Chronic pancreatitis
| Chronic pancreatitis | |
|---|---|
| Other names | Pancreatitis – chronic – discharge[1] |
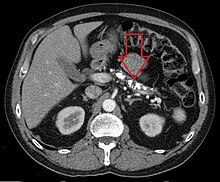 | |
| Axial CT showing multiple calcifications in the pancreas in a patient with chronic pancreatitis | |
| Specialty | Gastroenterology |
| Symptoms | Nausea and vomiting[2][3] |
| Complications | Exocrine pancreatic insufficiency, Endocrine pancreatic insufficiency (Type 3c diabetes), pancreatic pseudocyst,[4] pancreatic cancer,[4] vitamin deficiency (fat-soluble vitamins)[4] |
| Causes | Alcohol(ism), Immune disorder[5] |
| Diagnostic method | Serum trypsinogen, Fecal fat test[2] |
| Treatment | Pain medicines, avoiding alcohol(and smoking), among other possible management efforts[2] |
| Frequency | 50 per 100,000 persons (prevalence) |
Chronic pancreatitis is a long-standing
Signs and symptoms
- Upper abdominal pain: Upper abdominal pain which increases after drinking or eating, lessens when fasting or sitting and leaning forward. Some people may not suffer pain.[2][3]
- Nausea and vomiting[2][3]
- Steatorrhea: Frequent, oily, foul-smelling bowel movements. Damage to the pancreas reduces the production of pancreatic enzymes that aid digestion, which can result in malnutrition. Fats and nutrients are not absorbed properly, leading to loose, greasy stool known as steatorrhea.[2][3]
- Weight loss even when eating habits and amounts are normal.[2]
- pancreatic islets to produce insulin to regulate glucose levels, leading to diabetes type 3c. Symptoms of diabetes type 3c are due to elevated sugar and may include increased hunger and thirst, frequent urination, weight loss, fatigue, and blurry vision.[8]
There have been three symptom profiles described in those with chronic pancreatitis. Type A involves intermittent, severe symptom flare-ups with or without objective pancreatitis amongst a background of symptom-free periods. The type A symptom profile is usually more common early in the course of chronic pancreatitis.[4] Type B chronic pancreatitis involves chronic pain accompanied by intermittent severe attacks.[4] And, the type C symptom profile of chronic pancreatitis involves chronic, long-term, severe pain without interspersed acute flare-ups or symptom exacerbations.[4]
Causes
Among the causes of chronic pancreatitis are the following:[5]
- Alcohol
- Autoimmune disorders
- Intraductal obstruction
- Idiopathic pancreatitis
- Tumors
- Ischemia
- Calcific stones
Chronic
Pathophysiology

The mechanism of chronic pancreatitis viewed from a genetic standpoint indicates early onset of severe
Diagnosis
The diagnosis of chronic pancreatitis is made based on the history and characteristics of symptoms combined with findings on radiologic imaging.[4] Serum amylase and lipase may be moderately elevated in cases of chronic pancreatitis.
Symptoms of
When chronic pancreatitis is caused by genetic factors, elevations in
On MRI scan, there is a low T1 signal due to inflammation, fibrosis, focal lesions, and calcifications. In those who are given a contrast agent, there would be a higher T1 signal with late gadolinium enhancement due to compression from the fibrotic areas. The overall thickness of the pancreas will be reduced.[12]
Treatment
The different treatment options for the management of chronic pancreatitis are medical measures, therapeutic endoscopy, and surgery.
Endoscopic treatments, including removal of stones in the
Behavioral treatments such as
Pancreatic enzymes
Pancreatic enzyme replacement is often effective in treating the malabsorption and steatorrhea associated with chronic pancreatitis. Treatment of CP consists of the administration of a solution of pancreatic enzymes with meals. Some patients do have pain reduction with enzyme replacement, and since they are relatively safe, giving enzyme replacement to a chronic pancreatitis patient is an acceptable step in treatment for most patients. Treatment may be more likely to be successful in those without the involvement of large ducts and those with idiopathic pancreatitis.[16]
Surgery
Surgery to treat chronic pancreatitis tends to be divided into two areas – resectional and drainage procedures. Among the reasons to opt for surgery is if there is a pseudocyst,
Epidemiology
The annual incidence of chronic pancreatitis is 5 to 12 per 100,000 persons, the prevalence is 50 per 100,000 persons.[18] It has been reported that the pancreas is able to absorb radioactive
See also
References
- ^ a b "Chronic pancreatitis: MedlinePlus Medical Encyclopedia". www.nlm.nih.gov. Retrieved 2015-11-29.
- ^ a b c d e f g
"Chronic pancreatitis".
When scarring of the pancreas occurs, the organ is no longer able to make the right amount of these enzymes. As a result, your body may be unable to digest fat and key elements of food. Damage to the parts of the pancreas that make insulin may lead to diabetes
- ^ a b c d "What is chronic pancreatitis?".
diabetes; upper abdominal pain that is frequently chronic and debilitating. Pain is the most common symptom of chronic pancreatitis. The pain may increase after drinking or eating and lessens when fasting or sitting and leaning forward. However, some people with chronic pancreatitis report little to no pain; from google (chronic pancreatitis smelly poop) result 1
- ^ S2CID 247221549.
- ^ a b c "Chronic Pancreatitis: Practice Essentials, Background, Pathophysiology". 2018-11-11.
{{cite journal}}: Cite journal requires|journal=(help) - PMID 24259953.
- ^ "Chronic Pancreatitis". The Lecturio Medical Concept Library. 11 November 2020. Retrieved 9 July 2021.
- ^ Action, Pancreatic Cancer. "Type 3C diabetes (secondary diabetes) Pancreatic Cancer Symptoms". Pancreatic Cancer Action.
- ^ Choices, NHS. "Chronic pancreatitis – Causes – NHS Choices". www.nhs.uk. Retrieved 2015-11-29.
- PMID 24259953.
- ISBN 9781493919925.
- ^ PMID 31367093.
- ^ (Subscription may be required or content may be available in libraries.)|Available online 27 October 2005
- PMID 24259958.
- S2CID 20024219.
- PMID 20510833. – via ScienceDirect(Subscription may be required or content may be available in libraries.)
- ^ Nikolaidis, Paul; Meranda, Joseph; Miller, Frank; Summers, Allison; Gabriel, Helena; Talamonti, Mark; Gore, Richard. "Puestow Procedure – an overview ScienceDirect Topics". www.sciencedirect.com. Saunders.
- PMID 23622135.
- PMID 34501532..
 Text was copied from this source, which is available under Creative Commons Attribution 4.0 International License
Text was copied from this source, which is available under Creative Commons Attribution 4.0 International License
Further reading
- Yan, M-X; Li, Y-Q (2006-04-01). "Gall stones and chronic pancreatitis: the black box in between". Postgraduate Medical Journal. 82 (966): 254–258. PMID 16597812.
- Lerch, Markus M.; Gorelick, Fred S. (2013). "Models of Acute and Chronic Pancreatitis". Gastroenterology. 144 (6): 1180–1193. PMID 23622127. Retrieved 2015-11-29.
- Beyer, Georg; S2CID 221114304. Retrieved 1 January 2021.
