID 24311640.
