Clinical psychology
| Part of a series on |
| Psychology |
|---|
Clinical psychology is an integration of human science, behavioral science, theory, and clinical knowledge for the purpose of understanding, preventing, and relieving psychologically-based distress or dysfunction and to promote subjective well-being and personal development.[1][2] Central to its practice are psychological assessment, clinical formulation, and psychotherapy, although clinical psychologists also engage in research, teaching, consultation, forensic testimony, and program development and administration.[3] In many countries, clinical psychology is a regulated mental health profession.
The field is generally considered to have begun in 1896 with the opening of the first psychological clinic at the University of Pennsylvania by Lightner Witmer. In the first half of the 20th century, clinical psychology was focused on psychological assessment, with little attention given to treatment. This changed after the 1940s when World War II resulted in the need for a large increase in the number of trained clinicians. Since that time, three main educational models have developed in the US—the PhD Clinical Science model (heavily focused on research),[4] the PhD science-practitioner model (integrating scientific research and practice), and the PsyD practitioner-scholar model (focusing on clinical theory and practice). In the UK and the Republic of Ireland, the Clinical Psychology Doctorate falls between the latter two of these models, whilst in much of mainland Europe, the training is at the master's level and predominantly psychotherapeutic. Clinical psychologists are expert in providing psychotherapy, and generally train within four primary theoretical orientations—psychodynamic, humanistic, cognitive behavioral therapy (CBT), and systems or family therapy.
Clinical psychology is different from
History
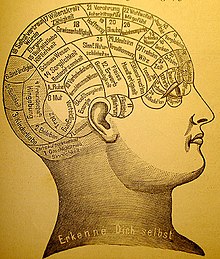
The earliest recorded approaches to assess and treat mental distress were a combination of religious, magical, and/or medical perspectives.
While the scientific community eventually came to reject all of these methods for treating mental illness, academic psychologists also were not concerned with serious forms of mental illness. The study of mental illness was already being done in the developing fields of psychiatry and neurology within the asylum movement.[6] It was not until the end of the 19th century, around the time when Sigmund Freud was first developing his "talking cure" in Vienna, that the first scientific application of clinical psychology began.
Early clinical psychology


By the second half of the 1800s, the scientific study of psychology was becoming well established in university laboratories. Although there were a few scattered voices calling for applied psychology, the general field looked down upon this idea and insisted on "pure" science as the only respectable practice.
Even as clinical psychology was growing, working with issues of serious mental distress remained the domain of psychiatrists and neurologists.[11] However, clinical psychologists continued to make inroads into this area due to their increasing skill at psychological assessment. Psychologists' reputation as assessment experts became solidified during World War I with the development of two intelligence tests, Army Alpha and Army Beta (testing verbal and nonverbal skills, respectively), which could be used with large groups of recruits.[7][8] Due in large part to the success of these tests, assessment was to become the core discipline of clinical psychology for the next quarter-century, when another war would propel the field into treatment.
Early professional organizations
The field began to organize under the name "clinical psychology" in 1917 with the founding of the American Association of Clinical Psychology. This only lasted until 1919, after which the American Psychological Association (founded by G. Stanley Hall in 1892) developed a section on Clinical Psychology, which offered certification until 1927.[10] Growth in the field was slow for the next few years when various unconnected psychological organizations came together as the American Association of Applied Psychology in 1930, which would act as the primary forum for psychologists until after World War II when the APA reorganized.[12] In 1945, the APA created what is now called Division 12, the Society for Clinical Psychology, which remains a leading organization in the field. Psychological societies and associations in other English-speaking countries developed similar divisions, including in Britain, Canada, Australia, and New Zealand.
World War II and the integration of treatment
When
WWII helped bring dramatic changes to clinical psychology, not just in America but internationally as well. Graduate education in psychology began adding psychotherapy to the science and research focus based on the 1947 scientist-practitioner model, known today as the Boulder Model, for PhD programs in clinical psychology.[14] Clinical psychology in Britain developed much like in the US after WWII, specifically within the context of the National Health Service[15] with qualifications, standards, and salaries managed by the British Psychological Society.[16]
Development of the Doctor of Psychology degree
By the 1960s, psychotherapy had become embedded within clinical psychology, but for many, the PhD educational model did not offer the necessary training for those interested in practice rather than research. There was a growing argument that said the field of psychology in the US had developed to a degree warranting explicit training in clinical practice. The concept of a practice-oriented degree was debated in 1965 and narrowly gained approval for a pilot program at the
A changing profession
Since the 1970s, clinical psychology has continued growing into a robust profession and academic field of study. Although the exact number of practicing clinical psychologists is unknown, it is estimated that between 1974 and 1990, the number in the US grew from 20,000 to 63,000.[19] Clinical psychologists continue to be experts in assessment and psychotherapy while expanding their focus to address issues of gerontology, sports, and the criminal justice system to name a few. One important field is health psychology, the fastest-growing employment setting for clinical psychologists in the past decade.[7] Other major changes include the impact of managed care on mental health care; an increasing realization of the importance of knowledge relating to multicultural and diverse populations; and emerging privileges to prescribe psychotropic medication.
Professional practice
| Occupation | |
|---|---|
| Names | Clinical psychologist |
Occupation type | Assessment and treatment of psychopathology |
Education required |
Or
|
Fields of employment | Hospitals, clinics |
Related jobs |
|
Clinical psychologists engage in a wide range of activities. Some focus solely on
In clinical practice, clinical psychologists may work with individuals, couples, families, or groups in a variety of settings, including private practices, hospitals, mental health organizations, schools, businesses, and non-profit agencies. Clinical psychologists who provide clinical services may also choose to specialize. Some specializations are codified and credentialed by regulatory agencies within the country of practice.[20] In the United States, such specializations are credentialed by the American Board of Professional Psychology (ABPP).
Training and certification to practice
Clinical psychologists study a generalist program in psychology plus postgraduate training and/or clinical placement and supervision. The length of training differs across the world, ranging from four years plus post-Bachelors supervised practice
In the UK, clinical psychologists undertake a Doctor of Clinical Psychology (DClinPsych), which is a practitioner
The practice of clinical psychology requires a license in the United States, Canada, the United Kingdom, and many other countries. Although each of the US states is somewhat different in terms of requirements and licenses, there are three common elements:[25]
- Graduation from an accredited school with the appropriate degree
- Completion of supervised clinical experience or internship
- Passing a written examination and, in some states, an oral examination
All U.S. state and Canadian province licensing boards are members of the Association of State and Provincial Psychology Boards (ASPPB), which created and maintains the Examination for Professional Practice in Psychology (EPPP). Many states require other examinations in addition to the EPPP, such as a jurisprudence (i.e. mental health law) examination and/or an oral examination.
In the UK, registration as a clinical psychologist with the Health Professions Council
Assessment
An important area of expertise for many clinical psychologists is psychological assessment, and there are indications that as many as 91% of psychologists engage in this core clinical practice.[27] Such evaluation is usually done in service to gaining insight into and forming hypothesis about psychological or behavioral problems. As such, the results of such assessments are usually used to create generalized impressions (rather than diagnosis) in service to informing treatment planning. Methods include formal testing measures, interviews, reviewing records, clinical observation, and physical examination.[2]
Measurement domains
There exist hundreds of various assessment tools, although only a few have been shown to have both high
Psychological measures generally fall within one of several categories, including the following:
- Intelligence & achievement tests – These tests are designed to measure certain specific kinds of cognitive functioning (often referred to as WRAML and the WIAT.
- Personality tests – NEO
- Neuropsychological tests – neurocognitivefunctioning, or when used in research, to contrast neuropsychological abilities across experimental groups.
- Diagnostic Measurement Tools – Clinical psychologists are able to diagnose psychological disorders and related disorders found in the for affective and Schizophrenia in children.
- Clinical observation – Clinical psychologists are also trained to gather data by observing behavior. The clinical interview is a vital part of the assessment, even when using other formalized tools, which can employ either a structured or unstructured format. Such assessment looks at certain areas, such as general appearance and behavior, mood and affects, perception, comprehension, orientation, insight, memory, and content of the communication. One psychiatric example of a formal interview is the mental status examination, which is often used in psychiatry as a screening tool for treatment or further testing.[27]
Diagnostic impressions
After assessment, clinical psychologists may provide a
Several new models are being discussed, including a "dimensional model" based on empirically validated models of human differences (such as the five factor model of personality[29][30]) and a "psychosocial model", which would take changing, intersubjective states into greater account.[31] The proponents of these models claim that they would offer greater diagnostic flexibility and clinical utility without depending on the medical concept of illness.[32] However, they also admit that these models are not yet robust enough to gain widespread use, and should continue to be developed.[32]
Clinical psychologists do not tend to diagnose, but rather use formulation—an individualized map of the difficulties that the patient or client faces, encompassing predisposing, precipitating and perpetuating (maintaining) factors.[33]
Clinical v. mechanical prediction
Clinical assessment can be characterized as a
What has come to be called the "clinical versus statistical prediction" debate was first described in detail in 1954 by
Intervention
Psychotherapy involves a formal relationship between professional and client—usually an individual, couple, family, or small group—that employs a set of procedures intended to form a therapeutic alliance, explore the nature of psychological problems, and encourage new ways of thinking, feeling, or behaving.[2][39]
Clinicians have a wide range of individual interventions to draw from, often guided by their training—for example, a cognitive behavioral therapy (CBT) clinician might use worksheets to record distressing cognitions, a psychoanalyst might encourage free association, while a psychologist trained in Gestalt techniques might focus on immediate interactions between client and therapist. Clinical psychologists generally seek to base their work on research evidence and outcome studies as well as on trained clinical judgment. Although there are literally dozens of recognized therapeutic orientations, their differences can often be categorized on two dimensions: insight vs. action and in-session vs. out-session.[9]
- Insight – emphasis is on gaining a greater understanding of the motivations underlying one's thoughts and feelings (e.g. psychodynamic therapy)
- Action – focus is on making changes in how one thinks and acts (e.g. solution focused therapy, cognitive behavioral therapy)
- In-session – interventions center on the here-and-now interaction between client and therapist (e.g. humanistic therapy, Gestalt therapy)
- Out-session – a large portion of therapeutic work is intended to happen outside of session (e.g. bibliotherapy, rational emotive behavior therapy)
The methods used are also different in regards to the population being served as well as the context and nature of the problem. Therapy will look very different between, say, a traumatized child, a depressed but high-functioning adult, a group of people recovering from substance dependence, and a ward of the state suffering from terrifying delusions. Other elements that play a critical role in the process of psychotherapy include the environment, culture, age, cognitive functioning, motivation, and duration (i.e. brief or long-term therapy).[39][40]
Four main schools
Many clinical psychologists are integrative or eclectic and draw from the evidence base across different models of therapy in an integrative way, rather than using a single specific model.
In the UK, clinical psychologists have to show competence in at least two models of therapy, including CBT, to gain their doctorate. The British Psychological Society Division of Clinical Psychology has been vocal about the need to follow the evidence base rather than being wedded to a single model of therapy.
In the US, intervention applications and research are dominated in training and practice by essentially four major schools of practice: psychodynamic, humanism, behavioral/cognitive behavioral, and systems or family therapy.[2]
Psychodynamic
The psychodynamic perspective developed out of the
Humanistic/Experiential
Humanistic psychology was developed in the 1950s in reaction to both behaviorism and psychoanalysis, largely due to the
Emotion focused therapy/Emotionally focused therapy (EFT), not to be confused with Emotional Freedom Techniques, was initially informed by humanistic–phenomenological and Gestalt theories of therapy.[45][46] "Emotion Focused Therapy can be defined as the practice of therapy informed by an understanding of the role of emotion in psychotherapeutic change. EFT is founded on a close and careful analysis of the meanings and contributions of emotion to human experience and change in psychotherapy. This focus leads therapist and client toward strategies that promotes the awareness, acceptance, expression, utilization, regulation, and transformation of emotion as well as corrective emotional experience with the therapist. The goals of EFT are strengthening the self, regulating affect, and creating new meaning".[45] Similarly to some Psychodynamic therapy approaches, EFT pulls heavily from attachment theory. Pioneers of EFT are Les Greenberg[47][48] and Sue Johnson.[49] EFT is often used in therapy with individuals, and may be especially useful for couples therapy.[50][51] Founded in 1998, Sue Johnson and others lead the International Centre for Excellence in Emotion Focused Therapy (ICEEFT) where clinicians can find EFT training internationally. EFT is also a commonly chosen modality to treat clinically diagnosable trauma.[52]
Behavioral and cognitive behavioral
Cognitive behavioral therapy (CBT) developed from the combination of cognitive therapy and rational emotive behavior therapy, both of which grew out of cognitive psychology and behaviorism. CBT is based on the theory that how we think (cognition), how we feel (emotion), and how we act (behavior) are related and interact together in complex ways. In this perspective, certain dysfunctional ways of interpreting and appraising the world (often through schemas or beliefs) can contribute to emotional distress or result in behavioral problems. The object of many cognitive behavioral therapies is to discover and identify the biased, dysfunctional ways of relating or reacting and through different methodologies help clients transcend these in ways that will lead to increased well-being.[53] There are many techniques used, such as systematic desensitization, socratic questioning, and keeping a cognition observation log. Modified approaches that fall into the category of CBT have also developed, including dialectic behavior therapy and mindfulness-based cognitive therapy.[54]
Behavior therapy is a rich tradition. It is well researched with a strong evidence base. Its roots are in
Systems or family therapy
Systems or family therapy works with couples and families, and emphasizes family relationships as an important factor in psychological health. The central focus tends to be on interpersonal dynamics, especially in terms of how change in one person will affect the entire system.[56] Therapy is therefore conducted with as many significant members of the "system" as possible. Goals can include improving communication, establishing healthy roles, creating alternative narratives, and addressing problematic behaviors.
Other therapeutic perspectives
There exist dozens of recognized schools or orientations of psychotherapy—the list below represents a few influential orientations not given above. Although they all have some typical set of techniques practitioners employ, they are generally better known for providing a framework of theory and philosophy that guides a therapist in his or her working with a client.
- Existential – Existential psychotherapy postulates that people are largely free to choose who we are and how we interpret and interact with the world. It intends to help the client find deeper meaning in life and to accept responsibility for living. As such, it addresses fundamental issues of life, such as death, aloneness, and freedom. The therapist emphasizes the client's ability to be self-aware, freely make choices in the present, establish personal identity and social relationships, create meaning, and cope with the natural anxiety of living.[57]
- Gestalt – Gestalt therapy was primarily founded by Fritz Perls in the 1950s. This therapy is perhaps best known for using techniques designed to increase self-awareness, the best-known perhaps being the "empty chair technique." Such techniques are intended to explore resistance to "authentic contact", resolve internal conflicts, and help the client complete "unfinished business".[58]
- Postmodern – Postmodern psychology says that the experience of reality is a subjective construction built upon language, social context, and history, with no essential truths.[59] Since "mental illness" and "mental health" are not recognized as objective, definable realities, the postmodern psychologist instead sees the goal of therapy strictly as something constructed by the client and therapist.[60] Forms of postmodern psychotherapy include narrative therapy, solution-focused therapy, and coherence therapy.
- Transpersonal – The transpersonal perspective places a stronger focus on the spiritual facet of human experience.[61] It is not a set of techniques so much as a willingness to help a client explore spirituality and/or transcendent states of consciousness. Transpersonal psychology is concerned with helping clients achieve their highest potential.
- Multiculturalism – Although the theoretical foundations of psychology are rooted in European culture, there is a growing recognition that there exist profound differences between various ethnic and social groups and that systems of psychotherapy need to take those differences into greater consideration.[40] Further, the generations following immigrant migration will have some combination of two or more cultures—with aspects coming from the parents and from the surrounding society—and this process of acculturation can play a strong role in therapy (and might itself be the presenting problem). Culture influences ideas about change, help-seeking, locus of control, authority, and the importance of the individual versus the group, all of which can potentially clash with certain givens in mainstream psychotherapeutic theory and practice.[62] As such, there is a growing movement to integrate knowledge of various cultural groups in order to inform therapeutic practice in a more culturally sensitive and effective way.[63]
- Feminism – Feminist therapy is an orientation arising from the disparity between the origin of most psychological theories (which have male authors) and the majority of people seeking counseling being female. It focuses on societal, cultural, and political causes and solutions to issues faced in the counseling process. It openly encourages the client to participate in the world in a more social and political way.[64]
- Positive psychology – mental illness rather than mental wellness. Applied positive psychology's main focus, therefore, is to increase one's positive experience of life and ability to flourish by promoting such things as optimism about the future, a sense of flow in the present, and personal traits like courage, perseverance, and altruism.[66][67] There is now preliminary empirical evidence to show that by promoting Seligman's three components of happiness—positive emotion (the pleasant life), engagement (the engaged life), and meaning (the meaningful life)—positive therapy can decrease clinical depression.[68]
Community psychology approaches are often used for psychological prevention of harm and clinical intervention.[69][70][71]
Integration
In the last couple of decades, there has been a growing movement to integrate the various therapeutic approaches, especially with an increased understanding of cultural, gender, spiritual, and sexual-orientation issues. Clinical psychologists are beginning to look at the various strengths and weaknesses of each orientation while also working with related fields, such as neuroscience, behavioural genetics, evolutionary biology, and psychopharmacology. The result is a growing practice of eclecticism, with psychologists learning various systems and the most efficacious methods of therapy with the intent to provide the best solution for any given problem.[72]
Professional ethics
The examples and perspective in this article deal primarily with the United States and do not represent a worldwide view of the subject. (February 2016) |
The field of clinical psychology in most countries is strongly regulated by a code of ethics. In the US, professional ethics are largely defined by the APA Code of Conduct, which is often used by states to define licensing requirements. The APA Code generally sets a higher standard than that which is required by law as it is designed to guide responsible behavior, the protection of clients, and the improvement of individuals, organizations, and society.[73] The Code is applicable to all psychologists in both research and applied fields.
The APA Code is based on five principles: Beneficence and Nonmaleficence, Fidelity and Responsibility, Integrity, Justice, and Respect for People's Rights and Dignity.[73] Detailed elements address how to resolve ethical issues, competence, human relations, privacy and confidentiality, advertising, record keeping, fees, training, research, publication, assessment, and therapy.
The Canadian Psychological Association ethical code principle's are: Respect for the Dignity of Persons and Peoples, Responsible Caring, Integrity in Relationships, and Responsibility to Society. It is considered very similar to the APA's Code.[74]
In the UK the British Psychological Society has published a Code of Conduct and Ethics for clinical psychologists. This has four key areas: Respect, Competence, Responsibility and Integrity.[75] Other European professional organizations have similar codes of conduct and ethics.
The Asian Federation for Psychotherapy published a code of ethics in 2008 with the following principles: Beneficence, Responsibility, Integrity, Justices, and Respect. Similar to the APA code, it provides detailed instructions for the conduct of psychologists, specifically psychotherapists.[76] Russia, India, Iran, Kazakhstan, China, Malaysia, and Japan are member countries.[77]
The National Latina/o Psychological Association adopted their current ethical guidelines in 2018, stating that "the traditional Eurocentric foundations in mainstream psychology have provided culturally bound knowledge about worldviews, ways of living, and cultural practices." Their principles are: Respect and Responsibility, Ethical Dilemmas, Ethical Decision-Making and Legal Responsibility, Consultation, Justice and Advocacy, Self-Awareness and Social-Consciousness, Action and Accountability, Training and Creating Infrastructure, and Mentorship.[78]
Comparison with other mental health professions
Psychiatry
Although clinical psychologists and
scanning. Conversely, clinical psychologists conduct specialist assessment and psychometric testing. Such assessments and tests would not normally only be administered and interpreted by psychologists due to their advanced training in psychometric assessment. As standard clinical psychologists also usually possess more advanced training and specialist knowledge in psycho-social development and psychological therapies.Clinical psychologists generally do not prescribe medication, although there is a movement for psychologists to have prescribing privileges.[80] These medical privileges require additional training and education. To date, medical psychologists (prescribing psychologists) may prescribe psychotropic medications in Colorado, Guam, Iowa, Idaho, Illinois, New Mexico, Louisiana, the Public Health Service, the Indian Health Service, and the United States Military.[81]
Counseling psychology
Counseling psychologists undergo the same level of rigor in study and use many of the same interventions and tools as clinical psychologists, including psychotherapy and assessment. Traditionally, counseling psychologists helped people with what might be considered normal or moderate psychological problems—such as the feelings of anxiety or sadness resulting from major life changes or events.[3][9] However, that distinction has faded over time, and of the counseling psychologists who do not go into academia (which does not involve treatment or diagnosis), the majority of counseling psychologists treat mental illness alongside clinical psychologists. Many counseling psychologists also receive specialized training in career assessment, group therapy, and relationship counseling.
Counseling psychology as a field values multiculturalism[82] and social advocacy, often stimulating research in multicultural issues. There are fewer counseling psychology graduate programs than those for clinical psychology and they are more often housed in departments of education rather than psychology. Counseling psychologists tend to be more frequently employed in university counseling centers compared to hospitals and private practice for clinical psychologists.[83] However, counseling and clinical psychologists can be employed in a variety of settings, with a large degree of overlap (prisons, colleges, community mental health, non-profits, corporations, private practice, hospitals and Veterans Affairs).
| Comparison of mental health professionals in the US | ||||
| Occupation | Degree | Common licenses | Prescription privilege | Mean 2022 income (USD) |
| Clinical psychologist | PhD/PsyD/EdD | Psychologist | Varies by state | $90,130 |
| Counseling psychologist (doctorate) | PhD/PsyD/EdD | Psychologist | No | $65,000 |
| Counselor (master's) | MA/MS/MEd | MFT/LPC/LHMC/LPA | No | $49,710 |
| School psychologist | PhD/EdD/MS/EdS | School psychologist | No | $81,500 |
| Psychiatrist | MD/DO | Psychiatrist | Yes | $226,880 |
| Clinical social worker | PhD/DSW/MSW | LCSW | No | $55,350 |
Psychiatric nurse
|
MSN/BSN | RN | No | $75,330 |
Psychiatric and mental health nurse practitioner
|
DNP/PhD/MSN | APRN/APN/PMHNP | Yes (varies by state) | $121,610 |
Expressive/Art therapist
|
MA | ATR | No | $55,900 |
School psychology
Traditional job roles for school psychologists employed in school settings have focused mainly on assessment of students to determine their eligibility for special education services in schools, and on consultation with teachers and other school professionals to design and carry out interventions on behalf of students. Other major roles also include offering individual and group therapy with children and their families, designing prevention programs (e.g. for reducing dropout), evaluating school programs, and working with teachers and administrators to help maximize teaching efficacy, both in the classroom and systemically.[90][91]
Clinical social work
Social workers provide a variety of services, generally concerned with social problems, their causes, and their solutions. With specific training, clinical social workers may also provide psychological counseling (in the US and Canada), in addition to more traditional social work.
Occupational therapy
Criticisms and controversies
Clinical psychology is a diverse field and there have been recurring tensions over the degree to which clinical practice should be limited to treatments supported by empirical research.[93] Despite some evidence showing that all the major therapeutic orientations are about of equal effectiveness,[94][95] there remains much debate about the efficacy of various forms of treatment in use in clinical psychology.[96]
See also
References
- ^ "About Clinical Psychology". American Psychological Association. American Psychological Association, Division 12. 1996. Archived from the original on 2015-04-01. Retrieved July 5, 2019.
- ^ ISBN 0-471-47276-X
- ^ ISBN 0-17-490058-9
- PMID 17716063.
- ^ "Getting Help".
- ^ ISBN 978-1-4051-3206-0.
- ^ PMID 17716080.
- ^ ISBN 0-306-44877-7
- ^ ISBN 0-07-012491-4
- ^ a b Evans Rand (1999). "Clinical psychology born and raised in controversy". APA Monitor. 30 (11).
- ISBN 978-0-306-44452-4.
- ^ American Psychological Association (1999). "APA: Uniting psychologists for more than 100 years". APA Monitor Online. Vol. 30, no. 11. Archived from the original on October 21, 2000.
- ISBN 978-1-56032-188-0.
- PMID 10717971.
- ISBN 978-0-19-856689-2.
- doi:10.1037/h0038711.
- ^ a b Murray, Bridget (2000). "The degree that almost wasn't: The PsyD comes of age". Monitor on Psychology. Vol. 31, no. 1. Archived from the original on October 8, 2010.
- ^ a b c Norcross, J. & Castle, P. (2002). "Appreciating the Psy.D: The Facts". Eye on Psi Chi. Vol. 7, no. 1. pp. 22–26. Archived from the original on 2006-09-27.
- ISBN 978-0-88048-866-2.
- ^ American Board of Professional Psychology, Specialty Certification in Professional Psychology Archived 2006-12-14 at the Wayback Machine
- ^ Pathways to register as a psychologist including clinical psychologist in Australia Archived August 19, 2008, at the Wayback Machine
- ^ "Society of Clinical Psychology". apa.org. Archived from the original on 2015-04-01.
- ^ APA. (2005). Guidelines and Principles for Accreditation of Programs in Professional Psychology: Quick Reference Guide to Doctoral Programs.
- ISBN 0-7619-4768-X
- ^ a b "Association of State and Provincial Psychology Boards". Archived from the original on 2011-02-22. Retrieved 2007-02-17.
- ^ "Professional Disciplines". Archived from the original on 2008-12-08. Retrieved 2008-12-01.
- ^ ISBN 0-471-41979-6
- ^ "Qualifications Policy".
- ^ S2CID 21164280.
- S2CID 137142. Archived from the original(PDF) on 2020-12-09.
- S2CID 34777977.
- ^ OCLC 43114994.
- S2CID 16787375.
- ^ ISSN 1076-8971.
- ^ ISBN 978-0-9638784-9-6.
- S2CID 11956010. Archived from the original(PDF) on 2019-03-03.
- S2CID 145150890.
- ISSN 1939-1323.
- ^ ISBN 1-58562-185-4
- ^ .
- ISBN 978-0-7619-4868-1.
- ISBN 978-0-415-23633-1.
- ^ Gessmann, Hans-Werner (2013;2), Humanistische Psychologie und Humanistisches Psychodrama. In: Humanistisches Psychodama Band 4, Verlag des PIB Duisburg, pp. 27–84.
- ISBN 978-0-7619-2121-9.
- ^ ISBN 978-1-4338-2631-3.
- ^ Perls, F., Hefferline, G., & Goodman, P. (1951). Gestalt therapy. New York, 64(7), 19-313.
- ^ Greenberg, L. S. (2004). Emotion–focused therapy. Clinical Psychology & Psychotherapy: An International Journal of Theory & Practice, 11(1), 3–16.
- ^ Greenberg, L. S. (2010). Emotion-focused therapy: A clinical synthesis. Focus, 8(1), 32–42.
- ^ Johnson, S. M. (2019). Attachment theory in practice: Emotionally focused therapy (EFT) with individuals, couples, and families. Guilford Publications.
- ^ Greenman, P. S., & Johnson, S. M. (2013). Process research on emotionally focused therapy (EFT) for couples: Linking theory to practice. Family Process, 52(1), 46–61.
- ^ Greenberg, L. S., & Goldman, R. N. (2008). Emotion-focused couples therapy: The dynamics of emotion, love, and power. American Psychological Association.
- ^ Paivio, S. C., & Pascual-Leone, A. (2010). Emotion-focused therapy for complex trauma: An integrative approach. American Psychological Association.
- ISBN 978-1-59385-476-8.
- ^ Association for Behavioral and Cognitive Therapies (2006). "What is CBT?". Retrieved 2007-03-04.
Albert Ellis is often referred as the "grandfather" of CBT for his influential work in this field.
- doi:10.1037/h0100155.
- ISBN 9780534348236.
- ISBN 0-7619-6223-9
- ISBN 0-7619-2791-3
- ISBN 0-7619-2080-3
- ^ Blatner Adam (1997). "The Implications of Postmodernism for Psychotherapy". Individual Psychology. 53 (4): 476–482.
- ISBN 0-7914-2835-4
- ISBN 978-0-13-111753-2.
- ^ Price, Michael (2008). "Culture matters: Accounting for clients' backgrounds and values makes for better treatment". Monitor on Psychology. Vol. 39, no. 7. pp. 52–53.
- ISBN 978-0-7890-0201-3.
- PMID 11392865.
- ISBN 978-0-19-513533-6.
- S2CID 18678209. Archived from the original(PDF) on 2016-09-10. Retrieved 2016-08-16.
- S2CID 10840428. Archived from the original(PDF) on 2020-02-25.
- ^ Graham-Bermann, S. A., Lynch, S., Banyard, V., DeVoe, E. R., & Halabu, H. (2007). Community-based intervention for children exposed to intimate partner violence: An efficacy trial. Journal of consulting and clinical psychology, 75(2), 199.
- ^ Breitenstein, S. M., Gross, D., Garvey, C. A., Hill, C., Fogg, L., & Resnick, B. (2010). Implementation fidelity in community‐based interventions. Research in nursing & health, 33(2), 164–173.
- ^ Grant, K. E., Tandon, D., Lambert, S., Farahmand, F. K., Ross, K., Odahl-Ruan, C., & Tolan, P. (2017). Community psychology approaches to intervention with children and adolescents. In M. A. Bond, I. Serrano-García, C. B. Keys, & M. Shinn (Eds.), APA handbooks in psychology®. APA handbook of community psychology: Methods for community research and action for diverse groups and issues (p. 587–603). American Psychological Association. https://doi.org/10.1037/14954-035
- .
- ^ a b APA. (2003). Ethical Principles of Psychologists and Code of Conduct. Retrieved July 28, 2007.
- – via Taylor & Francis Online.
- ^ "Code of Ethics and Conduct" (PDF). beta.bps.org.uk. August 2009. Archived from the original (PDF) on 2017-02-27. Retrieved 2019-07-23.
- ^ "Code of Ethics". ASIAN FEDERATION FOR PSYCHOTHERAPY. October 2008. Retrieved December 5, 2023.
- ^ "Member Countries - Russia". ASIAN FEDERATION FOR PSYCHOTHERAPY. Retrieved December 5, 2023.
- ^ Rodríguez, Melanie M. Domenech; Gallardo, Miguel E; Field, Lynda; Rosario, Cristalís Capielo; Delgado-Romero, Ed (January 1, 2018). "Ethical Guidelines" (PDF). National Latina/o Psychological Association. Retrieved December 5, 2023.
- PMID 15895765.
- .
- ^ Halloway, Jennifer (2004). "Gaining prescriptive knowledge". Monitor on Psychology. Vol. 35, no. 6. p. 22.
- ^ "What is Counseling Psychology – Society of Counseling Psychology, Division 17". div17.org.
- doi:10.24839/1092-0803.Eye5.1.20. Archived from the originalon 2003-04-15.
- ^ APA (2003). "Salaries in Psychology 2003: Report of the 2003 APA Salary Survey".
- ^ NIH: Office of Science Education (2006). "Lifeworks: Psychiatrist".
- ^ U.S. Department of Labor: Bureau of Labor Statistics (2004). "Occupational Outlook Handbook: Social Workers".
- ^ U.S. Department of Labor: Bureau of Labor Statistics (2004). "Occupational Outlook Handbook: Registered Nurses".
- ^ NIH: Office of Science Education (2006). "Advance News Magazines. (2005)" (PDF).
- ^ "Lifeworks: Art Therapist". Retrieved 2007-02-17.
- ^ Silva, Arlene (2003). "Who Are School Psychologists?". National Association of School Psychologists.
- ^ American Psychological Association. "Archival Description of School Psychology". American Psychological Association.
- ^ "Occupational Therapy". The American Heritage Dictionary of the English Language: Fourth Edition. 2000. Archived from the original on 2008-12-08.
- ISBN 978-0-415-04632-9.
- S2CID 39770553. Archived from the original(PDF) on 2020-12-09.
- S2CID 142840311.
- ISBN 978-1462517510.
External links
- American Academy of Clinical Psychology
- American Association for Marriage and Family Therapy Archived 2019-05-30 at the Wayback Machine
- American Board of Professional Psychology
- Annual Review of Clinical Psychology Archived 2009-01-20 at the Wayback Machine
- APA Society of Clinical Psychology (Division 12)
- Association of State and Provincial Psychology Boards (ASPPB) Archived 2017-10-09 at the Wayback Machine
- NAMI: National Alliance on Mental Illness
- National Institute of Mental Health

