Carotid artery stenosis
| Carotid artery stenosis | |
|---|---|
| Other names | TIA - carotid artery[1] |
 | |
| Carotid artery disease | |
| Specialty | Vascular surgery |
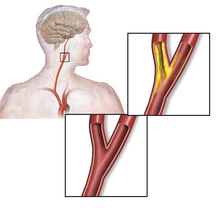
Carotid artery stenosis is a narrowing or constriction of any part of the carotid arteries, usually caused by atherosclerosis.[2]
Signs and symptoms
The
The plaque can be stable and asymptomatic, or it can be a source of embolization. Emboli break off from the plaque and travel through the circulation to blood vessels in the brain. As the vessels get smaller, an embolus can lodge in the vessel wall and restrict the blood flow to parts of the brain. This ischemia can either be temporary, yielding a transient ischemic attack (TIA), or permanent resulting in a thromboembolic stroke.[5]
Transient ischemic attacks are a warning sign and may be followed by severe permanent strokes, particularly within the first two days. TIAs by definition last less than 24 hours and frequently take the form of weakness or loss of sensation of a limb or the trunk on one side of the body or the loss of sight (amaurosis fugax) in one eye. Less common symptoms are artery sounds (bruits), or ringing in the ears (tinnitus).[6]
In asymptomatic individuals with a carotid stenosis, the risk of developing a stroke is increased above those without a stenosis. The risk of stroke is possibly related to the degree of stenosis on imaging. Some studies have found an increased risk with increasing degrees of stenosis[7] while other studies have not been able to find such a relationship.[8]
Pathophysiology
Atherosclerosis causes plaque to form within the carotid artery walls, usually at the fork where the common carotid artery divides into the internal and external carotid artery. The plaque build-up can narrow or constrict the artery lumen, a condition called stenosis. Rupture of the plaque can release atherosclerotic debris or blood clots into the artery. A piece of this material can break off and travel (embolize) up through the internal carotid artery into the brain, where it blocks circulation, and can cause death of the brain tissue, a condition referred to as ischemic stroke.[9]
Sometimes the
When the plaque does not cause symptoms, people are still at higher risk of stroke than the general population, but not as high as people with symptomatic stenosis. The incidence of stroke, including fatal stroke, is 1–2% per year. The surgical mortality of endarterectomy ranges from 1–2% to as much as 10%. Two large randomized clinical trials have demonstrated that carotid surgery done with a 30-day stroke and death risk of 3% or less will benefit asymptomatic people with ≥60% stenosis who are expected to live at least 5 years after surgery.[12][13] Surgeons are divided over whether asymptomatic people should be treated with medication alone or should have surgery.[14][15]
The common carotid artery is the large vertical artery in red. The blood supply to the carotid artery starts at the arch of the aorta (bottom). The carotid artery divides into the internal carotid artery and the external carotid artery. The internal carotid artery supplies the brain. Plaque often builds up at that division and causes a narrowing (stenosis). Pieces of plaque can break off and block the small arteries above in the brain, which causes a stroke. Plaque can also build up at the origin of the carotid artery at the aorta.[citation needed]
-
Carotid arteries
-
Section of carotid artery with plaque. Blood flows from the common carotid artery(bottom), and divides into the internal carotid artery (left) and external carotid artery (right). The atherosclerotic plaque is the dark mass on the left
Diagnosis


Carotid artery stenosis is usually diagnosed by color flow
Typically
One of several different imaging modalities, such as a computed tomography angiogram (CTA)[18][19][20] or magnetic resonance angiogram (MRA) may be useful. Each imaging modality has its advantages and disadvantages - Magnetic resonance angiography and CT angiography with contrast is contraindicated in patients with chronic kidney disease, catheter angiography has a 0.5% to 1.0% risk of stroke, MI, arterial injury or retroperitoneal bleeding. The investigation chosen will depend on the clinical question and the imaging expertise, experience and equipment available.[21]
For purpose of treatment, the degree of carotid stenosis is defined as:[citation needed]
- percent stenosis = ( 1 − ( minimum diameter within stenosis) / ( poststenotic diameter ) ) × 100%.
Screening
The
While routine population screening is not advised, the American Heart Association[23] and the Society for Vascular Surgery[24] recommend screening in those diagnosed with related medical conditions or have risk factors for carotid artery disease.[25] Screening is recommended for people who have:[citation needed]
- Vascular disease elsewhere in the body, including:
- Peripheral artery disease (PAD)
- Coronary artery disease (CAD)
- Atherosclerotic aortic aneurysm (AAA)
- Two or more of the following risk factors:
- High blood pressure (hypertension)
- High cholesterol (hyperlipidemia)
- Tobacco smoking
- Family history – First-degree relative diagnosed with atherosclerosis before age 60 or who had an ischemic stroke
The American Heart Association also recommends screening if a physician detects a carotid bruit, or murmur, over the carotid artery by listening through a stethoscope during a physical exam. For people with symptoms, the American Heart Association recommends initial screening using ultrasound.[citation needed]
Treatment
The goal of treating carotid artery stenosis is to reduce the risk of stroke. The type of treatment depends on the severity of the disease and includes:[citation needed]
- Lifestyle modifications including smoking cessation, eating a healthy diet and reducing sodium intake, losing weight, and exercising regularly.
- Medications to control high blood pressure and high levels of lipids in the blood.
- Surgical intervention for carotid artery revascularization.
Medication
Clinical guidelines (such as those of the
Revascularization
According to the American Heart Association, interventions beyond medical management is based upon whether patients have symptoms:[citation needed]
- Asymptomatic patients: severity of carotid artery stenosis, assessment of other medical conditions, life expectancy, and other individual factors; evaluation of the risks versus benefits; and patient preference are considered when determining whether surgical intervention should be performed.
- Symptomatic patients: it is recommended by the American Heart Association/
All interventions for carotid revascularization (carotid endarterectomy, carotid stenting, and transcarotid artery revascularization) carry some risk of stroke; however, where the risk of stroke over time from medical management alone is high, intervention may be beneficial. Carotid artery stenting and carotid endarterectomy have been found to have similar benefits in patients with severe degree of carotid artery stenosis.[30][31]
See also
References
- ^ "Carotid artery disease: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 29 May 2019.
- ^ "Atherosclerosis". The Lecturio Medical Concept Library. Retrieved 2 July 2021.
- S2CID 12109379.
- PMID 22031538.
- PMID 19423857.
- PMID 19423857.
- PMID 33609477.
- S2CID 7567725.
- ^ "What Are the Signs and Symptoms of Atherosclerosis? - NHLBI, NIH". www.nhlbi.nih.gov. 22 June 2016. Retrieved 2 July 2021.
- PMID 19423857.
- S2CID 19624935.
- .
- S2CID 22814764.
- PMID 18403770.
- ^ Drug Therapy Gains Favor to Avert Stroke, By THOMAS M. BURTON, Wall Street Journal, MARCH 3, 2009. Layman's summary of surgery vs. medication-only debate.
- PMID 15944595.
- PMID 31138235. Retrieved 2 July 2021.
- PMID 16418349.
- PMID 20724259.
- PMID 22547515.
- PMID 24047063.
- PMID 33528542.
- PMID 21282505.
- PMID 21889705.
- ^ "Guideline on the Management of Patients With Extracranial Carotid and Vertebral Artery Disease" (PDF). American Heart Association. Archived from the original (PDF) on 2017-11-17. Retrieved 2018-08-22.
- ^ Archived copy Archived 2017-11-17 at the Wayback Machine
- ^ "Carotid Artery Stenosis information. Internal carotis occlusion". patient.info. Retrieved 2018-10-08.
- PMID 9811916.
- S2CID 235169226.
- PMID 34469763.)
{{cite journal}}: CS1 maint: numeric names: authors list (link - PMID 28386040.


