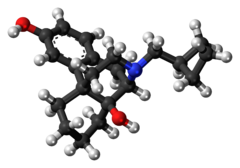
Butorphanol
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Stadol, others |
| Other names | BC 2627 |
| AHFS/Drugs.com | Micromedex Detailed Consumer Information |
| MedlinePlus | a682667 |
| Pregnancy category |
|
| Routes of administration | IV, intranasal, oral |
| ATC code | |
| Legal status | |
| Legal status |
|
Fecal , 15% | |
| Identifiers | |
| |
JSmol) | |
| |
| |
| | |
Butorphanol is a
It was patented in 1971 and approved for medical use in 1979.[7]
Medical uses
The most common indication for butorphanol is management of
Pharmacology
Butorphanol exhibits
Side effects
As with other opioid analgesics, central nervous system effects (such as
are common. Less common are the gastrointestinal effects of other opioids (mostly constipation). Another side effect experienced by people taking the medication is increased perspiration.Name
Within the
Its tradename Stadol was recently discontinued by the manufacturer. It is now only available in its generic formulations manufactured by Apotex, Mylan, Novex and Ben Venue Laboratories.
Availability
Butorphanol is available in the U.S. as a generic drug; it is available in various nations under one of any number of trade names, including Moradol and Beforal (Brand name Stadol no longer available in the US); veterinary trade names include Butorphic, Dolorex, Morphasol, Torbugesic, and Torbutrol.
Legality
Butorphanol is listed under the Single Convention on Narcotic Drugs 1961 and in the United States is a Schedule IV Narcotic controlled substance with a DEA ACSCN of 9720; being in Schedule IV it is not subject to annual aggregate manufacturing quotas. The free base conversion ratio of the hydrochloride is 0.69.[11] Butorphanol was originally in Schedule II and at one point it was decontrolled.
Veterinary use
In veterinary anesthesia, butorphanol (trade name: Torbugesic) is widely used as a sedative and analgesic in dogs, cats and horses. For sedation, it may be combined with tranquilizers such as alpha-2 agonists (medetomidine), benzodiazepines, or acepromazine in dogs, cats and exotic animals. It is frequently combined with xylazine or detomidine in horses.[12]
Butorphanol is used for sedation and mild to moderate pain control in dogs and cats. It is not considered adequate pain control in dogs undergoing surgical pain. It is used for operative and accident-related pain in small mammals such as dogs, cats, ferrets, coatis, raccoons, mongooses, various marsupials, some rodents and perhaps some larger birds.
Although butorphanol is commonly used for pain relief in reptiles, no studies (as of 2014) have conclusively shown that it is an effective analgesic in reptiles.[13]
Use in horses
Butorphanol is a narcotic used for pain relief in horses.[14] It is administered either IM or IV, with its analgesic properties beginning to take effect about 15 minutes after injection and lasting 4 hours.[15] It is also commonly paired with sedatives, such as xylazine and detomidine, to make the horse easier to handle during veterinary procedures.
Side effects specific to horses include sedation and CNS excitement (displayed by head pressing or tossing). Overdosing may result in seizures, falling, salivation, constipation, and muscle twitching. If an overdose occurs, a narcotic antagonist, such as naloxone, may be given. Caution should be used if butorphanol is administered in addition to other narcotics, sedatives, depressants, or antihistamines as it will cause an additive effect.
Butorphanol can cross the placenta and it will be present in the milk of lactating mares who are given the drug.
The drug is also prohibited for use in competition by most equestrian organizations, including the FEI, which considers it a class A drug.
See also
Notes
- ^ Anvisa (2023-03-31). "RDC Nº 784 - Listas de Substâncias Entorpecentes, Psicotrópicas, Precursoras e Outras sob Controle Especial" [Collegiate Board Resolution No. 784 - Lists of Narcotic, Psychotropic, Precursor, and Other Substances under Special Control] (in Brazilian Portuguese). Diário Oficial da União (published 2023-04-04). Archived from the original on 2023-08-03. Retrieved 2023-08-16.
- ^ US 3819635, "14-hydroxymorphinan derivatives."
- ^ US 3775414, "Process for the preparation of 14-hydroxymorphinan derivatives."
- ^ ISBN 978-1-4757-2085-3.
- ^ ISBN 978-3-88763-075-1.
- ^ ISBN 978-94-011-4439-1.
- ISBN 978-3-527-60749-5.
- ^ S2CID 31025735.
- PMID 16433932.
- ^ "Critical Review of Butorphanol" (PDF). 34th ECDD 2006/4.1. World Health Organization.
- ^ "Conversion Factors for Controlled Substances". DEA Diversion Control Division. United States Drug Enforcement Administration. Archived from the original on 2016-03-02. Retrieved 2014-06-19.
- ISBN 978-0-9548037-0-4.
- ISBN 978-0-323-24293-6.
- S2CID 249353700.
- PMID 6711944.
References
- Katzung BG (2001). Basic & Clinical Pharmacology (8th ed.). New York: McGraw-Hill. ISBN 978-0-8385-0598-4.
- Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM, DiPiro JT (2005). Pharmacotherapy: A Pathophysiologic Approach (6th ed.). New York: McGraw-Hill. ISBN 0-07-141613-7.
- Forney BC (2007). Equine Medications (Revised ed.). Lexington, Kentucky: Blood Horse Publications.
- The Merck Manual of Veterinary Medicine. 2004.
