Candida tropicalis
| Candida tropicalis | |
|---|---|
| |
| Scientific classification | |
| Domain: | Eukaryota |
| Kingdom: | Fungi |
| Division: | Ascomycota |
| Class: | Saccharomycetes |
| Order: | Saccharomycetales |
| Family: | Saccharomycetaceae |
| Genus: | Candida |
| Species: | C. tropicalis
|
| Binomial name | |
| Candida tropicalis (Castellani) Berkhout (1923)
| |
| Synonyms | |
| |
Candida tropicalis is a species of
History and taxonomy
In the history of fungi, the name of genus Candida, derived from the family
In the genus Candida, there are other species that are similar to Candida tropicalis. Candida albicans is taxonomically close to C. tropicalis sharing many pathogenic traits[5] whereas C. maltosa and C. sake are physiologically similar to C. tropicalis but they can be differentiated by the growth at 35 °C (only C. sake showing negative) and assimilation of soluble starch (only C. tropicalis showing positive starch assimilation).[6]
Identification
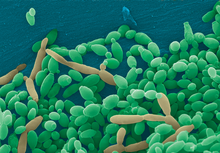
C. tropicalis is easily identified using phenotypic and molecular methods.[7] The identification of species in the genus Candida relies on morphological and physiological features. Species in the genus are vegetative cells which reproduce asexually by budding, and the structure, shape, septation, color and arrangement of buds is useful for identification.[8] The production and appearance of pseudohyphae and blastoconidia may also be useful for identification.[8] Physiological profiles relating to carbon and nitrogen utilization are of value in determining species, as are the presence certain distinctive biochemical features.[6] Increasingly, molecular genetic methods such as DNA sequencing are used as primary tools for the accurate determination of species identifications in this group.[6]
Growth and morphology
There are different media on which C. tropicalis can grow effectively. A common medium used is the Sabouraud’s agar which contains peptone and sugar. This is enough for identifying the species but with a disadvantage of promoting mycelial growth and suppressing conidia formation.[8] Another commonly used medium is the cornmeal agar which is useful in inducing formation of conidia.[8] Potato-glucose, potato-carrot, tomato juice, lima bean and others are also types of media used for growth.[8] The optimal temperature for growth is between 25–35 °C (77–95 °F)[4] and growth is enhanced if sugar or fat is added in the medium. Colonies of C. tropicalis are white, smooth and butyrous with a fringed border.[6][9]
Physiology
C. tropicalis reproduces asexually by the production of blastoconidia through
Physiological characteristics of C. tropicalis
Growth
- Positive for
- Positive temperatures from 25–40 °C (77–104 °F).[6]
Fermentation
- positive for F1 D-glucose, F2 D-glucose, F3 Maltose[6][10][7]
- positive delay after 7 days for F6 α,α-trehalose.[6][7]
- negative for F7 Melibiose, F8 Lactose, F9 Cellobiose, F11 Raffinose, F12 Inulin, F14 D-xylose.[6]
- negative delay after 7 days for F4 Me-α-D-glucoside, F10 Melezitose.[6]
- positive and negative for F5 Sucrose and F13 Starch.[6][10]
Urea hydrolysis
This test is to detect yeast’s ability to produce enzyme urease. Once there's a compatible substrate, urease will split urea to produce ammonia increasing the pH. C. tropicalis is found to be urease negative.[3]
Diazonium Blue B Test
This test uses the azo dye, diazonium blue B which differentially stains cells from species affiliated with the Division, Basidiomycota. For C. tropicalis, this test is negative.[6]
Parasexuality
C. tropicalis diploid cells of opposite mating type can mate to form tetraploid cells.[11] These cells may then undergo chromosome loss during long-term propagation in rich medium resulting in the eventual regeneration of diploid cells.[12] Such diploid cells are again mating competent thus completing a parasexual cycle. Opaque C. tropicalis cells can also form an architecturally complex sexual biofilm.[13]
Habitat and ecology
Candida species are very pervasive yeasts that are distributed worldwide geographically. They are more likely to be found in tropical climate where temperature and humidity will enhance the adaptability of C. tropicalis.
Storage and transportation
The selection of medium for sample growth is very important accounting for the pros and cons of each type of growth medium. Once decided on the medium, need to add 8 ug of fluconazole per mL to limit bacterial growth and contamination.[3] When the medium is ready, it is optional to add supplement to help and optimize specimen growth. After the growth, features examination including shape, size, bud arrangement, cell wall thickness, temperature of growth, pseudohyphae presence, arthroconidia presence, and capsule presence are all important to take into account.[3] If the species are grown using any type of the medium mentioned, the transportation of specimens for testing should be completed in less than two hours.[3] If there is any delay, the samples should be stored at 37 °C with the exception of contaminated specimens that need be stored in 4 °C.[3]
Pathogenicity
In tropical countries, C. tropicalis is one of the most common colonizer and pathogen causing human disease,[5] especially found on human skin, in the gastrointestinal tract and also in female genitourinary tract.[4] It can be transmitted between health-care workers and patients,[5] especially in environments such as hospitals.[5] C. tropicalis can survive for up to 24 hours therefore be cross-transmitted to a second hand with a probability of 69% and to a third hand with 38% probability.[5] It is the cause responsible for approximately half of the beyond-surface candida infections.[5] C. tropicalis is the second most virulent Candida species[7] that can significantly affect by spreading through the weakened immune system host and can occupy the gastrointestinal tract within 30 minutes of inoculation, all this resulting in increased mortality.[5][14][10] Impact of candidiasis, infections cause by C. tropicalis, have increased globally.[14] C. tropicalis is virulent due to its ability to produce biofilm, secrete lytic enzymes, adhere to epithelial and endothelial cells, and undergo transition of bud to hyphae.[15][10][7]
Biofilms are complex structures that are formed from the grouping of microorganisms on a local surface, either biotic or abiotic,[15] dependent on the ability of cellular adhesion to substrates.[7]
For C. tropicalis to fully enter and cause infection in the host, it needs some helpers. First, once it is attached onto the host tissues, extracellular enzymes called the proteases will be produced to facilitate the penetration of the pathogen and allow it to interfere with the host defense system.
Human diseases

Types of disease caused by C. tropicalis will vary depending on the location where the species colonizes. With an infection in the mucous membrane, subject will experience
If an infection involves interdigital candidiasis, paronychia and diaper rash, subject is likely to have cutaneous candidiasis.[14] Otherwise, if an infection involves body fluid and internal organs damages, subject will experience pulmonary candidiasis, invasive and disseminated candidiasis, gastrointestinal candidiasis and candidemia.[14] C. tropicalis colonization is favoured in the gastrointestinal tract;[14] a common risk factor for individuals that are susceptible for invasive candidiasis development.[5] Candidemia is a worldwide bloodstream disease mainly affecting peripheral organs in humans.[5] Usually, candidemia caused by C. tropicalis are associated with cancer patients that have either leukemia or neutropenia.[15] According to the data obtained from 2010, frequency of candidemia is 12-25% in the US, 4.5-9% in Europe, 20-24% in Brazil and 20-60% in South Asia.[5] C. tropicalis can cause nosocomial fungal bloodstream infections along with C. glabrata and C. parapsilosis.[5] Mortality rate of invasive and disseminated infections caused by C. tropicalis is high, ranging from 40% to 70%.[5] Risk factors that contribute to the high rate are leukemia, anti-neoplastic chemotherapy, previous neutropenia, central venous catheters, long stay on intensive care and total parenteral nutrition.[5] Although children infections are not as common seen as in adults, leukemia, secondary neutropenia and bone marrow transplantation[14] are factors favouring C. tropicalis infections.[5] Another infection seen commonly in patients who have leukemia and secondary neutropenia, is chronic disseminated candidiasis (CDC) is another type of disseminated candida infection that mainly develops in the liver, spleen and kidney.[5]
Treatment and prevention
The most important and most essential step to prevent contact with the fungi species is by washing the hands.
References
- PMID 23912864.
- S2CID 36366177.
- ^ ISBN 978-1555812553.
- ^ ISBN 9780323241472.
- ^ S2CID 36366177.
- ^ ISBN 978-0444813121.
- ^ PMID 29081766.
- ^ ISBN 978-0721624440.
- ^ ISBN 978-0521350563.
- ^ PMID 21569057.
- ^ Porman AM, Alby K, Hirakawa MP, Bennett RJ. Discovery of a phenotypic switch regulating sexual mating in the opportunistic fungal pathogen Candida tropicalis. Proceedings of the National Academy of Sciences USA 2011 Dec 27;108(52):21158-63. doi: 10.1073/pnas.1112076109.
- ^ Seervai RN, Jones SK Jr, Hirakawa MP, Porman AM, Bennett RJ. Parasexuality and ploidy change in Candida tropicalis. Eukaryot Cell. 2013 Dec;12(12):1629-40. doi: 10.1128/EC.00128-13. PMID 24123269
- ^ Jones SK Jr, Hirakawa MP, Bennett RJ. Sexual biofilm formation in Candida tropicalis opaque cells. Mol Microbiol. 2014 Apr;92(2):383-98. doi: 10.1111/mmi.12565. PMID 24612417
- ^ PMID 20413622.
- ^ PMID 23180477.
