Cytarabine
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Cytosar-U, Depocyt, others |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a682222 |
| Pregnancy category |
|
| Routes of administration | injectable (intravenous injection or infusion, intrathecal, or subcutaneously) |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 20% by mouth |
| Protein binding | 13% |
| Metabolism | Liver |
| Elimination half-life | biphasic: 10 min, 1–3 hr |
| Excretion | Kidney |
| Identifiers | |
| |
JSmol) | |
| |
| |
| (verify) | |
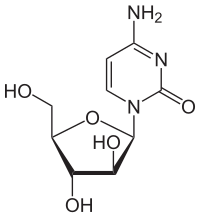
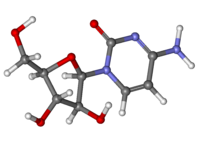
Cytarabine, also known as cytosine arabinoside (ara-C), is a
Common side effects include
Cytarabine was patented in 1960 and approved for medical use in 1969.[4] It is on the World Health Organization's List of Essential Medicines.[5]
Medical uses
Cytarabine is mainly used in the treatment of
Cytarabine also possesses
Cytarabine is also used in the study of the
Side effects
One of the unique toxicities of cytarabine is
Toxicity:
When used in protocols designated as high dose, cytarabine can cause cerebral and cerebellar dysfunction, ocular toxicity, pulmonary toxicity, severe GI ulceration and peripheral neuropathy (rare).[citation needed]
To prevent the side effects and improve the therapeutic efficiency, various derivatives of these drugs (including amino acid, peptide, fatty acid and phosphates) have been evaluated, as well as different delivery systems.[9]
Mechanism of action
Cytosine arabinoside combines a
Cytarabine is often given by continuous intravenous infusion, which follows a biphasic elimination – initial fast clearance rate followed by a slower rate of the analog.[13] Cytarabine is transported into the cell primarily by hENT-1.[14] It is then monophosphorylated by deoxycytidine kinase and eventually cytarabine-5´-triphosphate, which is the active metabolite being incorporated into DNA during DNA synthesis.[citation needed]
Several mechanisms of resistance have been reported.[15] Cytarabine is rapidly deaminated by cytidine deaminase in the serum into the inactive uracil derivative. Cytarabine-5´-monophosphate is deaminated by deoxycytidylate deaminase, leading to the inactive uridine-5´-monophosphate analog.[16] Cytarabine-5´-triphosphate is a substrate for SAMHD1.[17] Furthermore, SAMHD1 has been shown to limit the efficacy of cytarabine efficacy in patients.[18]
When used as an antiviral, cytarabine-5´-triphosphate functions by inhibiting viral DNA synthesis.[19] Cytarabine is able to inhibit herpesvirus and vaccinia virus replication in cells during tissue culture. However, cytarabine treatment was only effective for herpesvirus infection in a murine model.[citation needed]
In mice, Ara-CTP (cytarabine-5'-triphosphate) blocks memory consolidation, but not short-term memory, of a context fear conditioning event.[20] The blockage of memory consolidation was proposed to be due to the inhibition by Ara-CTP of the DNA non-homologous end joining pathway.[20] Thus transient DNA breakage followed by non-homologous end joining appear to be necessary steps in the formation of a long-term memory of an event.[citation needed]
History
Isolation of arabinose-containing nucleotides from the Caribbean sponge Cryptotheca crypta (now Tectitethya crypta) together with the realization that these compounds could act as DNA synthesis chain terminators led to exploration of these novel nucleotides as potential anticancer therapeutics.[21] Cytarabine was first synthesized in 1959 by Richard Walwick, Walden Roberts, and Charles Dekker at the University of California, Berkeley.[22]
It was approved by the United States Food and Drug Administration in June 1969, and was initially marketed in the US by Upjohn under the brand name Cytosar-U.[citation needed]
Names
It is also known as ara-C (arabinofuranosyl cytidine).[23]
- Cytosar-U
- Tarabine PFS (Pfizer)
- Depocyt (longer-lasting liposomalformulation)
- AraC
References
- FDA. Retrieved 22 Oct 2023.
- ^ a b c d e f g "Cytarabine". The American Society of Health-System Pharmacists. Archived from the original on 11 June 2016. Retrieved 8 December 2016.
- ISBN 9780857111562.
- ISBN 9783527607495. Archivedfrom the original on 2016-12-20.
- hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- PMID 18024370.
- PMID 15825312.
- PMID 7954266.
- S2CID 2988492.
- ^ Hall D (November 2019). "Sea Sponges: Pharmacies of the Sea". Smithsonian Ocean. Retrieved 25 April 2023.
- ISBN 978-0-7817-7328-7.
- ^ Feist P (April 2005). "A Tale from the Sea to Ara C". Archived from the original on 2007-03-06.
- PMID 3589691.
- PMID 12481710.
- PMID 27960273.
- PMID 20227960.
- PMID 28046007.
- S2CID 205398095.
- ISBN 0-683-30737-1.
- ^ PMID 16707804.
- PMID 11905767.
- ISBN 0-471-89979-8.
- PMID 19048119.
