Demyelinating disease
| Demyelinating disease | |
|---|---|
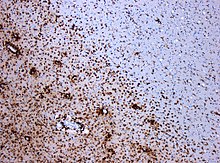 | |
| Photomicrograph of a demyelinating MS-lesion: Immunohistochemical staining for CD68 highlights numerous macrophages (brown). Original magnification 10×. | |
| Specialty | Neurology |
A demyelinating disease refers to any
Various factors can contribute to the development of demyelinating diseases, including
Demyelinating diseases are traditionally classified into two types: demyelinating myelinoclastic diseases and demyelinating leukodystrophic diseases. In the first group, a healthy and normal myelin is destroyed by toxic substances, chemicals, or autoimmune reactions. In the second group, the myelin is inherently abnormal and undergoes degeneration.[6] The Poser criteria named this second group dysmyelinating diseases.[7]
In the most well-known demyelinating disease,
Signs and symptoms
Symptoms and signs that present in demyelinating diseases are different for each condition. These symptoms and signs can present in a person with a demyelinating disease:[9]
- Blurred double vision (Diplopia)
- Ataxia
- Clonus
- Dysarthria
- Fatigue
- Clumsiness
- Hand paralysis
- Hemiparesis
- Genital anaesthesia
- Incoordination
- Paresthesias
- Ocular paralysis (cranial nerve palsy)
- Impaired muscle coordination
- Weakness (muscle)
- Loss of sensation
- Impaired vision
- Unsteady gait
- Spastic paraparesis
- Incontinence
- Hearing problems
- Speech problems
Evolutionary considerations
The role of prolonged cortical myelination in human evolution has been implicated as a contributing factor in some cases of demyelinating disease. Unlike other primates, humans exhibit a unique pattern of postpubertal myelination, which may contribute to the development of psychiatric disorders and neurodegenerative diseases that present in early adulthood and beyond. The extended period of cortical myelination in humans may allow greater opportunities for disruption in myelination, resulting in the onset of demyelinating disease.[10] Furthermore, humans have significantly greater prefrontal white matter volume than other primate species, which implies greater myelin density.[11] Increased myelin density in humans as a result of a prolonged myelination may, therefore, structure risk for myelin degeneration and dysfunction. Evolutionary considerations for the role of prolonged cortical myelination as a risk factor for demyelinating disease are particularly pertinent given that genetics and autoimmune deficiency hypotheses fail to explain many cases of demyelinating disease. As has been argued, diseases such as multiple sclerosis cannot be accounted for by autoimmune deficiency alone, but strongly imply the influence of flawed developmental processes in disease pathogenesis.[12] Therefore, the role of the human-specific prolonged period of cortical myelination is an important evolutionary consideration in the pathogenesis of demyelinating disease.[citation needed]
Diagnosis
Various methods/techniques are used to diagnose demyelinating diseases:
- Exclusion of other conditions that have overlapping symptoms[13]
- Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to visualize internal structures of the body in detail. MRI makes use of the property of nuclear magnetic resonance (NMR) to image nuclei of atoms inside the body. This method is reliable because MRIs assess changes in proton density. "Spots" can occur as a result of changes in brain water content.[13]: 113
- electrical potential recorded from the nervous system following the presentation of a stimulus as detected by electroencephalography (EEG), electromyography (EMG), or other electrophysiological recording method.[13]: 117
- Cerebrospinal fluid analysis (CSF) can be extremely beneficial in the diagnosis of central nervous system infections. A CSF culture examination may yield the microorganism that caused the infection.[13]
- Quantitative proton magnetic resonance spectroscopy (MRS) is a noninvasive analytical technique that has been used to study metabolic changes in brain tumors, strokes, seizure disorders, Alzheimer's disease, depression, and other diseases affecting the brain. It has also been used to study the metabolism of other organs such as muscles.[13]: 309
- Diagnostic criteria refers to a specific combination of signs, symptoms, and test results that the clinician uses in an attempt to determine the correct diagnosis.[13]: 320
- Fluid-attenuated inversion recovery (FLAIR) uses a pulse sequence to suppress cerebrospinal fluid and show lesions more clearly, and is used for example in multiple sclerosis evaluation.
Types
Demyelinating diseases can be divided in those affecting the central nervous system (CNS) and those affecting the peripheral nervous system (PNS). They can also be classified by the presence or absence of inflammation. Finally, a division may be made based on the underlying cause of demyelination: the disease process can be demyelinating myelinoclastic, wherein myelin is destroyed; or dysmyelinating leukodystrophic, wherein myelin is abnormal and degenerative.
CNS
The demyelinating disorders of the central nervous system include:[citation needed]
- Myelinoclastic or demyelinating disorders:
- Typical forms of multiple sclerosis
- Neuromyelitis optica, or Devic's disease
- Idiopathic inflammatory demyelinating diseases
- Leukodystrophic or dysmyelinating disorders:
- CNS neuropathies such as those produced by vitamin B12 deficiency
- Central pontine myelinolysis
- Myelopathies such as tabes dorsalis (syphilitic myelopathy)
- Leukoencephalopathies such as progressive multifocal leukoencephalopathy
- Leukodystrophies
The myelinoclastic disorders are typically associated with symptoms such as
PNS

The demyelinating diseases of the peripheral nervous system include:[citation needed]
- Guillain–Barré syndrome and its chronic counterpart, chronic inflammatory demyelinating polyneuropathy
- Anti-MAG peripheral neuropathy
- Charcot–Marie–Tooth disease and its counterpart Hereditary neuropathy with liability to pressure palsy
- Copper deficiency-associated conditions (peripheral neuropathy, myelopathy, and rarely optic neuropathy)
- Progressive inflammatory neuropathy
Treatment
Treatments are patient-specific and depend on the symptoms that present with the disorder, as well as the progression of the condition. Improvements to the patient's life may be accomplished through the management of symptoms or slowing of the rate of demyelination. Treatment can include medication, lifestyle changes (i.e. smoking cessation, increased rest, and dietary changes), counselling, relaxation, physical exercise, patient education, and in some cases, deep brain thalamic stimulation (to ameliorate tremors).[13]: 227–248
Prognosis
Prognosis depends on the condition itself. Some conditions such as MS depend on the subtype of the disease and various attributes of the patient such as age, sex, initial symptoms, and the degree of disability the patient experiences.[14] Life expectancy in MS patients is 5 to 10 years lower than unaffected people.[15] MS is an inflammatory demyelinating disease of the central nervous system (CNS) that develops in genetically susceptible individuals after exposure to unknown environmental trigger(s). The bases for MS are unknown but are strongly suspected to involve immune reactions against autoantigens, particularly myelin proteins. The most accepted hypothesis is that dialogue between T-cell receptors and myelin antigens leads to an immune attack on the myelin-oligodendrocyte complex. These interactions between active T cells and myelin antigens provoke a massive destructive inflammatory response and promote continuing proliferation of T and B cells and macrophage activation, which sustains secretion of inflammatory mediators.[16] Other conditions such as central pontine myelinolysis have about a third of patients recover and the other two-thirds experience varying degrees of disability.[17] In some cases, such as transverse myelitis, the patient can begin recovery as early as 2 to 12 weeks after the onset of the condition.[citation needed]
Epidemiology
Incidence of demyelinating diseases varies by disorder. Some conditions, such as tabes dorsalis appear predominantly in males and begin in midlife. Optic neuritis, though, occurs preferentially in females typically between the ages of 30 and 35.[18] Other conditions such as multiple sclerosis vary in prevalence depending on the country and population.[19] This condition can appear in children and adults.[15]
Research
Much of the research conducted on demyelinating diseases is targeted towards discovering the mechanisms by which these disorders function in an attempt to develop therapies and treatments for individuals affected by these conditions. For example, proteomics has revealed several proteins which contribute to the pathophysiology of demyelinating diseases.[20] For example,
Immunomodulatory drugs such as fingolimod have been shown to reduce immune-mediated damage to the CNS, preventing further damage in patients with MS. The drug targets the role of macrophages in disease progression.[26][27]
Manipulating
In other animals
Demyelinating diseases/disorders have been found worldwide in various animals. Some of these animals include mice, pigs, cattle, hamsters, rats, sheep, Siamese kittens, and a number of dog breeds (including Chow Chow, Springer Spaniel, Dalmatian, Samoyed, Golden Retriever, Lurcher, Bernese Mountain Dog, Vizsla, Weimaraner, Australian Silky Terrier, and mixed breeds).[31][32]
See also
- Degenerative disease
- Multiple sclerosis borderline
- The Lesion Project(multiple sclerosis)
- The Myelin Project
- Myelin Repair Foundation
References
- ^ "demyelinating disease" at Dorland's Medical Dictionary
- S2CID 29313644.
- PMID 17945195.
- PMID 23984056.
- PMID 29675077.
- .
- PMID 13737358.
- ^ Laetoli (January 2008). "Demyelination". Archived from the original on 2012-07-28.
- ^ "Symptoms of Demyelinating Disorders - Right Diagnosis." Right Diagnosis. Right Diagnosis, 01 Feb 2012. Web. 24 Sep 2012
- PMID 23012402.
- S2CID 205430527.
- S2CID 8575687.
- ^ ISBN 0781751705.
- S2CID 7140070.
- ^ S2CID 195686659.
- S2CID 10189144.
- PMID 16210283.
- S2CID 25800388.
- S2CID 207051545.
- PMID 15652809.
- PMID 21699540.
- S2CID 205834726.
- PMID 24961530.
- S2CID 33883037.
- S2CID 207357858.
- PMID 22888218.
- PMID 12401395.
- S2CID 1534460.
- S2CID 28658807.
- S2CID 15779187.
- ^ "Merck Veterinary Manual – Demyelinating Disorders: Introduction". Archived from the original on 2010-12-19. Retrieved 2012-10-30.
- ^ Johnson RT (2004). "Demyelinating Diseases". The Infectious Etiology of Chronic Diseases: Defining the Relationship, Enhancing the Research, and Mitigating the Effects: Workshop Summary. NIH.
