Collagen

Collagen (/ˈkɒlədʒən/) is the main structural protein in the extracellular matrix found in the body's various connective tissues. As the main component of connective tissue, it is the most abundant protein in mammals,[1] making up from 25% to 35% of the whole-body protein content. Collagen consists of amino acids bound together to form a triple helix of elongated fibril[2] known as a collagen helix. It is mostly found in connective tissue such as cartilage, bones, tendons, ligaments, and skin. Vitamin C is vital for collagen synthesis, and Vitamin E improves the production of collagen.
Depending upon the degree of
Etymology

The name collagen comes from the Greek
Human types
Over 90% of the collagen in the human body is type I collagen.[8] However, as of 2011, 28 types of human collagen have been identified, described, and divided into several groups according to the structure they form.[9] All of the types contain at least one triple helix.[9] The number of types shows collagen's diverse functionality.[10]
- Fibrillar (Type I, II, III, V, XI)
- Non-fibrillar
- FACIT (Fibril Associated Collagens with Interrupted Triple Helices) (Type IX, XII, XIV, XIX, XXI)
- Short chain (Type VIII, X)
- Basement membrane (Type IV)
- Multiplexin (Multiple Triple Helix domains with Interruptions) (Type XV, XVIII)
- MACIT (Membrane Associated Collagens with Interrupted Triple Helices) (Type XIII, XVII)
- Microfibril forming (Type VI)
- Anchoring fibrils (Type VII)
The five most common types are:[11]
- Type I: skin, tendon, vasculature, organs, bone (main component of the organic part of bone)
- Type II: cartilage (main collagenous component of cartilage)
- Type III: reticulate (main component of reticular fibers), commonly found alongside type I
- Type IV: forms basal lamina, the epithelium-secreted layer of the basement membrane
- Type V: cell surfaces, hair, and placenta
In human biology
Cardiac
The collagenous
Bone grafts
As the skeleton forms the structure of the body, it is vital that it maintains its strength, even after breaks and injuries. Collagen is used in bone grafting as it has a triple helical structure, making it a very strong molecule. It is ideal for use in bones, as it does not compromise the structural integrity of the skeleton. The triple helical structure of collagen prevents it from being broken down by enzymes, it enables adhesiveness of cells and it is important for the proper assembly of the extracellular matrix.[12]
Tissue regeneration
Collagen scaffolds are used in tissue regeneration, whether in sponges,
Reconstructive surgical uses
Collagens are widely employed in the construction of
Wound healing
This section needs additional citations for verification. (April 2021) |
Collagen is one of the body's key natural resources and a component of skin tissue that can benefit all stages of wound healing.[21] When collagen is made available to the wound bed, closure can occur. Wound deterioration, followed sometimes by procedures such as amputation, can thus be avoided.
Collagen is a natural product and is thus used as a natural wound dressing and has properties that artificial wound dressings do not have. It is resistant against bacteria, which is of vital importance in a wound dressing. It helps to keep the wound sterile, because of its natural ability to fight infection. When collagen is used as a burn dressing, healthy granulation tissue is able to form very quickly over the burn, helping it to heal rapidly.[22]
Throughout the four phases of wound healing, collagen performs the following functions:
- Guiding function: Collagen fibersserve to guide fibroblasts. Fibroblasts migrate along a connective tissue matrix.
- Chemotacticproperties: The large surface area available on collagen fibers can attract fibrogenic cells which help in healing.
- Nucleation: Collagen, in the presence of certain neutral salt molecules, can act as a nucleating agent causing formation of fibrillar structures.
- Hemostatic properties: Blood plateletsinteract with the collagen to make a hemostatic plug.
Basic research
Collagen is used in laboratory studies for cell culture, studying cell behavior and cellular interactions with the extracellular environment.[23] Collagen is also widely used as a bioink for 3D bioprinting and biofabrication of 3D tissue models.
Biology
The collagen protein is composed of a triple helix, which generally consists of two identical chains (α1) and an additional chain that differs slightly in its chemical composition (α2).[24] The amino acid composition of collagen is atypical for proteins, particularly with respect to its high hydroxyproline content. The most common motifs in the amino acid sequence of collagen are glycine-proline-X and glycine-X-hydroxyproline, where X is any amino acid other than glycine, proline or hydroxyproline. The average amino acid composition for fish and mammal skin is given.[25]
| Amino acid | Abundance in mammal skin ( residues /1000) |
Abundance in fish skin (residues/1000) |
|---|---|---|
| Glycine | 329 | 339 |
| Proline | 126 | 108 |
| Alanine | 109 | 114 |
| Hydroxyproline | 95 | 67 |
| Glutamic acid | 74 | 76 |
| Arginine | 49 | 52 |
| Aspartic acid | 47 | 47 |
| Serine | 36 | 46 |
| Lysine | 29 | 26 |
| Leucine | 24 | 23 |
| Valine | 22 | 21 |
| Threonine | 19 | 26 |
| Phenylalanine | 13 | 14 |
| Isoleucine | 11 | 11 |
| Hydroxylysine | 6 | 8 |
| Methionine | 6 | 13 |
| Histidine | 5 | 7 |
| Tyrosine | 3 | 3 |
| Cysteine | 1 | 1 |
| Tryptophan | 0 | 0 |
Synthesis
This section needs additional citations for verification. (April 2021) |
First, a three-dimensional stranded structure is assembled, with the amino acids glycine and proline as its principal components. This is not yet collagen but its precursor, procollagen. Procollagen is then modified by the addition of
- Transcription of mRNA: About 44 genes are associated with collagen formation, each coding for a specific mRNA sequence, and typically have the "COL" prefix. The beginning of collagen synthesis begins with turning on genes which are associated with the formation of a particular alpha peptide (typically alpha 1, 2 or 3).
- Pre-pro-peptide formation: Once the final mRNA exits from the cell nucleus and enters into the cytoplasm, it links with the ribosomal subunits and the process of translation occurs. The early/first part of the new peptide is known as the signal sequence. The signal sequence on the N-terminal of the peptide is recognized by a signal recognition particle on the endoplasmic reticulum, which will be responsible for directing the pre-pro-peptideinto the endoplasmic reticulum. Therefore, once the synthesis of new peptide is finished, it goes directly into the endoplasmic reticulum for post-translational processing. It is now known as preprocollagen.
- Pre-pro-peptide to pro-collagen: Three modifications of the pre-pro-peptide occur leading to the formation of the alpha peptide:
- The signal peptide on the N-terminal is removed, and the molecule is now known as propeptide (not procollagen).
- Hydroxylation of lysines and prolines on propeptide by the enzymes 'prolyl hydroxylase' and 'lysyl hydroxylase' (to produce hydroxyproline and hydroxylysine) occurs to aid cross-linking of the alpha peptides. This enzymatic step requires vitamin C as a cofactor. In scurvy, the lack of hydroxylation of prolines and lysines causes a looser triple helix (which is formed by three alpha peptides).
- Glycosylation occurs by adding either glucose or galactose monomers onto the hydroxyl groups that were placed onto lysines, but not on prolines.
- Once these modifications have taken place, three of the hydroxylated and glycosylated propeptides twist into a triple helix forming procollagen. Procollagen still has unwound ends, which will be later trimmed. At this point, the procollagen is packaged into a transfer vesicle destined for the Golgi apparatus.
- Golgi apparatus modification: In the Golgi apparatus, the procollagen goes through one last post-translational modification before being secreted out of the cell. In this step, oligosaccharides (not monosaccharides as in step 3) are added, and then the procollagen is packaged into a secretory vesicle destined for the extracellular space.
- Formation of tropocollagen: Once outside the cell, membrane bound enzymes known as collagen peptidases, remove the "loose ends" of the procollagen molecule. What is left is known as tropocollagen. Defects in this step produce one of the many collagenopathies known as Ehlers–Danlos syndrome. This step is absent when synthesizing type III, a type of fibrillar collagen.
- Formation of the collagen fibril: copper-dependentenzyme, produces the final step in the collagen synthesis pathway. This enzyme acts on lysines and hydroxylysines producing aldehyde groups, which will eventually undergo covalent bonding between tropocollagen molecules. This polymer of tropocollagen is known as a collagen fibril.

Amino acids
Collagen has an unusual amino acid composition and sequence:
- residue.
- Proline makes up about 17% of collagen.
- Collagen contains two unusual derivative amino acids not directly inserted during translation. These amino acids are found at specific locations relative to glycine and are modified post-translationally by different enzymes, both of which require vitamin C as a cofactor.
- Hydroxyproline derived from proline
- Hydroxylysine derived from lysine – depending on the type of collagen, varying numbers of hydroxylysines are glycosylated (mostly having disaccharides attached).
Collagen I formation
Most collagen forms in a similar manner, but the following process is typical for type I:
- Inside the cell
- Two types of alpha chains – alpha-1 and alpha 2, are formed during rough endoplasmic reticulum (RER). These peptide chains known as preprocollagen, have registration peptides on each end and a signal peptide.[30]
- Polypeptide chains are released into the lumen of the RER.
- Signal peptides are cleaved inside the RER and the chains are now known as pro-alpha chains.
- ascorbic acid (vitamin C) as a cofactor.
- Glycosylation of specific hydroxylysine residues occurs.
- Triple alpha helical structure is formed inside the endoplasmic reticulum from two alpha-1 chains and one alpha-2 chain.
- Procollagen is shipped to the Golgi apparatus, where it is packaged and secreted into extracellular space by exocytosis.
- Two types of alpha chains – alpha-1 and alpha 2, are formed during
- Outside the cell
- Registration peptides are cleaved and tropocollagen is formed by procollagen peptidase.
- Multiple tropocollagen molecules form collagen fibrils, via covalent cross-linking (aldol reaction) by lysyl oxidase which links hydroxylysine and lysine residues. Multiple collagen fibrils form into collagen fibers.
- Collagen may be attached to cell membranes via several types of protein, including fibronectin, laminin, fibulin and integrin.
Synthetic pathogenesis
Vitamin C deficiency causes
An autoimmune disease such as lupus erythematosus or rheumatoid arthritis[31] may attack healthy collagen fibers.
Many bacteria and viruses secrete virulence factors, such as the enzyme collagenase, which destroys collagen or interferes with its production.
Molecular structure
This section needs additional citations for verification. (April 2021) |
A single collagen molecule, tropocollagen, is used to make up larger collagen aggregates, such as fibrils. It is approximately 300
A distinctive feature of collagen is the regular arrangement of amino acids in each of the three chains of these collagen subunits. The sequence often follows the pattern Gly-Pro-X or Gly-X-Hyp, where X may be any of various other amino acid residues.[25] Proline or hydroxyproline constitute about 1/6 of the total sequence. With glycine accounting for the 1/3 of the sequence, this means approximately half of the collagen sequence is not glycine, proline or hydroxyproline, a fact often missed due to the distraction of the unusual GX1X2 character of collagen alpha-peptides. The high glycine content of collagen is important with respect to stabilization of the collagen helix as this allows the very close association of the collagen fibers within the molecule, facilitating hydrogen bonding and the formation of intermolecular cross-links.[25] This kind of regular repetition and high glycine content is found in only a few other fibrous proteins, such as silk fibroin.
Collagen is not only a structural protein. Due to its key role in the determination of cell phenotype, cell adhesion, tissue regulation, and infrastructure, many sections of its non-proline-rich regions have cell or matrix association/regulation roles. The relatively high content of proline and hydroxyproline rings, with their geometrically constrained
Because glycine is the smallest amino acid with no side chain, it plays a unique role in fibrous structural proteins. In collagen, Gly is required at every third position because the assembly of the triple helix puts this residue at the interior (axis) of the helix, where there is no space for a larger side group than glycine's single
The tropocollagen
There is some
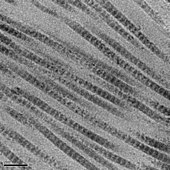
Collagen fibrils/aggregates are arranged in different combinations and concentrations in various tissues to provide varying tissue properties. In bone, entire collagen triple helices lie in a parallel, staggered array. 40 nm gaps between the ends of the tropocollagen subunits (approximately equal to the gap region) probably serve as nucleation sites for the deposition of long, hard, fine crystals of the mineral component, which is hydroxylapatite (approximately) Ca10(OH)2(PO4)6.
Associated disorders
Collagen-related diseases most commonly arise from genetic defects or nutritional deficiencies that affect the biosynthesis, assembly, posttranslational modification, secretion, or other processes involved in normal collagen production.
| Type | Notes | Gene(s) | Disorders |
I |
This is the most abundant collagen of the human body. It is present in scar tissue, the end product when tissue heals by repair. It is found in tendons, skin, artery walls, cornea, the endomysium surrounding muscle fibers, fibrocartilage, and the organic part of bones and teeth. | COL1A2 |
Osteogenesis imperfecta, Ehlers–Danlos syndrome, infantile cortical hyperostosis a.k.a. Caffey's disease |
II |
Vitreous humour of the eye. |
COL2A1 |
Collagenopathy, types II and XI |
III |
This is the collagen of granulation tissue and is produced quickly by young fibroblasts before the tougher type I collagen is synthesized. Reticular fiber. Also found in artery walls, skin, intestines and the uterus | COL3A1 |
Ehlers–Danlos syndrome, Dupuytren's contracture |
IV |
. | COL4A6 |
Goodpasture's syndrome
|
| V | Most interstitial tissue, assoc. with type I, associated with placenta | COL5A3 |
Ehlers–Danlos syndrome (classical) |
| VI | Most interstitial tissue, assoc. with type I | COL6A5 |
|
| VII | Forms anchoring fibrils in dermoepidermal junctions |
COL7A1 |
Epidermolysis bullosa dystrophica |
| VIII | Some endothelial cells | COL8A2 |
Posterior polymorphous corneal dystrophy 2
|
| IX | FACIT collagen, cartilage, assoc. with type II and XI fibrils | COL9A3 |
EDM3
|
| X | mineralizing cartilage |
COL10A1 |
Schmid metaphyseal dysplasia
|
| XI | Cartilage | COL11A2 |
Collagenopathy, types II and XI |
| XII | FACIT collagen, interacts with type I containing fibrils, decorin and glycosaminoglycans | COL12A1 |
– |
| XIII | Transmembrane collagen, interacts with integrin a1b1, fibronectin and components of basement membranes like nidogen and perlecan. | COL13A1 |
– |
| XIV | FACIT collagen, also known as undulin | COL14A1 |
– |
| XV | – | COL15A1 |
– |
| XVI | FACIT collagen | COL16A1 |
– |
XVII |
Transmembrane collagen, also known as BP180, a 180 kDa protein | COL17A1 |
Bullous pemphigoid and certain forms of junctional epidermolysis bullosa |
| XVIII | Source of endostatin | COL18A1 |
– |
| XIX | FACIT collagen | COL19A1 |
– |
| XX | – | COL20A1 |
– |
| XXI | FACIT collagen | COL21A1 |
– |
| XXII | FACIT collagen | COL22A1 |
– |
| XXIII | MACIT collagen | COL23A1 |
– |
| XXIV | – | COL24A1 | – |
| XXV | – | COL25A1 |
– |
| XXVI | – | EMID2 | – |
| XXVII | – | COL27A1 |
– |
| XXVIII | – | COL28A1 |
– |
| XXIX | Epidermal collagen | COL29A1 |
Atopic dermatitis[43] |
In addition to the above-mentioned disorders, excessive deposition of collagen occurs in scleroderma.
Diseases
One thousand mutations have been identified in 12 out of more than 20 types of collagen. These mutations can lead to various diseases at the tissue level.[44]
Osteogenesis imperfecta – Caused by a mutation in type 1 collagen, dominant autosomal disorder, results in weak bones and irregular connective tissue, some cases can be mild while others can be lethal. Mild cases have lowered levels of collagen type 1 while severe cases have structural defects in collagen.[45]
Ehlers–Danlos syndrome – Thirteen different types of this disorder, which lead to deformities in connective tissue, are known.[47] Some of the rarer types can be lethal, leading to the rupture of arteries. Each syndrome is caused by a different mutation. For example, the vascular type (vEDS) of this disorder is caused by a mutation in collagen type 3.[48]
Alport syndrome – Can be passed on genetically, usually as X-linked dominant, but also as both an autosomal dominant and autosomal recessive disorder, those with the condition have problems with their kidneys and eyes, loss of hearing can also develop during the childhood or adolescent years.[49]
Characteristics
Collagen is one of the long,
Uses

Collagen has a wide variety of applications, from food to medical.
If collagen is subject to sufficient denaturation, such as by heating, the three tropocollagen strands separate partially or completely into globular domains, containing a different secondary structure to the normal collagen polyproline II (PPII) of random coils. This process describes the formation of gelatin, which is used in many foods, including flavored gelatin desserts. Besides food, gelatin has been used in pharmaceutical, cosmetic, and photography industries. It is also used as a dietary supplement, and has been advertised as a potential remedy against the ageing process.[55][56][57]
From the Greek for glue, kolla, the word collagen means "
Gelatin-resorcinol-formaldehyde glue (and with formaldehyde replaced by less-toxic pentanedial and ethanedial) has been used to repair experimental incisions in rabbit lungs.[59]
Cosmetics
This section needs more primary sources. (March 2023) |  |
History
The molecular and packing structures of collagen eluded scientists over decades of research. The first evidence that it possesses a regular structure at the molecular level was presented in the mid-1930s.
The packing structure of collagen has not been defined to the same degree outside of the
See also
- Collagen hybridizing peptide, a peptide that can bind to denatured collagen
- Hypermobility spectrum disorder
- Metalloprotease inhibitor
- Osteoid, a collagen-containing component of bone
- Collagen loss
References
- PMID 11704682.
- ^ "Leather grown using biotechnology is about to hit the catwalk". The Economist. 26 August 2017. Archived from the original on 1 September 2017. Retrieved 2 September 2017.
- ^ Britannica Concise Encyclopedia 2007
- ISBN 978-1-56676-960-0.
- .
- ^ O.E.D. 2nd Edition 2005
- S2CID 17232196.
- ^ Sabiston textbook of surgery board review, 7th edition. Chapter 5 wound healing, question 14
- ^ PMID 21421911.
- PMID 15561712.
- S2CID 216270520.
- S2CID 136755815.
- PMID 14623404.
- PMID 11288796.
- PMID 12922147.
- S2CID 202227968.
- PMID 20186736.
- PMID 21572675.
- PMID 26858912.
- ^ "Collagen and Rosehip Extract Sachet". Alaina Pharma. Archived from the original on 4 July 2016. Retrieved 31 May 2021.
- PMID 25376879.
- PMID 21572675.
- S2CID 33438539.
- S2CID 20879450.
- ^ .
- PMID 1720597.
- PMID 20199358.
- PMID 6325436.
- PMID 4301453.
- ^ "preprocollagen". The Free Dictionary.
- PMID 7065727.
- PMID 12064927.
- ^ PMID 1425603.
- ^ PMID 16751282.
- ^ S2CID 4332269.
- PMID 18287018.
- (PDF) from the original on 27 January 2022.
- PMID 18487200.
- PMID 18220798.
- PMID 19694448.
- ^ Ross, M. H. and Pawlina, W. (2011) Histology, 6th ed., Lippincott Williams & Wilkins, p. 218.
- PMID 17850181.
- ^ "Collagen Types and Linked Disorders". News-Medical.net. 18 January 2011. Archived from the original on 1 December 2017. Retrieved 19 November 2017.
- ^ PMID 20799329.
- (PDF) from the original on 7 June 2013.
- PMID 2624272.
- S2CID 4440499.
- S2CID 39089732.
- PMID 20301386.
- ISBN 978-0-387-73905-2.
- PMID 16895989.
- ^ Dermal Fillers | The Ageing Skin Archived 13 May 2011 at the Wayback Machine. Pharmaxchange.info. Retrieved on 21 April 2013.
- .
- Penn Medicine. Philadelphia, PA: University of Pennsylvania Health System. 4 November 2018. Archived from the original on 19 September 2020. Retrieved 3 April 2023.)
{{cite web}}: CS1 maint: bot: original URL status unknown (link - PMID 35223163.
- ^ Graham Lawton (1 April 2023). "The radical new theory that wrinkles actually cause ageing". New Scientist.
- ISBN 978-1-84569-758-7.
- ^ Walker, Amélie A. (21 May 1998). "Oldest Glue Discovered". Archaeology. Archived from the original on 17 December 2005.
- PMID 8010812.
- ISSN 0261-3077. Retrieved 6 March 2023.
- ^ a b "Collagen". Harvard T.H. Chan School of Public Health: The Nutrition Source. 26 May 2021. Retrieved 6 March 2023.
- PMID 17810172.
- .
- S2CID 33745131.
- S2CID 4284147.
- S2CID 122261106. Archived from the originalon 10 January 2014.
- PMID 11468363.
- S2CID 7231304.
- PMID 458854.
- PMID 7328660.
- S2CID 4145093.
- PMID 7695699.
- S2CID 40958154.
- .
- PMID 3586015.
- PMID 9466908.
- PMID 2272900.
- PMID 11390960.
- PMID 17088555.
- PMID 19690380.
- .
