Chest pain
| Chest pain | |
|---|---|
| Other names | Pectoralgia, stethalgia, thoracalgia, thoracodynia |
physical exam, medical tests[3] | |
| Treatment | Based on the underlying cause[1] |
| Medication | Aspirin, nitroglycerin[1][4] |
| Prognosis | Depends on the underlying cause[3] |
| Frequency | ~5% of ER visits[3] |
Chest pain is
Serious and relatively common causes include
Management of chest pain is based on the underlying cause.[1] Initial treatment often includes the medications aspirin and nitroglycerin.[1][4] The response to treatment does not usually indicate whether the pain is heart-related.[1] When the cause is unclear, the person may be referred for further evaluation.[3]
Chest pain represents about 5% of
Signs and symptoms
Chest pain may present in different ways depending upon the underlying diagnosis. Chest pain may also vary from person to person based upon age, sex, weight, and other differences. The type, severity, duration, and associated symptoms of chest pain can help guide diagnosis and further treatment.
Differential diagnosis
Causes of chest pain range from non-serious to serious to life-threatening.[10]
In adults the most common causes of chest pain include:
In children, the most common causes for chest pain are
Cardiovascular
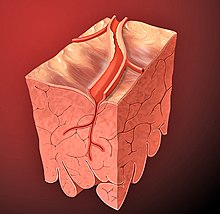
- Acute coronary syndrome
- Stable or unstable angina
- Myocardial infarction ("heart attack"): People usually complained of a pressure or squeezing sensation over the chest.[1] Other associated symptoms are: excessive sweating, nausea, vomiting, and weakness.[1] Chest pain is more commonly associated with anterior infarction because of left ventricular impairment; inferior infarction is more commonly associated with nausea, vomiting, and excessive sweating due to irritation of vagus nerve; lateral infarction is associated with left arm pain.
- Prinzmetal's angina: Chest pain is caused by coronary vasospasm. More common in women younger than 50 years. Person usually complain of chest pain at rest. It may occur early in the morning which awaken person from sleep.
- Cocaine use: This condition is suspected when a person with few or no risk of arteriosclerosis presented with non-traumatic chest pain. Ingestion of cocaine can cause vasoconstriction of coronary arteries, thus producing chest pain similar to heart attack. Symptoms can appear within one hour of cocaine use.
- second heart soundis heard in severe stenosis.
- Hypertrophic cardiomyopathy: It is the hypertrophy of interventricular septum that causes outflow obstruction of left ventricle. Dyspnea and chest pain commonly occurs during daily activities. Sometimes, syncope (fainting) may happen. On physical examination, significant findings include: loud systolic murmur and palpable triple apical impulse due to palpable presystolic fourth heart sound.
- Marfan's syndrome and hypertension. On examination, murmur of aortic insufficiency can be heard with unequal radial pulses.[14]
- coxsackie virus and echovirus, tuberculosis, autoimmune disease, uremia, and after myocardial infarction (Dressler syndrome). The chest pain is often pleuritic in nature (associated with respiration) which is aggravated when lying down and relieved on sitting forward, sometimes, accompanied by fever. On auscultation, pericardial friction rubcan be heard.
- Cardiac tamponade
- Arrhythmia: Atrial fibrillationand a number of other arrhythmias can cause chest pain.
- Myocarditis
- Mitral valve prolapse syndrome: Those affected are usually slim females presented with chest pain which is sharp in quality, localized at the apex, and relieved when lying down. Other symptoms include: shortness of breath, fatigue, and palpitations. On auscultation, midsystolic click followed by late systolic murmur can be heard, louder when person is in standing position.
- Aortic aneurysm
Respiratory
- Asthma is a common long-term inflammatory disease of the airways of the lungs. It is characterized by variable and recurring symptoms, reversible airflow obstruction, and bronchospasm. Symptoms include episodes of wheezing, coughing, chest tightness, and shortness of breath. Chest pain usually happens during a strenuous activity or heavy exercise.
- Bronchitis
- venous thromboembolism.
- Pneumonia[11]
- Hemothorax
- Pneumothorax: Those who are at a higher risk of developing pneumothorax are tall, slim male smokers who have had underlying lung diseases such as emphysema. Those affected can have a sharp chest pain which radiates to the shoulder of the same side. Physical examination revealed absent breath sounds and hyperresonance on the affected side of the chest.
- Pleurisy[11]
- Tuberculosis
- Tracheitis
- Lung cancer
Gastrointestinal

- Gastroesophageal reflux disease: The pain is aggravated when lying down or after meals. Persons may describe this as a heartburn. Besides, they may also complain of tasting bitter contents from the stomach.[11]
- Achalasia, nutcracker esophagus, and other motility disorders of the esophagus
- Diffuse esophageal spasm: Unlike cardiac chest pain, esophageal pain is not related to activity. The pain is usually associated with swallowing of hot or cold water.[11]
- Esophageal rupture: Those affected usually complain of sudden, severe, and constant pain that starts from the neck to the upper abdomen. The pain is aggravated by swallowing. On examination, neck swelling and crepitations can be felt due to subcutaneous emphysema as free air is entering from esophagus into the subcutaneous tissue.
- alendronate can induce esophagitis if not swallowed properly.[11]
- Functional dyspepsia
- Hiatus hernia
- Acute cholecystitis: Characterized by positive Murphy's sign where the person has a cessation of inhalationwhen the doctor places his finger at the right subcostal region of the abdomen.
- cholelithiasis (stones in the gallbladder), and hypertriglyceridemiaare risk factors for pancreatitis. It is a constant, boring pain in the upper abdomen.
- Perforated peptic ulcer: Sudden onset of severe pain in the upper abdomen which later develops into peritonitis(inflammation of tissues that lines the abdominal organs).
- Acute gastritis[11]
Chest wall
- Tietze's syndrome: An inflammation of a costochondral junction. Any movements or palpationof the chest can reproduce the symptoms.
- Spinal nerve problem
- Fibromyalgia
- Chest wall problems
- Radiculopathy
- Precordial catch syndrome: Another benign and harmless form of a sharp, localized chest pain often mistaken for heart disease.
- Breast conditions
- Herpes zoster (shingles): It is usually described as a burning sensation over the chest in a unilateral dermatomedistribution. However, diagnosis can be difficult because the pain usually appears before the characteristic rash is visible.
- Tuberculosis
- Osteoarthritis
- Bornholm disease
- Rib fracture[11]
Psychological
- Panic attack: Chest pain is a common symptom of panic attacks, with as high as 78% of persons describing chest pain with their worst panic attacks.[12] Overall chest pain is a symptom of up to 48% of sudden-onset panic attacks, and 10% of gradual-onset panic attacks.[12]
- Anxiety[11]
- Clinical depression
- Somatization disorder[11]
- Hypochondria
Others
- Hyperventilation syndrome often presents with chest pain and a tingling sensation of the fingertips and around the mouth.
- Da Costa's syndrome
- Carbon monoxide poisoning
- Sarcoidosis
- Lead poisoning
- Prolapsed intervertebral disc
- Thoracic outlet syndrome
- Adverse effect from certain medications
Diagnostic approach
History taking
Knowing a person's risk factors can be extremely useful in ruling in or ruling out serious causes of chest pain. For example,
Physical examination
Careful medical history and physical examination is essential in separating dangerous from trivial causes of disease, and the management of chest pain may be done on specialized units (termed medical assessment units) to concentrate the investigations. Occasionally, invisible medical signs will direct the diagnosis towards particular causes, such as
In the emergency department the typical approach to chest pain involves ruling out the most dangerous causes:
Risk scores
The Global Registry of Acute Coronary Events score and the Thrombosis in Myocardial Infarction performed at time of admission may help stratify persons into low, intermediate and high risk groups for acute coronary syndrome.[1] However these scores do not provide management guidelines for risk-stratified persons.
The HEART score, stratifies persons into low-risk and high-risk groups, and recommends either discharge or admission based upon the score.[1]
| Criteria | Point Value |
|---|---|
| History | |
| Highly suspicious | +2 |
| Moderately suspicious | +1 |
| Slightly suspicious | 0 |
| ECG | |
| Significant ST-depression | +2 |
| Nonspecific repolarization disturbance | +1 |
| Normal | 0 |
| Age | |
| ≥ 65 | +2 |
| 45-65 | +1 |
| ≤ 45 | 0 |
| Risk factors* | |
| ≥ 3 risk factors or history of atherosclerotic disease | +2 |
| 1-2 risk factors | +1 |
| No risk factors known | 0 |
| Troponin | |
| ≥ 3× normal limit | +2 |
| 1-3× normal limit | +1 |
| ≤ normal limit | 0 |
| *include diabetes mellitus , smoking, obesity
| |
Cumulative score:
- 0-3: 2.5% risk of adverse cardiac event. Patient's can be discharged with follow-up.
- 4-6: 20.3% risk of adverse cardiac event. Patients should be admitted to the hospital for trending of troponin and provocative testing.
- ≥7: 72.7% risk of adverse cardiac event, suggesting early invasive measures with these patients and close coordination with inpatient cardiology.
If
Medical tests
On the basis of the above, a number of tests may be ordered:[26]
- An electrocardiogram(ECG)
- Chest radiograph or chest x rays are frequently performed
- Echocardiography can be useful in patients with known cardiac disease or aortic dissection[8][27]
- CT scanning is used in the diagnosis of aortic dissection[27]
- V/Q scintigraphy or CT pulmonary angiogram (when a pulmonary embolism is suspected)[8]
- Blood tests:
- myocardialdamage)
- Complete blood count
- renal function (creatinine)
- Liver enzymes
- Creatine kinase (and CK-MB fraction in many hospitals)
- D-dimer (when suspicion for pulmonary embolism is present but low)
- serum lipase to exclude acute pancreatitis
Management
Management of chest pain varies with the underlying cause of the pain and the stage of care.
Prehospital care
Chest pain is a common symptom encountered by
Hospital care
Hospital care of chest pain begins with initial survey of a person's vital signs, airway and breathing, and level of consciousness.[1][8] This may also include attachment of ECG leads, cardiac monitors, intravenous lines and other medical devices depending on initial evaluation.[8] After evaluation of a person's history, risk factors, physical examination, laboratory testing and imaging, management begins depending on suspected diagnoses.[8] Depending upon the diagnosis, a person may be placed in the intensive care unit, admitted to the hospital, or be treated outpatient.[8] For persons with suspected cardiac chest pain or acute coronary syndrome, or other emergent diagnoses such as pneumothorax, pulmonary embolism, or aortic dissection, admission to the hospital is most often recommended for further treatment.[8]
Outpatient care
For people with non-cardiac chest pain, cognitive behavioral therapy might be helpful on an outpatient basis. A 2015 Cochrane review found that cognitive behavioral therapy might reduce the frequency of chest pain episodes the first three months after treatment.[32] For persons with chest pain due to gastroesophageal reflux disease, a proton-pump inhibitor has been shown to be the most effective treatment.[33] However, treatment with proton pump inhibitors has been shown to be no better than placebo in persons with noncardiac chest pain not caused by gastroesophageal reflux disease.[33] For musculoskeletal causes of chest pain, manipulation therapy or chiropractic therapy, acupuncture, or a recommendation for increased exercise are often used as treatment.[33] Studies have shown conflicting results on the efficacy of these treatments.[33] A combination therapy of nonsteroidal anti-inflammatory drugs and manipulation therapy with at-home exercises has been shown to be most effective in treatment of musculoskeletal chest pain.[9]
Epidemiology
Chest pain is a common
References
- ^ OCLC 915775025.
- ^ PMID 21960837.
- ^ PMID 29262011. Retrieved 22 June 2019.
- ^ ISBN 9781455733941.
- ISBN 9781573402125.
- ^ PMID 24207111.
- PMID 20380959.
- ^ OCLC 853286850.
- ^ PMID 24209723.
- ^ PMID 19932401.
- ^ PMID 20194155.
- ^ PMID 19158976.
- ISBN 978-1-4160-0087-7.
- PMID 27533160.
- ^ "NIH: Jackhammer esophagus Disorder Summary". U.S.A. National Institutes of Health, Genetic and Rare Diseases Information Center (GARD). Retrieved 2020-10-29.
- ^ "Mayo Clinic: Chest Pain Symptoms & causes". U.S.A. Mayo Clinic: Chest Pain, Symptoms & causes. Retrieved 2020-10-29.
- PMID 16304077.
- PMID 9786377.
- ^ PMID 28611898.
- ^ PMID 10866870.
- PMID 8541748.
- PMID 15336583.
- PMID 24141968.
- PMID 23465250.
- PMID 18665203.
- PMID 20219160.
- ^ PMID 16831999.
- ^ PMID 20956226.
- ^ "Highlights of the 2010 AHA Guidelines for CPR and ECC" (PDF). American Heart Association. Archived from the original (PDF) on 2017-01-06. Retrieved 2010-11-09.
- PMID 12655961.
- ^ "Entonox for the Treatment of Undiagnosed Chest Pain: Clinical Effectiveness and Guidelines" (PDF). Canadian Agency for Drugs and Technologies in Health. Archived from the original (PDF) on 29 September 2011. Retrieved 12 July 2011.
- PMID 26123045.
- ^ PMID 25111147.
- PMID 20380955.
- ^ "Products - Data Briefs - Number 43 - September 2010". www.cdc.gov. Retrieved 2018-01-19.
- ^ Skiner HG, Blanchard J, Elixhauser A (September 2014). "Trends in Emergency Department Visits, 2006-2011". HCUP Statistical Brief #179. Rockville, MD: Agency for Healthcare Research and Quality.
- S2CID 72035162.
