Carcinogenesis
Carcinogenesis, also called oncogenesis or tumorigenesis, is the formation of a
Variants of inherited genes may predispose individuals to cancer. In addition, environmental factors such as
Causes
Genetic and epigenetic
There is a diverse classification scheme for the various genomic changes that may contribute to the generation of
DNA damage
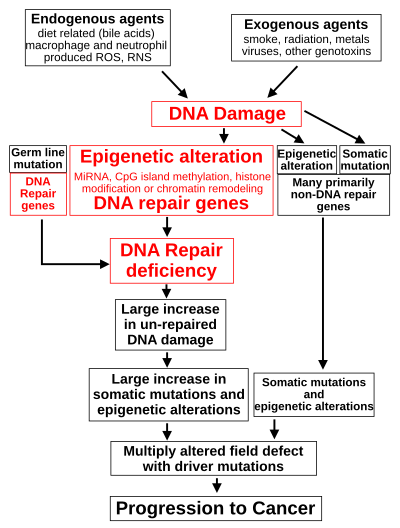
DNA damage is considered to be the primary cause of cancer.[17] More than 60,000 new naturally-occurring instances of DNA damage arise, on average, per human cell, per day, due to endogenous cellular processes (see article DNA damage (naturally occurring)).
Additional DNA damage can arise from exposure to
DNA damage can also be caused by
Such exogenous and endogenous sources of DNA damage are indicated in the boxes at the top of the figure in this section. The central role of DNA damage in progression to cancer is indicated at the second level of the figure. The central elements of DNA damage, epigenetic alterations and deficient DNA repair in progression to cancer are shown in red.
A deficiency in DNA repair would cause more DNA damage to accumulate, and increase the risk for cancer. For example, individuals with an inherited impairment in any of 34
The majority of cancers are called non-hereditary or "sporadic cancers". About 30% of sporadic cancers do have some hereditary component that is currently undefined, while the majority, or 70% of sporadic cancers, have no hereditary component.[26]
In sporadic cancers, a deficiency in DNA repair is occasionally due to a mutation in a DNA repair gene; much more frequently, reduced or absent expression of DNA repair genes is due to
When expression of DNA repair genes is reduced, this causes a DNA repair deficiency. This is shown in the figure at the 4th level from the top. With a DNA repair deficiency, DNA damage persists in cells at a higher than typical level (5th level from the top in figure); this excess damage causes an increased frequency of mutation and/or
The somatic mutations and epigenetic alterations caused by DNA damage and deficiencies in DNA repair accumulate in field defects. Field defects are normal-appearing tissues with multiple alterations (discussed in the section below), and are common precursors to development of the disordered and over-proliferating clone of tissue in a cancer. Such field defects (second level from bottom of figure) may have numerous mutations and epigenetic alterations.
It is impossible to determine the initial cause for most specific cancers. In a few cases, only one cause exists: for example, the virus
Using molecular biological techniques, it is possible to characterize the mutations, epimutations or chromosomal aberrations within a tumor, and rapid progress is being made in the field of predicting certain cancer patients' prognosis based on the spectrum of mutations. For example, up to half of all tumors have a defective p53 gene. This mutation is associated with poor prognosis, since those tumor cells are less likely to go into apoptosis or programmed cell death when damaged by therapy. Telomerase mutations remove additional barriers, extending the number of times a cell can divide. Other mutations enable the tumor to grow new blood vessels to provide more nutrients, or to metastasize, spreading to other parts of the body. However, once a cancer is formed it continues to evolve and to produce sub-clones. It was reported in 2012 that a single renal cancer specimen, sampled in nine different areas, had 40 "ubiquitous" mutations, found in all nine areas, 59 mutations shared by some, but not all nine areas, and 29 "private" mutations only present in one area.[35]
The lineages of cells in which all these DNA alterations accumulate are difficult to trace, but two recent lines of evidence suggest that normal
Second, statistics show that most human cancers are diagnosed in older people. A possible explanation is that cancers occur because cells accumulate damage through time. DNA is the only cellular component that can accumulate damage over the entire course of a life, and stem cells are the only cells that can transmit DNA from the zygote to cells late in life. Other cells, derived from stem cells, do not keep DNA from the beginning of life until a possible cancer occurs. This implies that most cancers arise from normal stem cells.[36][37]
Contribution of field defects

The term "field cancerization" was first used in 1953 to describe an area or "field" of epithelium that has been preconditioned by (at that time) largely unknown processes so as to predispose it towards development of cancer.[39] Since then, the terms "field cancerization" and "field defect" have been used to describe pre-malignant tissue in which new cancers are likely to arise.[citation needed]
Field defects have been identified in association with cancers and are important in progression to cancer.
In the colon, a field defect probably arises by natural selection of a mutant or epigenetically altered cell among the stem cells at the base of one of the
If the general process by which sporadic colon cancers arise is the formation of a pre-neoplastic clone that spreads by natural selection, followed by formation of internal sub-clones within the initial clone, and sub-sub-clones inside those, then colon cancers generally should be associated with, and be preceded by, fields of increasing abnormality, reflecting the succession of premalignant events. The most extensive region of abnormality (the outermost yellow irregular area in the diagram) would reflect the earliest event in formation of a malignant neoplasm.
In experimental evaluation of specific DNA repair deficiencies in cancers, many specific DNA repair deficiencies were also shown to occur in the field defects surrounding those cancers. The table below gives examples for which the DNA repair deficiency in a cancer was shown to be caused by an epigenetic alteration, and the somewhat lower frequencies with which the same epigenetically caused DNA repair deficiency was found in the surrounding field defect.
| Cancer | Gene | Frequency in Cancer | Frequency in Field Defect | Reference |
|---|---|---|---|---|
| Colorectal | MGMT | 46% | 34% | [45] |
| Colorectal | MGMT | 47% | 11% | [46] |
| Colorectal | MGMT | 70% | 60% | [47] |
| Colorectal | MSH2 | 13% | 5% | [46] |
| Colorectal | ERCC1 | 100% | 40% | [48] |
| Colorectal | PMS2 | 88% | 50% | [48] |
| Colorectal | XPF | 55% | 40% | [48] |
| Head and Neck | MGMT | 54% | 38% | [49] |
| Head and Neck | MLH1 | 33% | 25% | [50] |
| Head and Neck | MLH1 | 31% | 20% | [51] |
| Stomach | MGMT | 88% | 78% | [52] |
| Stomach | MLH1 | 73% | 20% | [53] |
| Esophagus | MLH1 | 77%–100% | 23%–79% | [54] |
Some of the small polyps in the field defect shown in the photo of the opened colon segment may be relatively benign neoplasms. In a 1996 study of polyps less than 10mm in size found during colonoscopy and followed with repeat colonoscopies for 3 years, 25% remained unchanged in size, 35% regressed or shrank in size and 40% grew in size.[55]
Genome instability
Cancers are known to exhibit
Non-mainstream theories
There are a number of theories of carcinogenesis and cancer treatment that fall outside the mainstream of scientific opinion, due to lack of scientific rationale, logic, or evidence base. These theories may be used to justify various alternative cancer treatments. They should be distinguished from those theories of carcinogenesis that have a logical basis within mainstream cancer biology, and from which conventionally testable hypotheses can be made.[citation needed]
Several alternative theories of carcinogenesis, however, are based on scientific evidence and are increasingly being acknowledged. Some researchers believe that cancer may be caused by
A number of authors have questioned the assumption that cancers result from sequential random mutations as oversimplistic, suggesting instead that cancer results from a failure of the body to inhibit an innate, programmed proliferative tendency.[63] A related theory suggests that cancer is an atavism, an evolutionary throwback to an earlier form of multicellular life.[64] The genes responsible for uncontrolled cell growth and cooperation between cancer cells are very similar to those that enabled the first multicellular life forms to group together and flourish. These genes still exist within the genomes of more complex metazoans, such as humans, although more recently evolved genes keep them in check. When the newer controlling genes fail for whatever reason, the cell can revert to its more primitive programming and reproduce out of control. The theory is an alternative to the notion that cancers begin with rogue cells that undergo evolution within the body. Instead, they possess a fixed number of primitive genes that are progressively activated, giving them finite variability.[65] Another evolutionary theory puts the roots of cancer back to the origin of the eukaryote (nucleated) cell by massive horizontal gene transfer, when the genomes of infecting viruses were cleaved (and thereby attenuated) by the host, but their fragments integrated into the host genome as immune protection. Cancer thus originates when a rare somatic mutation recombines such fragments into a functional driver of cell proliferation.[66]
Cancer cell biology
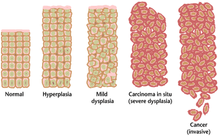
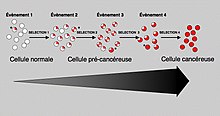
Often, the multiple genetic changes that result in cancer may take many years to accumulate. During this time, the biological behavior of the pre-malignant cells slowly changes from the properties of normal cells to cancer-like properties. Pre-malignant tissue can have a
The most severe cases of dysplasia are referred to as carcinoma in situ. In Latin, the term in situ means "in place"; carcinoma in situ refers to an uncontrolled growth of dysplastic cells that remains in its original location and has not shown invasion into other tissues. Carcinoma in situ may develop into an invasive malignancy and is usually removed surgically when detected.
Clonal evolution
Just as a population of animals undergoes evolution, an unchecked population of cells also can undergo "evolution". This undesirable process is called somatic evolution, and is how cancer arises and becomes more malignant over time.[67]
Most changes in cellular metabolism that allow cells to grow in a disorderly fashion lead to cell death. However, once cancer begins,
Biological properties of cancer cells
In a 2000 article by Hanahan and Weinberg, the biological properties of malignant tumor cells were summarized as follows:[69]
- Acquisition of self-sufficiency in growth signals, leading to unchecked growth.
- Loss of sensitivity to anti-growth signals, also leading to unchecked growth.
- Loss of capacity for apoptosis, allowing growth despite genetic errors and external anti-growth signals.
- Loss of capacity for senescence, leading to limitless replicative potential (immortality)
- Acquisition of sustained angiogenesis, allowing the tumor to grow beyond the limitations of passive nutrient diffusion.
- Acquisition of ability to invade neighbouring tissues, the defining property of invasive carcinoma.
- Acquisition of ability to seed metastases at distant sites, a late-appearing property of some malignant tumors (carcinomas or others).
The completion of these multiple steps would be a very rare event without:
- Loss of capacity to repair genetic errors, leading to an increased mutation rate (genomic instability), thus accelerating all the other changes.
These biological changes are classical in
Cancer as a defect in cell interactions
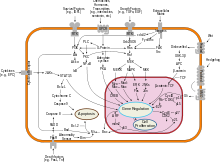
Normally, once a tissue is injured or infected, damaged cells elicit inflammation by stimulating specific patterns of enzyme activity and cytokine gene expression in surrounding cells.[71][72] Discrete clusters ("cytokine clusters") of molecules are secreted, which act as mediators, inducing the activity of subsequent cascades of biochemical changes.[73] Each cytokine binds to specific receptors on various cell types, and each cell type responds in turn by altering the activity of intracellular signal transduction pathways, depending on the receptors that the cell expresses and the signaling molecules present inside the cell.[74][75] Collectively, this reprogramming process induces a stepwise change in cell phenotypes, which will ultimately lead to restoration of tissue function and toward regaining essential structural integrity.[76][77] A tissue can thereby heal, depending on the productive communication between the cells present at the site of damage and the immune system.[78] One key factor in healing is the regulation of cytokine gene expression, which enables complementary groups of cells to respond to inflammatory mediators in a manner that gradually produces essential changes in tissue physiology.[79][80][81] Cancer cells have either permanent (genetic) or reversible (epigenetic) changes to their genome, which partly inhibit their communication with surrounding cells and with the immune system.[82][83] Cancer cells do not communicate with their tissue microenvironment in a manner that protects tissue integrity; instead, the movement and the survival of cancer cells become possible in locations where they can impair tissue function.[84][85] Cancer cells survive by "rewiring" signal pathways that normally protect the tissue from the immune system. This alteration of the immune response is evident in early stages of malignancy too.[86][87]
One example of tissue function rewiring in cancer is the activity of transcription factor NF-κB.[88] NF-κB activates the expression of numerous genes involved in the transition between inflammation and regeneration, which encode cytokines, adhesion factors, and other molecules that can change cell fate.[89] This reprogramming of cellular phenotypes normally allows the development of a fully functional intact tissue.[90] NF-κB activity is tightly controlled by multiple proteins, which collectively ensure that only discrete clusters of genes are induced by NF-κB in a given cell and at a given time.[91] This tight regulation of signal exchange between cells protects the tissue from excessive inflammation, and ensures that different cell types gradually acquire complementary functions and specific positions. Failure of this mutual regulation between genetic reprogramming and cell interactions allows cancer cells to give rise to metastasis. Cancer cells respond aberrantly to cytokines, and activate signal cascades that can protect them from the immune system.[88][92]
In fish
The role of iodine in marine fish (rich in iodine) and freshwater fish (iodine-deficient) is not completely understood, but it has been reported that freshwater fish are more susceptible to infectious and, in particular, neoplastic and atherosclerotic diseases, than marine fish.[93][94] Marine elasmobranch fishes such as sharks, stingrays etc. are much less affected by cancer than freshwater fishes, and therefore have stimulated medical research to better understand carcinogenesis.[95]
Mechanisms
In order for cells to start dividing uncontrollably, genes that regulate cell growth must be dysregulated.
Oncogenes
Mutations in proto-oncogenes, which are the normally quiescent counterparts of
One of the first
Proto-oncogenes
Proto-oncogenes promote cell growth in a variety of ways. Many can produce
Mutations in proto-oncogenes can modify their expression and function, increasing the amount or activity of the product protein. When this happens, they become oncogenes, and, thus, cells have a higher chance of dividing excessively and uncontrollably. The chance of cancer cannot be reduced by removing proto-oncogenes from the genome, as they are critical for growth, repair and homeostasis of the body. It is only when they become mutated that the signals for growth become excessive. It is important to note that a gene possessing a growth-promoting role may increase the carcinogenic potential of a cell, under the condition that all necessary cellular mechanisms that permit growth are activated.[101] This condition also includes the inactivation of specific tumor suppressor genes (see below). If the condition is not fulfilled, the cell may cease to grow and can proceed to die. This makes identification of the stage and type of cancer cell that grows under the control of a given oncogene crucial for the development of treatment strategies.
Tumor suppressor genes
Despite nearly half of all cancers possibly involving alterations in p53, its tumor suppressor function is poorly understood. p53 clearly has two functions: one a nuclear role as a transcription factor, and the other a cytoplasmic role in regulating the cell cycle, cell division, and apoptosis.
The Warburg effect is the preferential use of glycolysis for energy to sustain cancer growth. p53 has been shown to regulate the shift from the respiratory to the glycolytic pathway.[102]
However, a mutation can damage the tumor suppressor gene itself, or the signal pathway that activates it, "switching it off". The invariable consequence of this is that DNA repair is hindered or inhibited: DNA damage accumulates without repair, inevitably leading to cancer.
Mutations of tumor suppressor genes that occur in
Development of cancer was proposed in 1971 to depend on at least two mutational events. In what became known as the
Usually, oncogenes are
Knudson's two hit model has recently been challenged by several investigators. Inactivation of one allele of some tumor suppressor genes is sufficient to cause tumors. This phenomenon is called haploinsufficiency and has been demonstrated by a number of experimental approaches. Tumors caused by haploinsufficiency usually have a later age of onset when compared with those by a two hit process.[104]
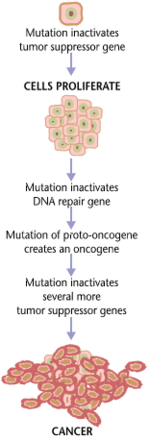
Multiple mutations
In general, mutations in both types of genes are required for cancer to occur. For example, a mutation limited to one oncogene would be suppressed by normal mitosis control and tumor suppressor genes, first
Mutation of tumor suppressor genes that are passed on to the next generation of not merely cells, but their
A new idea announced in 2011 is an extreme version of multiple mutations, called chromothripsis by its proponents. This idea, affecting only 2–3% of cases of cancer, although up to 25% of bone cancers, involves the catastrophic shattering of a chromosome into tens or hundreds of pieces and then being patched back together incorrectly. This shattering probably takes place when the chromosomes are compacted during normal cell division, but the trigger for the shattering is unknown. Under this model, cancer arises as the result of a single, isolated event, rather than the slow accumulation of multiple mutations. [105]
Non-mutagenic carcinogens
Many
Role of infections
Bacterial
Helicobacter pylori can cause gastric cancer. Although the data varies between different countries, overall about 1% to 3% of people infected with Helicobacter pylori develop gastric cancer in their lifetime compared to 0.13% of individuals who have had no H. pylori infection.[106][107] H. pylori infection is very prevalent. As evaluated in 2002, it is present in the gastric tissues of 74% of middle-aged adults in developing countries and 58% in developed countries.[108] Since 1% to 3% of infected individuals are likely to develop gastric cancer,[109] H. pylori-induced gastric cancer is the third highest cause of worldwide cancer mortality as of 2018.[110]
Infection by H. pylori causes no symptoms in about 80% of those infected.[111] About 75% of individuals infected with H. pylori develop gastritis.[112] Thus, the usual consequence of H. pylori infection is chronic asymptomatic gastritis.[113] Because of the usual lack of symptoms, when gastric cancer is finally diagnosed it is often fairly advanced. More than half of gastric cancer patients have lymph node metastasis when they are initially diagnosed.[114]
The gastritis caused by H. pylori is accompanied by
H. pylori also causes many epigenetic alterations linked to cancer development.[118][119] These epigenetic alterations are due to H. pylori-induced methylation of CpG sites in promoters of genes[118] and H. pylori-induced altered expression of multiple microRNAs.[119]
As reviewed by Santos and Ribeiro
Other bacteria might also play a role in carcinogenesis. Checkpoint control of the cell cycle and apoptosis by p53 is inhibited by the mycoplasma bacterium,[123] allowing cells with DNA damage to "run an apoptotic red light" and proceed through the cell cycle.
Viral
Furthermore, many cancers originate from a
Viruses that are known to cause cancer such as
Depending on their location, cells can be damaged through radiation, chemicals from cigarette smoke, and inflammation from bacterial infection or other viruses. Each cell has a chance of damage. Cells often die if they are damaged, through failure of a vital process or the immune system, however, sometimes damage will knock out a single cancer gene. In an old person, there are thousands, tens of thousands, or hundreds of thousands of knocked-out cells. The chance that any one would form a cancer is very low.[citation needed]
When the damage occurs in any area of changed cells, something different occurs. Each of the cells has the potential for growth. The changed cells will divide quicker when the area is damaged by physical, chemical, or viral agents. A vicious circle has been set up: Damaging the area will cause the changed cells to divide, causing a greater likelihood that they will experience knock-outs.
This model of carcinogenesis is popular because it explains why cancers grow. It would be expected that cells that are damaged through radiation would die or at least be worse off because they have fewer genes working; viruses increase the number of genes working.
One thought is that we may end up with thousands of vaccines to prevent every virus that can change our cells. Viruses can have different effects on different parts of the body. It may be possible to prevent a number of different cancers by immunizing against one viral agent. It is likely that HPV, for instance, has a role in cancers of the mucous membranes of the mouth.
Helminthiasis
Certain parasitic worms are known to be carcinogenic.[125] These include:
- Clonorchis sinensis (the organism causing Clonorchiasis) and Opisthorchis viverrini (causing Opisthorchiasis) are associated with cholangiocarcinoma.[126]
- Schistosoma species (the organisms causing Schistosomiasis) is associated with bladder cancer.
Epigenetics
Cancer stem cells
A new way of looking at carcinogenesis comes from integrating the ideas of
Clonal evolution
While genetic and
See also
- Cancer cell
- Armitage–Doll multistage model of carcinogenesis
- Linear no-threshold model
- Oncogenic retroviridae protein
References
- S2CID 247145082.
- S2CID 38445059.
- S2CID 1478778.
- PMID 12432047.
- ISSN 0036-8075.
- PMID 28336671.
- S2CID 7586573.
- ^ S2CID 20201610.
- S2CID 22975880.
- ^ PMID 28939880.
- PMID 34434669.
- PMID 35030162.
- PMID 18234754.
- S2CID 4430576.
- ^ PMID 20682795.
- ^ "How Chromosome Imbalances Can Drive Cancer | Harvard Medical School". hms.harvard.edu. 6 July 2023. Retrieved 2 April 2024.
- PMID 18403632.
- ^ PMID 21802474.
- PMID 22123420.
- PMID 21605492.
- PMID 12011430.
- PMID 21685942.
- PMID 21267546.
- PMID 21779515.
- PMID 9353177.
- PMID 10891514.
- PMID 15888787.
- ^ PMID 9096356.
- ^ PMID 16728433.
- ^ PMID 11850397.
- PMID 5770175.
- PMID 18704159.
- PMID 17616978.
- PMID 7895211.
- PMID 22397650.
- ^ PMID 26090957.
- ^ PMID 26097879.
- PMID 25554788.
- S2CID 6736946.
- PMID 18164807.
- PMID 20689513.
- S2CID 44981539.
- PMID 10655514.
- ^ PMID 23539594.
- PMID 16174854.
- ^ S2CID 8069716.
- S2CID 206950452.
- ^ PMID 22494821.
- PMID 21147548.
- S2CID 8357370.
- PMID 21353335.
- PMID 19695681.
- PMID 23098428.
- PMID 22808291. Review.
- PMID 8949653.
- PMID 22954224.
- PMID 11237011.
- PMID 22492626.
- PMID 22622578.
- PMID 10359645.
- ^ PMID 20062820.
- PMID 29794049.
- PMID 15382143.
- PMID 21301065.
- ^ Dean, Tim. "Cancer resembles life 1 billion years ago, say astrobiologists", Australian Life Scientist, 8 February 2011. Retrieved 15 February 2011.
- ^ Sterrer, W (August 2016). "Cancer - Mutational Resurrection of Prokaryote Endofossils" (PDF). Cancer Hypotheses. 1 (1): 1–15. Archived from the original (PDF) on 3 March 2022. Retrieved 8 May 2019.
- ^ S2CID 38445059.
- ^ S2CID 8040576.
- PMID 10647931.
- PMID 18356041.
- PMID 25731159.
- PMID 24868495.
- PMID 21940629.
- PMID 26634935.
- PMID 26674868.
- S2CID 22554281.
- PMID 26631474.
- PMID 22951309.
- PMID 26566817.
- PMID 22985997.
- PMID 26447335.
- PMID 24825771.
- PMID 26554912.
- S2CID 11182192.
- PMID 26502405.
- PMID 31015447.
- PMID 34580161.
- ^ PMID 26119834.
- PMID 20018552.
- PMID 25529612.
- PMID 25438737.
- PMID 24895166.
- ISSN 1872-3136.
- ISSN 0393-9375.
- PMID 19343108.
- S2CID 205383514.
- S2CID 16745745.
- PMID 2547513.
- S2CID 4234621.
- PMID 32877650.
- S2CID 678541.
- S2CID 36668814.
- PMID 5279523.
- S2CID 50724.
- PMID 21215367.
- Lay summary in: Wade N (10 January 2011). "Cancer Can Develop in Catastrophic Burst". The New York Times.
- PMID 10209681.
- PMID 16847081.
- PMID 16404738.
- PMID 20930071.
- PMID 30350310.
- PMID 11996414.
- PMID 7868485.
- PMID 26316793.
- PMID 24744586.
- ^ PMID 26668499.
- S2CID 18727504.
- PMID 26074077.
- ^ PMID 30781778.
- ^ PMID 22919587.
- PMID 26290630.
- ^ PMID 32143126.
- PMID 27239194.
- PMID 30146800.
- PMID 17487374.
- ISBN 978-1-60761-643-6.
- PMID 20539059.
- PMID 20945317. Review.
- PMID 22082348.
- PMID 23029077.
- PMID 22096249.
- PMID 18845242.
- PMID 12640109.
- PMID 17002552.
- PMID 15498793.
Further reading
- Tokar EJ, Benbrahim-Tallaa L, Waalkes MP (2011). "Chepter 14. Metal Ions in Human Cancer Development". In Sigel A, Sigel H, Sigel RK (eds.). Metal ions in toxicology: effects, interactions, interdependencies. Metal Ions in Life Sciences. Vol. 8. RSC Publishing. pp. 375–401. ISBN 978-1-84973-091-4.
- Dixon K, Kopras E (December 2004). "Genetic alterations and DNA repair in human carcinogenesis". Seminars in Cancer Biology. 14 (6): 441–8. PMID 15489137.
- Kleinsmith LJ (2006). Principles of cancer biology. San Francisco: Pearson Benjamin Cummings. ISBN 978-0-8053-4003-7.
- Sarasin A (November 2003). "An overview of the mechanisms of mutagenesis and carcinogenesis". Mutation Research. 544 (2–3): 99–106. PMID 14644312.
- Schottenfeld D, Beebe-Dimmer JL (2005). "Advances in cancer epidemiology: understanding causal mechanisms and the evidence for implementing interventions". Annual Review of Public Health. 26: 37–60. PMID 15760280.
- Tannock I, Hill R, Bristow R, Harrington L (2005). The basic science of oncology (4th ed.). New York: McGraw-Hill. ISBN 978-0-07-138774-3.
- Wicha MS, Liu S, Dontu G (February 2006). "Cancer stem cells: an old idea--a paradigm shift". Cancer Research. 66 (4): 1883–90, discussion 1895–6. PMID 16488983.
