Complication (medicine)
A complication in
The development of complications depends on a number of factors, including the degree of vulnerability, susceptibility, age, health status, and immune system condition. Knowledge of the most common and severe complications of a disease, procedure, or treatment allows for prevention and preparation for treatment if they should occur.
Complications are not to be confused with sequelae, which are residual effects that occur after the acute (initial, most severe)[1] phase of an illness or injury. Sequelae can appear early in the development of disease or weeks to months later and are a result of the initial injury or illness. For example, a scar resulting from a burn or dysphagia resulting from a stroke would be considered sequelae.[2] In addition, complications should not be confused with comorbidities, which are diseases that occur concurrently but have no causative association. Complications are similar to adverse effects, but the latter term is typically used in pharmacological contexts or when the negative consequence is expected or common.
Common illnesses and complications
Iatrogenic complications
Medical errors can fall into various categories listed below:[3]
- Medication: Medication medical errors include wrong prescription, impaired delivery, or improper adherence. The process of prescribing medication is a complex process that relies on the accurate transfer of information through various parties. Prevention methods include increased use of electronic prescription, pre-packaging unit dosing, and ensuring medical literacy among patients.
- Surgical: Surgery-related medical errors can be anesthesia-related, but most often include wrong-site and wrong-patient procedural errors. Preventive measures include following and double-checking standardized surgical protocol before, during, and after procedures. Universal surgical protocols include verification of patient identity and proper site-marking.
- Diagnostic: Diagnostic errors include misdiagnosis, wrong diagnosis, and over diagnosis. Diagnostic errors are often the result of patient characteristics and physician bias.
- Machine interface: Errors in this category refer to mistakes in human interaction with tools or machines. Machine-related errors can be reduced by standardization and clear differentiation in design of products.
- Transition and handoff: Errors in this category can occur person-to-person or site-to-site during transfer, and can be managed by adhering to proper hand-off protocols.
- Human factors, teamwork, and communication: Errors in this category highlight the impact of culture and relationships on communication. These concepts can play a role in other categories of medical errors. Preventive measures include cultivating a "culture of safety" which includes creating an environment where people feel comfortable discussing concerns, feedback, and errors without fear of punishment.
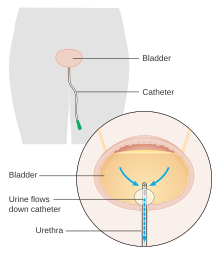
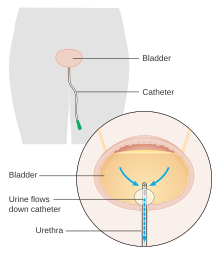
Image of a urinary catheter, a common cause of healthcare associated infections. - Healthcare-associated infections (HAIs): HAIs are complications of general treatments involving microorganisms or viral infections and are most commonly caused by indwelling devices (urinary catheters, central lines) or previous surgical procedures.[4] Common microbes involved in HAIs are Escherichia coli, Proteus mirabilis,[5] and Clostridium difficile.[4] The most effective preventive measure is hand-hygiene.[6]
Cardiovascular complications
Atrial fibrillation
A patient with atrial fibrillation may experience symptoms of fatigue, dizziness or lightheadedness, heart palpitations, chest pain, and shortness of breath.[7][8] The heart does not effectively pump blood into the pulmonary or systemic vasculature, and causes the blood to remain within the chambers of the heart.[8][9] The collection of blood within the heart due to atrial fibrillation can cause and increase the risk of development of a thrombus (blood clot).[9] The thrombus can also develop into an embolus (mobile blood clot) and travel into the systemic circulation.[9] Atrial fibrillation is associated with an increase in risk of having a stroke especially if the embolus travels to the brain.[9]
Other examples
Metabolic complications
Diabetes mellitus
- Cardiovascular disease. Adults with diabetes are significantly more likely to die from heart disease than are those without diabetes.[13] Diabetes is associated with risk factors for various cardiovascular diseases including obesity, insulin resistance, high blood cholesterol and triglyceride content, and high blood pressure. These conditions increase risk of thrombosis, atherosclerosis (blockage of coronary arteries leading to inadequate supply of oxygen to parts of the heart), and hypertension[13] which can lead to myocardial infarction, coronary artery disease (CAD), and others.
- mononeuropathy), and internal organs (autonomic neuropathy).[14] Initial symptoms may present as numbness, tingling, pain, muscular weakness, loss of reflexes or proper bodily functions, and many others.[14]
- Diabetic nephropathy. Excessive amounts of certain solutes passing through the kidneys for prolonged periods of time can lead to kidney damage.[15] Diabetic nephropathy is specifically characterized by abnormally high levels of urinary albumin excretion. This affects approximately 40% of patients with type I or type II diabetes.[16]
- Foot damage. Diabetes mellitus can lead to poor vascular blood flow to the extremities. Injury of the foot with inadequate blood flow can progress to ulcers and become infected. Individuals with diabetic neuropathy may not notice the damage[18] and may develop gangrene[19] (tissue necrosis due to inadequate blood supply).

Commonly referred to as "diabetic foot," wounds and ulcers are a common complication of elevated blood sugar levels in diabetes. - Skin conditions.[20] Insulin insensitivity in the case of type II diabetes can cause prolonged increases in blood insulin. Insulin normally binds to insulin receptors but in excess amounts may bind to insulin-like growth factor (IGF) receptors in epithelial tissue. This can cause excessive proliferation of keratinocytes and fibroblasts.[21] This presents as acanthosis nigricans, a thickening and darkening of areas of the skin such as the armpits, necks, hands, and face.[22] Other skin conditions include diabetic dermopathy, digital sclerosis, eruptive xanthomatosis, and others.
Neurologic / psychiatric complications
- Hepatic encephalopathy is a possible complication of liver cirrhosis.[23]
- Significant intellectual, physical, and developmental disability are common complications of untreated hydrocephalus.[24]
- .
- Complications of outpatient drugs are very common and many patients experience worry or discomfort due to them.[29]
- tranquilizers with varying hypnotic, sedative, anxiolytic, anticonvulsant, and muscle relaxant effects; paradoxically they may also create hyperactivity, anxiety, convulsions etc. in susceptible individuals.[30]
Reproductive complications
Pregnancy
Pregnancy is the development of an embryo or fetus inside the womb of a female for the rough duration of 9 months or 40 weeks from the last menstrual period until birth.[31] It is divided into three trimesters, each lasting for about 3 months. The 1st trimester is when the developing embryo becomes a fetus, organs start to develop, limbs grow, and facial features appear.[32] The 2nd and 3rd trimesters are marked by a significant amount of growth and functional development of the body.[31] During this time, the woman's body undergoes a series of changes and many complications may arise involving either the fetus, the mother, or both.[33]
- chronic hypertension; if it occurs after 20 weeks of gestation or pregnancy, it is gestational hypertension. A previously hypertensive mother who shows signs of gestational hypertension can lead to preeclampsia, a more severe case which can be detrimental to the mother and developing fetus.[34]
- Gestational diabetes. Appropriate levels of blood sugar is typically maintained by insulin secretion from the pancreas.[35] During pregnancy the placenta surrounding the developing fetus produces hormones that can inhibit the action of insulin, preventing the mother's blood sugar from decreasing. Occurs primarily in the second half of pregnancy and can cause excessive birth weight, preterm delivery, and place the child at greater risk for type II diabetes.[36]
- Preterm labor. Delivery of the baby prior to 37 weeks of pregnancy is considered preterm.[37] This can cause a variety of issues with the child including underdeveloped viscera (organs), behavioral or learning disabilities, low birth weight, and respiratory issues.[38]
- Miscarriage. The loss of the developing fetus prior to 20 weeks of pregnancy.[37] Common causes may be related to chromosomal abnormalities (abnormal genetic makeup) of the fetus but can also include ectopic pregnancy, maternal age, and other factors.[39]
- Stillbirth. The loss of the developing fetus after 20 weeks of pregnancy. Can be due to a variety of reasons including chromosomal abnormalities, developmental issues, or health-related problems of the mother.[37]
- Hyperemesis gravidarum.[40] Persistent, acute nausea throughout pregnancy that does not go away after the 1st trimester. Different from morning sickness which is more common and less severe.[41]

Respiratory complications
Streptococcal pharyngitis

- Scarlet fever.[47] In addition to the symptoms of strep throat, individuals may experience increased a red rash, increased red tone, and strawberry tongue.[47] The prominent rash generally fades after a few days and may peel for a few weeks.[48] Treatment is the same as for strep throat.[49]
- rheumatic heart disease.[50]
- Glomerulonephritis. Onset of kidney damage that may present a few weeks after strep infection. Rather than being a direct result of infection in the kidneys, It is believed to be caused by an overreactive immune response. Symptoms can include blood or protein in the urine, hypertension, and reduced urine output. Can lead to further kidney damage later in life[51]
- Otitis media. Infection of the middle ear.[52]
- Meningitis. Infection of the meninges of the central nervous system (brain and spinal cord) that leads to swelling. Symptoms vary and differ between adults and children but can include headaches, fever, stiff neck, and other neurological-related issues. Early treatment is important to prevent more serious complications.[53]
- Toxic shock syndrome. A severe reaction of the body to toxins produced by various bacteria such as Streptococcus pyogenes.[54] Results from an overactive response by the immune system and can cause hypotension, fever, and in more severe cases, organ failure.[55]

Surgical / procedural complications
- antisepsis and antibiotics.[56]
- Erectile dysfunction and urinary incontinence which may follow prostatectomy.[57][58]
- Malignant hyperthermia can be a reaction to general anesthetics, as a complication in a surgery.[59]
- Fractured sternum may be a complication of cardiopulmonary resuscitation attempts.[60]
Other examples of complications
- Sepsis (infection of the blood) may occur as a complication of a bacterial, viral, or fungal infection.[61]
- Miscarriage is the most common complication of early pregnancy.[62]
- eczema.
See also
- Adverse effect
- Classification of Pharmaco-Therapeutic Referrals
- Diagnosis
- Iatrogenesis
- Late effect
- Nocebo
- Placebo
- Prognosis
- Sequela
References
- ^ "Acute vs. chronic conditions: MedlinePlus Medical Encyclopedia Image". medlineplus.gov. Retrieved 2019-08-30.
- OCLC 812289395.
- OCLC 1073069539.
- ^ a b "Overview - Health Care-Associated Infections - health.gov". health.gov. Retrieved 2019-08-30.
- PMID 18202436.
- PMID 24701065.
- ^ OCLC 1029074059.)
{{cite book}}: CS1 maint: location missing publisher (link - ^ PMID 28628500.
- ^ PMID 25988464.
- ^ "Thrombophlebitis - Symptoms and causes". Mayo Clinic. Retrieved 2019-08-30.
- ^ "Endocarditis - Symptoms and causes". Mayo Clinic. Retrieved 2019-08-30.
- ^ "Heart valve surgery - Mayo Clinic". mayoclinic.org. Retrieved 2019-08-30.
- ^ a b "Cardiovascular Disease and Diabetes". heart.org. Retrieved 2019-08-30.
- ^ a b "Diabetic neuropathy - Symptoms and causes". Mayo Clinic. Retrieved 2019-08-30.
- PMID 25342915.
- PMID 15616252.
- ^ "Diabetic retinopathy - Symptoms and causes". Mayo Clinic. Retrieved 2019-08-30.
- ^ "Diabetic Foot". medlineplus.gov. Retrieved 2019-08-30.
- ^ "Diabetic Foot Problems". WebMD. Retrieved 2019-08-30.
- ^ "Diabetes - Symptoms and causes". Mayo Clinic. Retrieved 2019-08-30.
- PMID 25165638.
- ^ "Diabetes & Skin Conditions". Cleveland Clinic. Retrieved 2019-08-30.
- ^ "Cirrhosis - Symptoms and causes". Mayo Clinic. Retrieved 2019-08-30.
- ^ "Hydrocephalus - Symptoms and causes". Mayo Clinic. Retrieved 2019-08-30.
- ^ "Depression (major depressive disorder) - Symptoms and causes". Mayo Clinic. Retrieved 2019-08-30.
- ^ "Post-traumatic stress disorder (PTSD) - Symptoms and causes". Mayo Clinic. Retrieved 2019-08-30.
- ^ "Schizophrenia - Symptoms and causes". Mayo Clinic. Retrieved 2019-08-30.
- ^ "Anxiety disorders - Symptoms and causes". Mayo Clinic. Retrieved 2019-08-30.
- PMID 10718894.
- S2CID 38614605.
- ^ a b "Definition of Pregnancy". MedicineNet. Retrieved 2019-08-30.
- ^ "Fetal development: What happens during the 1st trimester?". Mayo Clinic. Retrieved 2019-08-30.
- ^ "What are some common complications of pregnancy?". nichd.nih.gov/. Retrieved 2019-09-02.
- ^ "Gestational Hypertension: Pregnancy Induced Hypertension". American Pregnancy Association. 2012-04-27. Retrieved 2019-08-30.
- PMID 16278749.
- ^ "Gestational diabetes - Symptoms and causes". Mayo Clinic. Retrieved 2019-08-30.
- ^ a b c "What are some common complications of pregnancy?". nichd.nih.gov/. Retrieved 2019-08-30.
- ^ "Preterm labor - Symptoms and causes". Mayo Clinic. Retrieved 2019-08-30.
- ^ "Miscarriage: Signs, Symptoms, Treatment and Prevention". American Pregnancy Association. 2012-04-27. Retrieved 2019-08-30.
- ^ "Pregnancy Complications | Maternal and Infant Health | CDC". cdc.gov. 2019-01-16. Retrieved 2019-08-30.
- ^ "Hyperemesis gravidarum: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2019-08-30.
- ^ a b "Group A Strep | Strep Throat | For Clinicians | GAS | CDC". cdc.gov. 2019-04-19. Retrieved 2019-09-02.
- PMID 19275067.
- ^ a b "What Are the Possible Complications of Strep Throat?". MedicineNet. Retrieved 2019-09-02.
- ^ a b "Rheumatic fever - Symptoms and causes". Mayo Clinic. Retrieved 2019-09-02.
- ^ "Strep Throat Complications | Michigan Medicine". uofmhealth.org. Retrieved 2019-09-02.
- ^ a b "Scarlet fever - Symptoms and causes". Mayo Clinic. Retrieved 2019-09-02.
- ^ "Scarlet Fever (for Parents) - KidsHealth". kidshealth.org. Retrieved 2019-09-02.
- ^ "Articles". Cedars-Sinai. Archived from the original on 2020-05-30. Retrieved 2019-09-02.
- ^ "Group A Strep | Rheumatic Fever | GAS | CDC". cdc.gov. 2019-02-21. Retrieved 2019-09-02.
- PMID 30855843, retrieved 2019-09-02
- ^ "Otitis Media". hopkinsmedicine.org. Retrieved 2019-09-02.
- ^ "Meningitis - Symptoms and causes". Mayo Clinic. Retrieved 2019-09-02.
- ^ "Toxic Shock Syndrome: Background, Pathophysiology, Etiology". 2019-01-15.
{{cite journal}}: Cite journal requires|journal=(help) - PMID 29083727, retrieved 2019-09-02
- PMID 25221345.
- ^ Mayo Clinic Staff. "Open prostatectomy risks". Mayo Clinic. Retrieved 31 October 2014.
- PMID 25261861.
- ^ "Malignant hyperthermia: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2019-08-30.
- PMID 19234634.
- ^ "Sepsis - Symptoms and causes". Mayo Clinic. Retrieved 2019-08-30.
- from the original on October 20, 2013. Retrieved July 4, 2013.
- ^ "Side Effects of Smallpox Vaccination | Smallpox | CDC". cdc.gov. 2019-02-15. Retrieved 2019-08-30.
Further reading
- Coventry BJ (2014). Surgery: Complications, Risks and Consequences. Book series, seven volumes. Springer.
- Mulholland MW, Doherty GM (2006). Complications in Surgery. Lippincott Williams and Wilkins. ISBN 978-0-7817-5316-6.
- Gawande A (2002). Complications: A Surgeon's Notes on an Imperfect Science. Macmillan.