Chronic obstructive pulmonary disease
| Chronic obstructive pulmonary disease | |
|---|---|
| Other names | Chronic obstructive lung disease (COLD), chronic obstructive airway disease (COAD) |
| Frequency | 174.5 million (2015)[7] |
| Deaths | 3.2 million (2019)[3] |
Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms and airflow limitation.[8] GOLD 2024 defined COPD as a heterogeneous lung condition characterized by chronic respiratory symptoms (dyspnea, cough, sputum production and/or exacerbations) due to abnormalities of the airways (bronchitis, bronchiolitis) and/or alveoli (emphysema) that cause persistent, often progressive, airflow obstruction.[9]
The main symptoms of COPD include
Emphysema is defined as enlarged airspaces (
The most common cause of COPD is
Most cases of COPD can be prevented by reducing exposure to risk factors such as smoking and indoor and outdoor pollutants.
As of 2015, COPD affected about 174.5 million people (2.4% of the global population).[7] It typically occurs in males and females over the age of 35–40.[1][3] In 2019 it caused 3.2 million deaths, 80% occurring in lower and middle income countries,[3] up from 2.4 million deaths in 1990.[23][24] The number of deaths is projected to increase further because of continued exposure to risk factors and an aging population.[8] In the United States in 2010 the economic cost was put at US$32.1 billion and projected to rise to US$49 billion in 2020.[25] In the United Kingdom this cost is estimated at £3.8 billion annually.[26]
Signs and symptoms

Shortness of breath
A
Cough
The most often first symptom of COPD is a chronic cough, which may or may not be productive of mucus as phlegm. Phlegm coughed up as sputum can be intermittent and may be swallowed or spat out depending on social or cultural factors and is therefore not always easy to evaluate. However, an accompanying productive cough is only seen in up to 30% of cases. Sometimes limited airflow may develop in the absence of a cough.[4] Symptoms are usually worse in the morning.[30]
A chronic
Exacerbations
An acute exacerbation is a sudden worsening of signs and symptoms that lasts for several days. The key symptom is increased breathlessness, other more pronounced symptoms are of excessive mucus, increased cough and wheeze. A commonly found sign is air trapping giving a difficulty in complete exhalation.[31] The usual cause of an exacerbation is a
The number of exacerbations is not seen to relate to any stage of the disease; those with two or more a year are classed as frequent exacerbators and these lead to a worsening in the disease progression.[31] Frailty in ageing increases exacerbations and hospitalization.[41]
Acute exacerbations in COPD are often unexplained and thought to have many causes other than infections. A study has emphasized the possibility of a pulmonary embolism as sometimes being responsible in these cases. Signs can include pleuritic chest pain and heart failure without signs of infection. Such emboli could respond to anticoagulants.[42]
Other conditions
COPD often occurs along with a number of other conditions (
Anxiety and depression are often complications of COPD.
Cognitive impairment is common in those with COPD as it is for other lung conditions that affect airflow. Cognitive impairment is associated with the declining ability to cope with the basic activities of daily living.[48]
It is unclear if those with COPD are at greater risk of contracting COVID-19, though if infected they are at risk of hospitalization and developing severe COVID-19. Differentiating COVID-19 symptoms from an exacerbation is difficult; mild prodromal symptoms may delay its recognition and where they include loss of taste or smell COVID-19 is to be suspected.[36]
Definition
Many definitions of COPD in the past included chronic bronchitis and
Subtypes
It has since been recognized that COPD is more complex, with a diverse group of disorders of differing risk factors and clinical courses that has resulted in a number of subtypes or phenotypes of COPD being accepted and proposed.[51][52] The two classic emphysematous and chronic bronchitic phenotypes are fundamentally different conditions with unique underlying mechanisms.[10] Another subtype of COPD, categorized by some as a separate clinical entity, is asthma-COPD overlap, which is a condition sharing clinical features of both asthma and COPD.[53][54] Spirometry measures are inadequate for defining phenotypes and chest X-ray, CT and MRI scans have been mostly employed. Most cases of COPD are diagnosed at a late stage and the use of imaging methods would allow earlier detection and treatment.[10]
The identification and recognition of different phenotypes can guide appropriate treatment approaches. For example, the
Two inflammatory phenotypes show a phenotype stability: the neutrophilic inflammatory phenotype and the eosinophilic inflammatory phenotype.[56] Mepolizumab, a monoclonal antibody, has been shown to have benefit in treating the eosinophilic inflammatory type rather than the use of oral corticosteroids, but further studies have been called for.[57]
Another recognized phenotype is the frequent exacerbator.[58] The frequent exacerbator has two or more exacerbations a year, has a poor prognosis and is described as a moderately stable phenotype.[31]
A pulmonary vascular COPD phenotype has been described due to cardiovascular dysfunction.
The only genotype is the alpha-1 antitrypsin deficiency (AATD) genetic subtype and this has a specific treatment.[61]
Cause
The cause of the development of COPD is the exposure to harmful
A host factor of an
Alcohol abuse can lead to alcoholic lung disease and is seen to be an independent risk factor for COPD.[65][66]
Smoking
The primary risk factor for COPD globally is
Inhaled smoke triggers the release of excessive proteases in lungs, which then degrades elastin, the major component of alveoli.[17] Smoke also impairs the action of cilia, inhibiting mucociliary clearance that clears the bronchi of mucus, cellular debris and unwanted fluid.[17]
Other types of tobacco smoke, such as from cigar, pipe, water-pipe and hookah use, also confer a risk.[13] Water-pipe or hookah smoke appears to be as harmful or even more harmful than smoking cigarettes.[76]
Pollution

Exposure to particulates can bring about the development of COPD, or its exacerbations. Those with COPD are more susceptible to the harmful effects of particulate exposure that can cause acute exacerbations brought about by infections.[45] Black carbon also known as soot, is an air pollutant associated with an increased risk of hospitalization due to the exacerbations caused. Long-term exposure is indicated as an increased rate of mortality in COPD.[45] Studies have shown that people who live in large cities have a higher rate of COPD compared to people who live in rural areas.[82] Areas with poor outdoor air quality, including that from exhaust gas, generally have higher rates of COPD.[83] Urban air pollution significantly effects the developing lung and its maturation, and contributes a potential risk factor for the later development of COPD. The overall effect in relation to smoking is believed to be small.[13]
Poorly ventilated fires used for cooking and heating, are often fueled by coal or biomass such as wood and dry dung, leading to indoor air pollution and are one of the most common causes of COPD in developing countries. Women are affected more as they have a greater exposure.[13] These fuels are used as the main source of energy in 80% of homes in India, China and sub-Saharan Africa.[83]
Occupational exposure
Intense and prolonged exposure to workplace
Genetics
Genetics play a role in the development of COPD. It is more common among relatives of those with COPD who smoke than unrelated smokers.[13] The most well known genetic risk factor is alpha-1 antitrypsin deficiency (AATD) and this is the only genotype (genetic subtype) with a specific treatment.[61] This risk is particularly high if someone deficient in alpha-1 antitrypsin (AAT) also smokes.[86] It is responsible for about 1–5% of cases[86][87] and the condition is present in about three to four in 10,000 people.[88]
Mutations in MMP1 gene that encodes for interstitial collagenase are associated with COPD.[89]
The COPDGene study is an ongoing longitudinal study into the epidemiology of COPD, identifying phenotypes and looking for their likely association with susceptible genes. Genome wide analyses in concert with the International COPD Genetics Consortium has identified more than 80 genome regions associated with COPD and further studies in these regions has been called for. Whole genome sequencing is an ongoing collaboration (2019) with the National Heart, Lung and Blood Institute (NHLBI) to identify rare genetic determinants.[90]
Pathophysiology

COPD is a progressive
COPD develops as a significant and chronic inflammatory response to inhaled irritants which ultimately leads to bronchial and alveolar remodelling in the lung known as small airways disease.
Narrowing of the airways occurs due to inflammation and subsequent scarring within them. This contributes to the inability to breathe out fully. The greatest reduction in air flow occurs when breathing out, as the pressure in the chest is compressing the airways at this time.[98] This can result in more air from the previous breath remaining within the lungs when the next breath is started, resulting in an increase in the total volume of air in the lungs at any given time, a process called air trapping which is closely followed by hyperinflation.[98][99][93] Hyperinflation from exercise is linked to shortness of breath in COPD, as breathing in is less comfortable when the lungs are already partly filled.[100] Hyperinflation may also worsen during an exacerbation.[101] There may also be a degree of airway hyperresponsiveness to irritants similar to those found in asthma.[88]
Low oxygen levels and eventually, high carbon dioxide levels in the blood, can occur from poor gas exchange due to decreased ventilation from airway obstruction, hyperinflation and a reduced desire to breathe.[13] During exacerbations, airway inflammation is also increased, resulting in increased hyperinflation, reduced expiratory airflow and worsening of gas transfer. This can lead to low blood oxygen levels which if present for a prolonged period, can result in narrowing of the arteries in the lungs, while emphysema leads to the breakdown of capillaries in the lungs. Both of these conditions may result in pulmonary heart disease also classically known as cor pulmonale.[47]
Diagnosis

The diagnosis of COPD should be considered in anyone over the age of 35 to 40 who has
Spirometry
Screening using spirometry in those without symptoms has uncertain effect and is generally not recommended; however, it is recommended for those without symptoms but with a known risk factor.[43]
Assessment
| Grade | Activity affected |
|---|---|
| 1 | Only strenuous activity |
| 2 | Vigorous walking |
| 3 | With normal walking |
| 4 | After a few minutes of walking |
| 5 | With changing clothing |
| Severity | FEV1 % predicted |
|---|---|
| Mild (GOLD 1) | ≥80 |
| Moderate (GOLD 2) | 50–79 |
| Severe (GOLD 3) | 30–49 |
| Very severe (GOLD 4) | <30 |
A number of methods can be used to assess the affects and severity of COPD.
Use of screening questionnaires, such as COPD diagnostic questionnaire (CDQ), alone or in combination with hand-held flow meters is appropriate for screening of COPD in primary care.[110]
Other tests
A
A
-
Chest X-ray demonstrating severe COPD, displaying small heart size in comparison to the lungs
-
A lateral chest X-ray of a person with emphysema, displaying barrel chest and flat diaphragm
-
Lung bulla as seen on chest X-ray in a person with severe COPD
-
A severe case of bullous emphysema
-
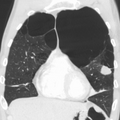
Axial CT image of the lung of a person with end-stage bullous emphysema
-
Very severe emphysema with lung cancer on the left (CT scan)
Differential diagnosis
COPD may need to be
Prevention
Most cases of COPD are potentially preventable through decreasing exposure to tobacco smoke and other indoor and outdoor pollutants.[20]
Smoking cessation
The policies of governments, public health agencies and antismoking organizations can reduce smoking rates by discouraging people from starting and encouraging people to stop smoking.[114] Smoking bans in public areas and places of work are important measures to decrease exposure to secondhand smoke and while many places have instituted bans, more are recommended.[83]
In those who smoke, stopping smoking is the only measure shown to slow down the worsening of COPD.[115][116] Even at a late stage of the disease, it can reduce the rate of worsening lung function and delay the onset of disability and death.[117] Often, several attempts are required before long-term abstinence is achieved.[114] Attempts over 5 years lead to success in nearly 40% of people.[118]
Some smokers can achieve long-term smoking cessation through willpower alone. Smoking, however, is highly addictive and many smokers need further support.[119] The chance of quitting is improved with social support, engagement in a smoking cessation program and the use of medications such as nicotine replacement therapy, bupropion, or varenicline.[114][116][118] Combining smoking-cessation medication with behavioral therapy is more than twice as likely to be effective in helping people with COPD stop smoking, compared with behavioral therapy alone.[120]
Occupational health
A number of measures have been taken to reduce the likelihood that workers in at-risk industries—such as coal mining, construction and stonemasonry—will develop COPD.[83] Examples of these measures include the creation of public policy,[83] education of workers and management about the risks, promoting smoking cessation, checking workers for early signs of COPD, use of respirators and dust control.[121][122] Effective dust control can be achieved by improving ventilation, using water sprays and by using mining techniques that minimize dust generation.[123] If a worker develops COPD, further lung damage can be reduced by avoiding ongoing dust exposure, for example by changing their work role.[124]
Pollution control
Both indoor and outdoor air quality can be improved, which may prevent COPD or slow the worsening of existing disease.[83] This may be achieved by public policy efforts, cultural changes and personal involvement.[125] Many developed countries have successfully improved outdoor air quality through regulations which has resulted in improvements in the lung function of their populations.[83] Individuals are also advised to avoid irritants of indoor and outdoor pollution.[20]
In developing countries one key effort is to reduce exposure to smoke from cooking and heating fuels through improved ventilation of homes and better stoves and chimneys.
Management
COPD currently has no cure,
A number of
In those with a severe exacerbation, antibiotics improve outcomes.
In those with end-stage disease, palliative care is focused on relieving symptoms.[136] Morphine can improve exercise tolerance.[21] Non-invasive ventilation may be used to support breathing and also reduce daytime breathlessness.[137][21]
Bronchodilators
Inhaled short-acting
Which type of long-acting agent,
Several short-acting β2 agonists are available, including
The two main anticholinergics used in COPD are
Corticosteroids
Inhaled corticosteroids are anti-inflammatories that are recommended by GOLD as a first-line maintenance treatment in COPD cases with repeated exacerbations.[159][160] Their regular use increases the risk of pneumonia in severe cases.[31] Studies have shown that the risk of pneumonia is associated with all types of corticosteroids; is related to the disease severity and a dose-response relationship has been noted.[159] Oral glucocorticoids can be effective in treating an acute exacerbation.[139] They appear to have fewer side effects than those given intravenously.[161] Five days of steroids work as well as ten or fourteen days.[162]
The use of corticosteroids is associated with a decrease in the number of lymphoid follicles (in the
PDE4 inhibitors
Phosphodiesterase-4 inhibitors (PDE4 inhibitors) are anti-inflammatories that improve lung function and reduce exacerbations in moderate to severe illness. Roflumilast is a PDE4 inhibitor used orally once daily to reduce inflammation, it has no direct bronchodilatory effects. It is essentially used in treating those with chronic bronchitis along with systemic corticosteroids.[57] Reported adverse effects of roflumilast appear early in treatment, become less with continued treatment and are reversible. One effect is dramatic weight loss and its use is to be avoided in underweight people. It is also advised to be used with caution in those who have depression.[57]
Other medications
Long-term
Recent studies show that metformin plays a role in reducing systemic inflammation by reducing biomarker levels that are increased during COPD exacerbations.[171]
Oxygen therapy
Rehabilitation
Pulmonary rehabilitation is a program of exercise, disease management and counseling, coordinated to benefit the individual.[178] A severe exacerbation leads to hospital admission, high mortality and a decline in the ability to carry out daily activities. Following a hospital admission pulmonary rehabilitation has been shown to significantly reduce future hospital admissions, mortality and improve quality of life.[55]
The optimal exercise routine, use of noninvasive ventilation during exercise and intensity of exercise suggested for people with COPD, is unknown.[179][180] Performing endurance arm exercises improves arm movement for people with COPD and may result in a small improvement in breathlessness.[181] Performing arm exercises alone does not appear to improve quality of life.[181] Pursed-lip breathing exercises may be useful.[27] Tai chi exercises appear to be safe to practice for people with COPD and may be beneficial for pulmonary function and pulmonary capacity when compared to a regular treatment program.[182] Tai Chi was not found to be more effective than other exercise intervention programs.[182] Inspiratory and expiratory muscle training (IMT, EMT) have been suggested and may provide some improvements when compared to no treatment.[183] A combination of IMT and walking exercises at home may help limit breathlessness in cases of severe COPD.[184] Additionally, the use of low amplitude high velocity joint mobilization together with exercise improves lung function and exercise capacity.[185] The goal of spinal manipulation therapy is to improve thoracic mobility in an effort to reduce the work on the lungs during respiration, however, the evidence supporting manual therapy for people with COPD is very weak.[185][186]
Being either underweight or overweight can affect the symptoms, degree of disability and prognosis of COPD. People with COPD who are underweight can improve their breathing muscle strength by increasing their calorie intake. When combined with regular exercise or a pulmonary rehabilitation program, this can lead to improvements in COPD symptoms. Supplemental nutrition may be useful in those who are malnourished.[21][188]
Management of exacerbations
People with COPD can experience
Room temperatures
Maintaining room temperatures of at least 21 °C [70 °F] for a minimum of nine hours a day was associated with better health in those with COPD, especially for smokers.[191] The World Health Organization (WHO) recommends indoor temperatures of a slightly higher range between 18 °C and 24 °C [65 °F and 75 °F].[192]
Room humidity
For people with COPD, the ideal indoor humidity levels are 30–50% RH. Maintaining indoor humidity can be difficult in the winter, especially in cold climates where the heating system is constantly running.[193]
Keeping the indoor relative humidity above 40% RH significantly reduces the infectivity of aerosolized viruses.[194]
Procedures for emphysema
There are a number of procedures to
Surgical
For severe emphysema that has proved unresponsive to other therapies
Bronchoscopic
Minimally invasive bronchoscopic procedures may be carried out to reduce lung volume. These include the use of valves, coils, or thermal ablation.[21][198] Endobronchial valves are one-way valves that may be used in those with severe hyperinflation resulting from advanced emphysema; a suitable target lobe and no collateral ventilation are required for this procedure. The placement of one or more valves in the lobe induces a partial collapse of the lobe that ensures a reduction in residual volume that improves lung function, the capacity for exercise and quality of life.[199]
The placement of
Both of these techniques are associated with adverse effects including persistent air leaks and cardiovascular complications. Thermal vapor ablation has an improved profile. Heated water vapor is used to target lobe regions which leads to permanent fibrosis and volume reduction. The procedure is able to target individual lobe segments, can be carried out regardless of collateral ventilation and can be repeated with the natural advance of emphysema.[201]
Other surgeries
In very severe cases
Prognosis


| no data ≤110 110–220 220–330 330–440 440–550 550–660 | 660–770 770–880 880–990 990–1100 1100–1350 ≥1350 |
COPD is progressive and can lead to premature death. It is estimated that 3% of
There are many variables affecting the long-term outcome in COPD and GOLD recommends the use of a composite test (
NICE recommends against the use of BODE for the prognosis assessment in stable COPD; factors such as exacerbations and
Epidemiology
Estimates of prevalence have considerable variation due to differences in analytical and surveying approach and the choice of diagnostic criteria.[207] An estimated 384 million people aged 30 years or more had COPD in 2010, corresponding to a global prevalence of 12%.[8] The disease affects men and women.[3] The increase in the developing world between 1970 and the 2000s is believed to be related to increasing rates of smoking in this region, an increasing population and an aging population due to fewer deaths from other causes such as infectious diseases.[135] Some developed countries have seen increased rates, some have remained stable and some have seen a decrease in COPD prevalence.[135]
Around three million people die of COPD each year.[8] In some countries, mortality has decreased in men but increased in women.[208] This is most likely due to rates of smoking in women and men becoming more similar.[88] A higher rate of COPD is found in those over 40 years and this increases greatly with advancing age with the highest rate found in those over 60 years.[8] Sex differences in the anatomy of the respiratory system include smaller airway lumens and thicker airway walls in women, which contribute to a greater severity of COPD symptoms like dyspnea and frequency of COPD exacerbation.[209]
In the UK, three million people are reported to be affected by COPD – two million of these being undiagnosed. On average, the number of COPD-related deaths between 2007 and 2016 was 28,600. The estimated number of deaths due to occupational exposure was estimated to be about 15% at around 4,000.[207] In the United States in 2018, almost 15.7 million people had been diagnosed with COPD and it is estimated that millions more have not been diagnosed.[210]
In 2011, there were approximately 730,000 hospitalizations in the United States for COPD.[211] Globally, COPD in 2019 was the third-leading cause of death. In low-income countries, COPD does not appear in the Top 10 causes of death; in other income groups, it is in the Top 5.[212]
History
The name chronic obstructive pulmonary disease is believed to have first been used in 1965.[213] Previously it has been known by a number of different names, including chronic obstructive bronchopulmonary disease, chronic airflow obstruction, chronic obstructive lung disease, nonspecific chronic pulmonary disease, diffuse obstructive pulmonary syndrome.[213]
The terms emphysema and chronic bronchitis were formally defined as components of COPD in 1959 at the CIBA guest symposium and in 1962 at the American Thoracic Society Committee meeting on Diagnostic Standards.[213]
Early descriptions of probable emphysema began in 1679 by T. Bonet of a condition of "voluminous lungs" and in 1769 by
Air pollution and the increase in cigarette smoking in Great Britain at the start of the 20th century led to high rates of chronic lung disease, though it received little attention until the Great Smog of London in December 1952. This spurred epidemiological research in the United Kingdom, Holland and elsewhere.[215] In 1953, George L. Waldbott, an American allergist, first described a new disease he named smoker's respiratory syndrome in the 1953 Journal of the American Medical Association. This was the first association between tobacco smoking and chronic respiratory disease.[216]
Modern treatments were developed during the second half of the 20th century. Evidence supporting the use of steroids in COPD was published in the late 1950s. Bronchodilators came into use in the 1960s following a promising trial of isoprenaline. Further bronchodilators, such as short-acting salbutamol, were developed in the 1970s and the use of long-acting bronchodilators began in the mid-1990s.[217]
Society and culture
It is generally accepted that COPD is widely underdiagnosed and many people remain untreated. In the US the
Economics
Globally, as of 2010, COPD is estimated to result in economic costs of $2.1 trillion, half of which occurring in the developing world.[219] Of this total an estimated $1.9 trillion are direct costs such as medical care, while $0.2 trillion are indirect costs such as missed work.[220] This is expected to more than double by 2030.[219] In Europe, COPD represents 3% of healthcare spending.[125] In the United States, costs of the disease are estimated at $50 billion, most of which is due to exacerbation.[112] COPD was among the most expensive conditions seen in U.S. hospitals in 2011, with a total cost of about $5.7 billion.[211]
Research
A new cryogenic treatment aimed at the chronic bronchitic subtype using a liquid nitrogen metered cryospray is being trialled and was due to complete in September 2021.[222][223]
Stem-cell therapy using mesenchymal stem cells has the potential to restore lung function and thereby improve quality of life. In June 2021 eight clinical trials had been completed and seventeen were underway. Overall, stem cell therapy has proved to be safe. The trials include the use of stem cells from different sources such as adipose tissue, bone marrow and umbilical cord blood.[224]
A procedure known as targeted lung denervation is being trialled and has been used as part of a clinical trial (2021) in a hospital in the UK. The new minimally invasive procedure which takes about an hour to carry out, places electrodes to destroy branches of the vagus nerve in the lungs. The vagus nerve is responsible for both muscle contraction and mucus secretion, which results in narrowing the airways. In those with COPD these nerves are overactive, usually as a result of smoking damage and the constant mucus secretion and airway constriction leads to the symptoms of cough, shortness of breath, wheeze and tightness of the chest.[225]
The effectiveness of alpha-1 antitrypsin augmentation treatment for people who have alpha-1 antitrypsin deficiency is unclear.[226] A later clinical trial of double-dosing has shown some improvements in slowing the breakdown of elastin and the progression of emphysema with further studies being called for.[227]
Mass spectrometry is being studied as a diagnostic tool in COPD.[228]
Research continues into the use of
Evidence is growing for the effectiveness of Astaxanthin against lung disease including COPD. Astaxanthin is a potent antioxidant with anti-inflammatory properties and more trials are said to be needed into its use.[230]
American COPD patients and their caregivers consider the following COPD-related research areas as the most important:
- family/social/community research
- patients' well‐being
- curative research
- biomedical therapies
- policy
- holistic therapies.[231]
Other animals
Chronic obstructive pulmonary disease may occur in a number of other animals and may be caused by exposure to tobacco smoke.[232] Most cases of the disease, however, are relatively mild.[233] In horses it is known as recurrent airway obstruction (RAO) or heaves. RAO can be quite severe and most often is linked to exposure to common allergens.[234] COPD is also commonly found in old dogs.[235]
See also
References
- ^ a b c d e f g h i "Chronic obstructive pulmonary disease". nice.org. Retrieved 5 July 2021.
- ^ a b c "Chronic obstructive pulmonary disease (COPD) - Complications | BMJ Best Practice". bestpractice.bmj.com. Retrieved 11 July 2021.
- ^ a b c d e f g "Chronic obstructive pulmonary disease (COPD)". Fact Sheets. World Health Organization. Retrieved 1 July 2021.
- ^ a b c d e f g h i j k l Gold Report 2021, pp. 20–27, Chapter 2: Diagnosis and initial assessment.
- ^ a b c d Gold Report 2021, pp. 33–35, Chapter 2: Diagnosis and initial assessment.
- ^ a b c d e f g h i j k Gold Report 2021, pp. 40–46, Chapter 3: Evidence supporting prevention and maintenance therapy.
- ^ PMID 27733282.
- ^ a b c d e f g h i j k l Gold Report 2021, pp. 4–8, Chapter 1: Definition and overview.
- ^ "2024 GOLD Report". Global Initiative for Chronic Obstructive Lung Disease - GOLD. Retrieved 2024-02-23.
- ^ PMID 30989390.
- ^ a b "ICD-11 - ICD-11 for Mortality and Morbidity Statistics". icd.who.int. Retrieved 30 June 2021.
- PMID 33313212.
- ^ a b c d e f g h i j k l m n o p q r Gold Report 2021, pp. 8–14, Chapter 1: Definition and overview.
- ^ PMID 29849481.
- ^ GINA and GOLD joint guidelines Ga (2014). "Asthma COPD and asthma COPD overlap syndrome (ACOS)" (PDF). GINA Guidelines.
- S2CID 32732993.
- ^ a b c d e "Chronic obstructive pulmonary disease (COPD) - Aetiology | BMJ Best Practice". bestpractice.bmj.com. Retrieved 25 November 2022.
- ^ a b "COPD causes - occupations and substances". www.hse.gov.uk. Retrieved 3 July 2021.
- PMID 27207325.
- ^ a b c d Gold Report 2021, pp. 80–83, Chapter 4: Management of stable COPD.
- ^ a b c d e f g Gold Report 2021, pp. 60–65, Chapter 3: Evidence supporting prevention and maintenance therapy.
- S2CID 211476101.
- PMID 27733281.
- PMID 25530442.
- ^ "COPD Costs". www.cdc.gov. 5 July 2019.
- ^ "COPD commissioning toolkit" (PDF). www.assets.publishing.service.gov.uk. Retrieved 18 July 2021.
- ^ PMID 28969859.
- ^ Gold Report 2021, pp. 90–96, Chapter 4: Management of stable COPD.
- PMID 31673990.
- ^ PMID 34209651.
- ^ a b c d e f g h i j Gold Report 2021, pp. 104–109, Chapter 5: Management of exacerbations.
- ^ "Common Colds". Centers for Disease Control and Prevention. 7 October 2020. Archived from the original on June 18, 2023. Retrieved 20 August 2021.
- PMID 32655557.
- S2CID 230608674.
- ^ US EPA O (19 April 2016). "Particulate Matter (PM) Basics". www.epa.gov. Retrieved 21 July 2021.
- ^ PMID 33146552.
- S2CID 221097739.
- ^ US EPA O (13 August 2019). "Health Effects Attributed to Wildfire Smoke". www.epa.gov. Retrieved 21 July 2021.
- ^ "Forest Fires and Lung Health". the lung association. 25 August 2014. Retrieved 21 July 2021.
- ^ "Bushfire smoke". National Centre for Farmer Health. 19 March 2014. Retrieved 21 July 2021.
- PMID 33880018.
- S2CID 7181799.
- ^ a b c d e f g Gold Report 2021, pp. 26–33, Chapter 2: Diagnosis and initial assessment.
- PMID 28496314.
- ^ PMID 30704059.
- PMID 30822464.
- ^ PMID 23662171.
- ^ Gold Report 2021, pp. 121–126, Chapter 6: COPD and comorbidities.
- ^ ISBN 978-0-323-52371-4.)
{{cite book}}: CS1 maint: location missing publisher (link - S2CID 7124561. Retrieved 30 August 2021.
- PMID 30810542.
- PMID 31740261.
- PMID 26398072.
- PMID 34168440.
- ^ PMID 29062228.
- ^ S2CID 149444134.
- ^ a b c d e Gold Report 2021, pp. 54–58, Chapter 3: Evidence supporting prevention and maintenance therapy.
- PMID 34026786.
- PMID 34285903.
- PMID 24741301.
- ^ PMID 31730394.
- ^ "FAQs Dust - Health and Safety Executive (HSE)".
- ^ PMID 30111617.
- PMID 29339516.
- ^ PMID 33080339.
- ^ PMID 31278041.
- S2CID 239523761.
- PMID 31229291.
- ^ ISBN 978-0-19-165478-7.
- ISBN 978-0-8493-7588-0.
- ISBN 978-1-84619-316-3.
- PMID 32800188.
- S2CID 9360093.
- ^ "Tobacco". Fact Sheets. World Health Organization. Retrieved 12 July 2021.
- PMID 29520136.
- S2CID 155103502.
- ^ PMID 28483343.
- S2CID 59233744.
- PMID 27507173.
- PMID 27763599.
- ^ "Access to clean fuels and technologies for cooking". Our World in Data. Retrieved 15 February 2020.
- PMID 16611654.
- ^ PMID 22793948.
- ISBN 978-0-323-29245-0.
- ISBN 978-0-12-374001-4.
- ^ PMID 22793939.
- PMID 22761482.
- ^ ISBN 978-0-07-174889-6.
- ^ "Home - Gene - NCBI". www.ncbi.nlm.nih.gov. Retrieved 17 July 2022.
- PMID 31154041.
- S2CID 195844108.
- ISBN 978-0-323-35317-5.
- ^ PMID 33116475.
- S2CID 254665705.
- PMID 37221593.
- S2CID 212416323.
- ^ PMID 30832670.
- ^ PMID 15640341.
- ISBN 978-1-4443-2948-3.
- S2CID 20644418.
- PMID 16996896.
- ^ a b c "Chronic obstructive pulmonary disease - NICE Pathways". pathways.nice.org.uk. 9 April 2020. Retrieved 29 June 2021.
- ^ S2CID 18830625.
- ^ ISBN 978-0-7817-8870-0.
- ^ National Institute for Health and Clinical Excellence. Clinical guideline 101: Chronic Obstructive Pulmonary Disease. London, June 2010.
- PMID 22793942.
- PMID 28898975.
- ^ a b "Chronic obstructive pulmonary disease (COPD) - Criteria | BMJ Best Practice". bestpractice.bmj.com. Retrieved 2 July 2021.
- ^ "COPD Assessment Test (CAT)". American Thoracic Society. Archived from the original on December 3, 2013. Retrieved November 29, 2013.
- PMID 34322411.
- ^ "saber sheath trachea | Search | Radiopaedia.org". Radiopaedia. Retrieved 13 August 2021.
- ^ PMID 22878278.
- ^ BTS COPD Consortium (2005). "Spirometry in practice – a practical guide to using spirometry in primary care". pp. 8–9. Archived from the original on 26 August 2014. Retrieved 25 August 2014.
- ^ ISBN 978-92-4-156240-9. Archived from the originalon 2008-09-15.
- PMID 23741944.
- ^ a b "Chronic obstructive pulmonary disease in over 16s: diagnosis and management | Guidance and guidelines | NICE". www.nice.org.uk. 23 June 2010. Retrieved 2018-06-05.
- ISBN 978-0-7020-2763-5.
- ^ PMID 23457163.
- ^ "Coping with cravings". nhs.uk. 27 April 2018. Retrieved 15 July 2021.
- PMID 27545342.
- ISBN 978-0-7817-5098-1.
- ISBN 978-0-7817-6299-1.
- ^ "Wet cutting". Health and Safety Executive. Archived from the original on December 3, 2013. Retrieved November 29, 2013.
- ISBN 978-0-7817-5273-2.
- ^ PMID 22878278.
- ^ "Chronic obstructive pulmonary disease (COPD) - Treatment - NHS". 20 October 2017.
- ^ CDC (2024-01-18). "RSV information for healthcare providers". Centers for Disease Control and Prevention. Retrieved 2024-02-23.
- ^ "2024 GOLD Report". Global Initiative for Chronic Obstructive Lung Disease - GOLD. Retrieved 2024-02-23.
- PMID 27990628.
- PMID 28777450.
- PMID 30630893.
- ^ PMID 30371937.
- PMID 22793945.
- ^ "Fluoroquinolone Antibacterial Drugs: Drug Safety Communication – FDA Advises Restricting Use for Certain Uncomplicated Infections". FDA. 12 May 2016. Archived from the original on 16 May 2016. Retrieved 16 May 2016.
- ^ PMID 22314182.
- PMID 32638839.
- PMID 32016309.
- PMID 30085570. Retrieved 27 July 2021.
- ^ a b c Gold Report 2021, pp. 48–52, Chapter 3: Evidence supporting prevention and maintenance therapy.
- PMID 26490945.
- PMID 30521694.
- ^ a b "Recommendations | Chronic obstructive pulmonary disease in over 16s: diagnosis and management | Guidance | NICE". www.nice.org.uk. 5 December 2018. Retrieved 1 August 2021.
- ^ PMID 21276815.
- PMID 22161409.
- S2CID 45383688.
- ^ PMID 25575340.
- PMID 23378756.
- PMID 22972099.
- PMID 37276335.
- PMID 30401700.
- ^ PMID 25046211.
- PMID 26391969.
- PMID 22764216.
- S2CID 3530290.
- S2CID 24973904.
- ^ PMID 25234126.
- PMID 28631387.
- PMID 26604738.
- ^ PMID 34267661.
- PMID 26831345.
- PMID 25178099.
- PMID 29553157.
- PMID 38054551.
- S2CID 35183033.
- ^ PMID 30376188.
- PMID 23352223.
- PMID 31107966.
- ^ "Erdosteine". NICE. Retrieved 20 July 2021.
- PMID 34199312.
- ^ "Bronchitis". nhs.uk. 17 October 2017.
- PMID 31737323.
- ^ PMID 31544111.
- PMID 27886372.
- ISBN 978-93-5090-353-7.
- ^ PMID 18838559.
- ^ "2024 GOLD Report". Global Initiative for Chronic Obstructive Lung Disease - GOLD. Retrieved 2024-02-23.
- S2CID 265751322.
- ^ "Pulmonary Rehabilitation". medlineplus.gov. Retrieved 9 September 2021.
- PMID 24353107.
- PMID 24823712.
- ^ PMID 27846347.
- ^ PMID 27272131.
- PMID 36606682.
- PMID 20420957.
- ^ PMID 26700633.
- PMID 30738792.
- ^ PMID 22419331.
- PMID 23235577.
- PMID 27569680.
- ^ Wise R. "Chronic Obstructive Pulmonary Disease (COPD)". Pulmonary Disorders: Merck Manuals Professional Edition. Archived from the original on 28 December 2016. Retrieved 16 December 2016.
- PMID 18367496.
- S2CID 25962322.
- ^ "Humidifiers: Ease skin, breathing symptoms". Mayo Clinic.
- PMID 23460865.
- ^ a b Gold Report 2021, pp. 92–96, Chapter 4: Management of stable COPD.
- S2CID 73428098.
- ^ S2CID 221145423.
- ^ a b "1 Recommendations | Endobronchial valve insertion to reduce lung volume in emphysema | Guidance | NICE". www.nice.org.uk. 20 December 2017. Retrieved 7 July 2021.
- PMID 33345947.
- PMID 30210833.
- S2CID 78181696.
- S2CID 56486118.
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. Archived from the original on 2009-11-11. Retrieved Nov 11, 2009.
- ^ S2CID 205967479.
- PMID 23245607.
- ^ Gold Report 2021, pp. 26–33, Chapter 2:Diagnosis and assessment.
- ^ a b "COPD prevalence". NICE. Retrieved 18 July 2021.
- PMID 22927753.
- PMID 17431226.
- ^ "Basics About COPD". Chronic Obstructive Pulmonary Disease (COPD). Center for Disease Control. 9 June 2021. Retrieved 18 July 2021.
- ^ from the original on 2017-03-14.
- ^ "The top 10 causes of death". Fact Sheets. World Health Organization.
- ^ PMID 18046898.
- ^ ISBN 978-0-07-164109-8. Archived from the original(PDF) on 2016-03-03. Retrieved 2008-11-11.
- .
- ^ Waldbott GL (1965). A struggle with Titans. Carlton Press. p. 6.
- PMID 15849329.
- ^ "November is National COPD Awareness Month | NHLBI, NIH". www.nhlbi.nih.gov. Retrieved 21 July 2021.
- ^ ISBN 978-1-107-03959-9.
- ^ Bloom D (2011). The Global Economic Burden of Noncommunicable Diseases (PDF). World Economic Forum. p. 24. Archived (PDF) from the original on 2015-02-04.
- ^ "NIH study shows hyaluronan is effective in treating chronic lung disease". National Institutes of Health (NIH). 1 February 2021. Retrieved 7 August 2021.
- PMID 30622803.
- ^ "A Prospective Safety and Feasibility Study of the RejuvenAir™ System Metered Cryospray Therapy for Chronic Bronchitis Patients". clinicaltrials.gov. 25 January 2021. Retrieved 16 August 2021.
- PMID 34250959.
- ^ "First UK patients get pioneering new treatment for serious lung disease | Royal Brompton & Harefield hospitals". www.rbht.nhs.uk. Retrieved 4 August 2021.
- PMID 27644166.
- PMID 30965011.
- PMID 30907495.
- PMID 21735417.
- PMID 33179051.
- PMID 34865193.
- ISBN 978-1-118-70115-7.
- PMID 17684336.
- ^ "Recurrent Airway Obstruction in Horses - Respiratory System". Veterinary Manual. Retrieved 7 July 2021.
- PMID 2646821.
Works cited
- Global Strategy for Prevention, Diagnosis and Management of COPD: 2021 Report (PDF). Global Initiative for Chronic Obstructive Lung Disease. 25 November 2020. Retrieved 28 June 2021.
External links
- WHO fact sheet on COPD
- Chronic obstructive pulmonary disease at Curlie
- "COPD". MedlinePlus. U.S. National Library of Medicine.