CYP2D6
Ensembl |
|
| |||||||
|---|---|---|---|---|---|---|---|---|---|
| UniProt |
| ||||||||
| RefSeq (mRNA) |
| ||||||||
| RefSeq (protein) |
| ||||||||
| Location (UCSC) | Chr 22: 42.13 – 42.13 Mb | n/a | |||||||
| PubMed search | [2] | n/a | |||||||
| View/Edit Human | |||
Cytochrome P450 2D6 (CYP2D6) is an enzyme that in humans is encoded by the CYP2D6 gene. CYP2D6 is primarily expressed in the liver. It is also highly expressed in areas of the central nervous system, including the substantia nigra.
CYP2D6, a member of the
Considerable variation exists in the efficiency and amount of CYP2D6 enzyme produced between individuals. Hence, for drugs that are metabolized by CYP2D6 (that is, are CYP2D6
Gene
The gene is located on
Genotype/phenotype variability
CYP2D6 shows the largest phenotypical variability among the CYPs, largely due to genetic polymorphism. The genotype accounts for normal, reduced, and non-existent CYP2D6 function in subjects. Pharmacogenomic tests are now available to identify patients with variations in the CYP2D6 allele and have been shown to have widespread use in clinical practice.[17] The CYP2D6 function in any particular subject may be described as one of the following:[18]
- poor metabolizer – little or no CYP2D6 function
- intermediate metabolizers – metabolize drugs at a rate somewhere between the poor and extensive metabolizers
- extensive metabolizer – normal CYP2D6 function
- ultrarapid metabolizer – multiple copies of the CYP2D6 gene are expressed, so greater-than-normal CYP2D6 function occurs
A patient's CYP2D6 phenotype is often clinically determined via the administration of debrisoquine (a selective CYP2D6 substrate) and subsequent plasma concentration assay of the debrisoquine metabolite (4-hydroxydebrisoquine).[19]
The type of CYP2D6 function of an individual may influence the person's response to different doses of drugs that CYP2D6 metabolizes. The nature of the effect on the drug response depends not only on the type of CYP2D6 function, but also on the extent to which processing of the drug by CYP2D6 results in a chemical that has an effect that is similar, stronger, or weaker than the original drug, or no effect at all. For example, if CYP2D6 converts a drug that has a strong effect into a substance that has a weaker effect, then poor metabolizers (weak CYP2D6 function) will have an exaggerated response to the drug and stronger side-effects; conversely, if CYP2D6 converts a different drug into a substance that has a greater effect than its parent chemical, then ultrarapid metabolizers (strong CYP2D6 function) will have an exaggerated response to the drug and stronger side-effects.[20] Information about how human genetic variation of CYP2D6 affects response to medications can be found in databases such PharmGKB,[21] Clinical Pharmacogenetics Implementation Consortium (CPIC).[22]
Genetic basis of variability
The variability in metabolism is due to multiple different polymorphisms of the CYP2D6 allele, located on chromosome 22. Subjects possessing certain allelic variants will show normal, decreased, or no CYP2D6 function, depending on the allele. Pharmacogenomic tests are now available to identify patients with variations in the CYP2D6 allele and have been shown to have widespread use in clinical practice.[17] The current known alleles of CYP2D6 and their clinical function can be found in databases such as PharmVar.[23]
| CYP2D6 enzyme activity for selected alleles[24][25] | |
| Allele | CYP2D6 activity |
| CYP2D6*1 | normal |
| CYP2D6*2 | normal |
| CYP2D6*3 | none |
| CYP2D6*4 | none |
| CYP2D6*5 | none |
| CYP2D6*6 | none |
| CYP2D6*7 | none |
| CYP2D6*8 | none |
| CYP2D6*9 | decreased |
| CYP2D6*10 | decreased |
| CYP2D6*11 | none |
| CYP2D6*12 | none |
| CYP2D6*13 | none |
| CYP2D6*14 | none |
| CYP2D6*15 | none |
| CYP2D6*17 | decreased |
| CYP2D6*19 | none |
| CYP2D6*20 | none |
| CYP2D6*21 | none |
| CYP2D6*27 | normal |
| CYP2D6*29 | decreased |
| CYP2D6*31 | none |
| CYP2D6*33 | normal |
| CYP2D6*38 | none |
| CYP2D6*40 | none |
| CYP2D6*41 | decreased |
| CYP2D6*42 | none |
| CYP2D6*44 | none |
| CYP2D6*47 | none |
| CYP2D6*50 | decreased |
| CYP2D6*51 | none |
| CYP2D6*68 | none |
| CYP2D6*92 | none |
| CYP2D6*100 | none |
| CYP2D6*101 | none |
| CYP2D6 duplication | increased |
Ethnic factors in variability
Ethnicity is a factor in the occurrence of CYP2D6 variability. The reduction of the liver cytochrome CYP2D6 enzyme occurs approximately in 7–10% in
Caucasians with European descent predominantly (around 71%) have the functional group of CYP2D6 alleles, producing extensive metabolism, while functional alleles represent only around 50% of the allele frequency in populations of Asian descent.[29]
This variability is accounted for by the differences in the prevalence of various CYP2D6 alleles among the populations–approximately 10% of whites are intermediate metabolizers, due to decreased CYP2D6 function, because they appear to have the one (
Ligands
Following is a table of selected
Inhibitors of CYP2D6 can be classified by their potency, such as:
- Strong inhibitor being one that causes at least a 5-fold increase in the plasma clearance thereof.[30]
- Moderate inhibitor being one that causes at least a 2-fold increase in the plasma AUC values of sensitive substrates metabolized through CYP2D6, or 50-80% decrease in clearance thereof.[30]
- Weak inhibitor being one that causes at least a 1.25-fold but less than 2-fold increase in the plasma AUC values of sensitive substrates metabolized through CYP2D6, or 20-50% decrease in clearance thereof.[30]
| Substrates ↑ = bioactivation by CYP2D6 |
Inhibitors | Inducers |
|---|---|---|
|
Strong
Moderate
Weak
Unspecified potency
|
Strong Unspecified potency |
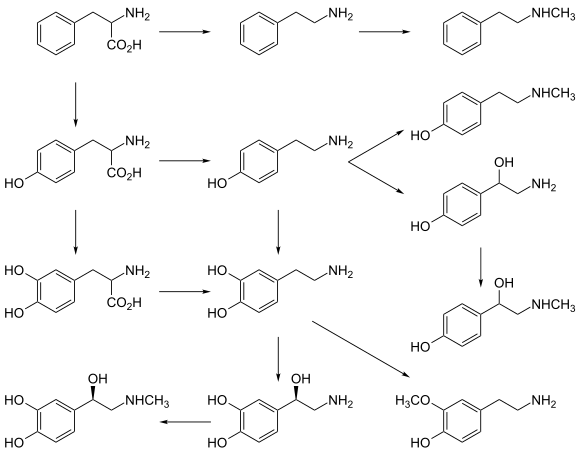
Dopamine biosynthesis
m-tyramine into dopamine.[36] |
References
- ^ a b c ENSG00000275211, ENSG00000280905, ENSG00000282966, ENSG00000283284, ENSG00000272532 GRCh38: Ensembl release 89: ENSG00000100197, ENSG00000275211, ENSG00000280905, ENSG00000282966, ENSG00000283284, ENSG00000272532 - Ensembl, May 2017
- ^ "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- ^ S2CID 41857580.
- PMID 24374199.
- ^ PMID 22185816.
- PMID 22515611.
- PMID 28520365.
- PMID 28520350.
- S2CID 218535295.
- PMID 22694279.
- (PDF) from the original on 2 February 2024. Retrieved 2 February 2024.
- S2CID 5326129.
- PMID 34046497.
- PMID 18781911.
- PMID 21670550.
- ^ "Entrez Gene: CYP2D6 cytochrome P450, family 2, subfamily D, polypeptide 6". Archived from the original on 8 March 2010. Retrieved 3 November 2017.
- ^ S2CID 206399446.
- PMID 11851634.
- PMID 19102711.
- PMID 17708140.
- ^ "PharmGKB". PharmGKB. Archived from the original on 3 October 2022. Retrieved 3 October 2022.
- ^ "CYP2D6 CPIC guidelines". cpicpgx.org. Archived from the original on 3 October 2022. Retrieved 3 October 2022.
- ^ "PharmVar". www.pharmvar.org. Archived from the original on 19 May 2020. Retrieved 15 February 2024.
- ^ PMID 9731719.
- ^ "PharmVar". Archived from the original on 19 May 2020. Retrieved 20 May 2020.
- ISBN 9780779699711.
- PMID 9241658.
- PMID 19512959.
- PMID 11972444.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah ai aj ak al am an ao ap aq ar as at au av aw ax ay az ba bb bc bd be bf bg bh bi bj bk bl bm bn bo bp bq br bs bt bu bv bw bx by bz ca cb cc cd ce cf "Drug Interactions: Cytochrome P450 Drug Interaction Table". Indiana University School of Medicine. 2007. Archived from the original on 10 October 2007. Retrieved 25 July 2010. Retrieved in July 2011
- ^ FASS (drug formulary): Swedish environmental classification of pharmaceuticals Archived 11 June 2002 at the Wayback MachineFacts for prescribers (Fakta för förskrivare), retrieved July 2011
- ^ PMID 11411304.
- ^ "Hydrocodone". Drugbank. Archived from the original on 6 September 2011. Retrieved 14 June 2011.
- S2CID 19501089.
- ^ "Wakix pitolisant tablets Prescribing Information" (PDF). Wakix HCP. Archived (PDF) from the original on 11 January 2023. Retrieved 11 January 2023.
- ^ PMID 24374199.
- PMID 34035391.
- PMID 20942780.
- ^ a b "DILTIAZEM HCL CD- diltiazem hydrochloride capsule, coated, extended release". DailyMed. 1 February 2017. Archived from the original on 31 January 2019. Retrieved 31 January 2019.
- ^ "NIFEDIPINE EXTENDED RELEASE- nifedipine tablet, extended release". DailyMed. 29 November 2012. Archived from the original on 31 January 2022. Retrieved 1 February 2019.
- S2CID 24591644.
- PMID 27618912.
- ^ "Medical Cannabis Adverse Effects & Drug Interactions" (PDF). Archived (PDF) from the original on 14 December 2019. Retrieved 28 October 2019.
- S2CID 24002845.
- PMID 22855269.
- S2CID 206489481.
- PMID 12756210.
- ^ a b "Citalopram Oral Solution". Drugs.com. Archived from the original on 8 February 2018. Retrieved 23 January 2018.
- ^ "Escitalopram-drug-information". UpToDate. Archived from the original on 28 October 2020. Retrieved 22 May 2019.
- ^ a b "Drug Development and Drug Interactions: Table of Substrates, Inhibitors and Inducers". FDA. 26 May 2021. Archived from the original on 4 November 2020. Retrieved 21 June 2020.
- ^ Nevels RM, Weiss NH, Killebrew AE, Gontkovsky ST (July 2013). "Methylphenidate and Its Under-recognized, Under- explained, and Serious Drug Interactions: A Review of the Literature with Heightened Concerns" (PDF). German Journal of Psychiatry: 29–42. Archived from the original (PDF) on 9 April 2018. Retrieved 31 August 2016.
- S2CID 1246705.
- PMID 9153299.
- PMID 2061924.
- S2CID 34832618. Archived from the originalon 1 November 2019. Retrieved 1 November 2019.
- ^ Last reviewed 8 April 2008
- S2CID 601644.
- S2CID 2366709.
- PMID 15081432.
- PMID 30558213.
- S2CID 71360020.
- PMID 19948186.
- PMID 15860375.
Further reading
- Smith G, Stubbins MJ, Harries LW, Wolf CR (December 1998). "Molecular genetics of the human cytochrome P450 monooxygenase superfamily". Xenobiotica; the Fate of Foreign Compounds in Biological Systems. 28 (12): 1129–65. PMID 9890157.
- Wolf CR, Smith G (1999). "Cytochrome P450 CYP2D6". IARC Scientific Publications (148): 209–29. PMID 10493260.
- Ding X, Kaminsky LS (2003). "Human extrahepatic cytochromes P450: function in xenobiotic metabolism and tissue-selective chemical toxicity in the respiratory and gastrointestinal tracts". Annual Review of Pharmacology and Toxicology. 43: 149–73. PMID 12171978.
- Lilienfeld S (2006). "Galantamine--a novel cholinergic drug with a unique dual mode of action for the treatment of patients with Alzheimer's disease". CNS Drug Reviews. 8 (2): 159–76. PMID 12177686.
- Yu AM, Idle JR, Gonzalez FJ (May 2004). "Polymorphic cytochrome P450 2D6: humanized mouse model and endogenous substrates". Drug Metabolism Reviews. 36 (2): 243–77. from the original on 29 June 2022. Retrieved 5 July 2019.
- Abraham JE, Maranian MJ, Driver KE, Platte R, Kalmyrzaev B, Baynes C, et al. (2010). "CYP2D6 gene variants: association with breast cancer specific survival in a cohort of breast cancer patients from the United Kingdom treated with adjuvant tamoxifen". Breast Cancer Research. 12 (4): R64. PMID 20731819.
- Abraham JE, Maranian MJ, Driver KE, Platte R, Kalmyrzaev B, Baynes C, et al. (June 2011). "CYP2D6 gene variants and their association with breast cancer susceptibility". Cancer Epidemiology, Biomarkers & Prevention. 20 (6): 1255–8. S2CID 32846974.
External links
- Flockhart Lab Cyp2D6 Substrates Page at IUPUI
- PharmGKB: Annotated PGx Gene Information for CYP2D6
- Human CYP2D6 genome location and CYP2D6 gene details page in the UCSC Genome Browser.
- Overview of all the structural information available in the PDB for UniProt: P10635 (Cytochrome P450 2D6) at the PDBe-KB.