Dental extraction
This article may need to be rewritten to comply with Wikipedia's quality standards. (February 2024) |
| Dental extraction | |
|---|---|
Periodontics[1] | |
| ICD-9-CM | 23.0-23.1 |
| MeSH | D014081 |
A dental extraction (also referred to as tooth extraction, exodontia, exodontics, or informally, tooth pulling) is the removal of
Procedure
Extractions could be categorized into non-surgical (simple) and surgical, depending on the type of tooth to be removed and other factors.

Assessment and special investigations
A comprehensive history taking should be performed to find out the pain history of the tooth, the patient's medical history and the history of previous difficult extractions.[2] The tooth should be assessed clinically i.e. checked visually by the dentist.[2] Pre-extraction radiographs are not always necessary but are often taken to confirm the diagnosis and hence appropriate treatment plan.[2] Radiographs also help in visualising the shape and size of roots which are beneficial in planning the extraction.[2] All this information will aid the dentist in foreseeing any difficulties and hence preparing appropriately.[2]
Obtaining consent from patient
In order to obtain permission from patient for extraction of tooth, the dentist should explain that other treatment options are available, what is involved in the dental extraction procedure, the potential risks of the procedure and the benefits of the procedure.[2] The process of gaining consent should be documented in clinical notes.[2]

Giving local anaesthetic
Before extracting a tooth, the dentist would deliver local anaesthetic to ensure the tooth and surrounding tissues are numb before they start the extraction.[2] There are several techniques to achieve numbness of the tooth including
- infiltration – injection containing local anaesthetic is delivered into the gum near the root tip of the tooth to be extracted. This allows the local anaesthetic to penetrate through the bone, eventually reaching the nerve bundle of the tooth to be extracted.[2]
- nerve block – injection containing local anaesthetic is delivered to an earlier branch of a nerve. For example, the inferior alveolar nerve block can be used to anaesthetise all the lower teeth.[2]
The two most commonly used local anaesthetics in the UK are lidocaine and articaine.[3] Prior to injection, topical anaesthetic gel or cream, such as lidocaine or benzocaine, can be applied to the gum to numb the site of the injection up to a few millimetres deep.[2] This should reduce the discomfort felt during the injection and thus help to reduce patient anxiety.[2]

Removal of tooth
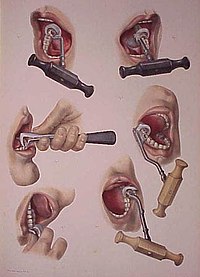
During extraction, multiple instruments are used to aid and ease the removal of the tooth whilst trying to minimally traumatise the tissues to allow for quicker healing. Extraction forceps are commonly used to remove teeth. Different shaped forceps are available depending on the type of tooth requiring removal, what side of the mouth (left or right) it is on and if it is an upper or lower tooth. The beaks of the forceps must grip onto the root of the tooth securely before pressure is applied along the long axis of the tooth towards the root.
Different movements of the forceps can be employed to remove teeth. Generally, while keeping downwards pressure attempts to move the tooth towards the cheek side (buccal) and then the opposite direction (palatal or lingual) are made to loosen the tooth from its socket.[2] For single, conical-rooted teeth such as the incisors, rotatory movements are also used.[2] A 'figure of eight' movement can be used to extract lower molars.[2]

Instruments used are summarised below:
| Name | Type of instrument | Use | Area of use | Unique features |
|---|---|---|---|---|
| Luxator | Luxator | Tear PDL around tooth | Anywhere | Sharp blade |
| Coupland | Elevator | expand socket and lift | Anywhere | Numbered 1-3 from most narrow to wide |
| Warrick James | Elevator | Expand socket and lift tooth | Anywhere | Right left and straight |
| Cryers | Elevator | Expand socket and lift tooth | Anywhere | Right and left with sharp tips |
| Upper straight | Forcep | Remove teeth | Upper canine to canine | Straight handle |
| Upper anterior | Forcep | Remove teeth | Upper anteriors and premolars | |
| Upper molar | Forcep | Remove teeth | Upper 1st/2nd/3rd molars | One pointed end to engage buccal furcation |
| Upper bayonet | Forcep | Remove teeth | Upper 3rd molars | Curved handle and tip to reach 3rd molars |
| Upper root | Forcep | Remove teeth | Upper retained/fractured roots | Narrow tips |
| Cowhorn | Forcep | Remove teeth | Lower molars | Thin tips to engage furcation of broken down molars |
| Lower anterior | Forcep | Remove teeth | Lower anteriors and premolars | 90 degree bend handle |
| lower molar | Forcep | Remove teeth | Lower 1st/2nd/3rd molars | 2 beak tips to engage furcations |
| Lower root | Forcep | Remove teeth | Lower retained/fractured roots | Narrow tips to engage roots |
In terms of operator positioning when removing a tooth, the patient is placed more supine when extracting an upper and more upright when extracting a lower. This is to allow direct vision for the operator during the procedure. A right handed operator will stand to the front of the patient and to their right when removing any upper teeth or lower left teeth. However, they will stand behind the patient and to the right when extracting a lower right tooth.[4]
Dental elevators can be used to aid removal of teeth. Various types are available that have different shapes. Their working ends are designed to engage into the space between the tooth and bone of the socket.[2] Rotatory movements are then made to dislodge the tooth from the socket.[2] Another similar looking but sharper instrument that can be used is a luxator; this instrument can be used gently and with great care to cut the ligament between the tooth and its boney socket (periodontal ligament).[2]
Achieving haemostasis
Biting down on a piece of sterile gauze over the socket will provide firm pressure to the wound. Normally this is sufficient to stop any bleeding and will promote blood clot formation at the base of the socket.[5]
Moreover, the patient must be inhibited from eating and drinking hot food in the first 24 hours. Using straw for drinking is also prohibited due to the negative pressure it can produce which will lead to removal of a newly formed clot from the socket.
The source of any bleeding can either be from soft tissues (
Reasons


Medical/Dental
- Severe third molar) teeth, accounting for up to two thirds of extractions.[7]
- Severe gum disease, which may affect the supporting tissues and bone structures of teeth.
- Treatment of symptomatic impacted wisdom teeth e.g. that are associated with pericoronitis, unrestorable caries or cysts.[8]
- Prophylactic removal of asymptomatic impacted wisdom teeth. Historically, many asymptomatic impacted third molars were removed, however, both American and British Health Authorities now provide guidance about the indication for third molar removal.[8] The American Public Health Association, for example, adopted a policy, Opposition to Prophylactic Removal of Third Molars (Wisdom Teeth), because of the large number of injuries resulting from unnecessary extractions.[9]
- Supernumerary teeththat are blocking other teeth from coming in.
- Supplementary or malformed teeth.
- Fractured teeth.
- Teeth in the fracture line of the jaw bone
- Teeth which cannot be restored
- Head and neck tumors, may require extraction of teeth, either before or after radiation treatments.
- Lower cost, compared to other treatments.[13]: 98
- Medically unnecessary extraction as a form of physical torture.[14]
- It was once a common practice to remove the front teeth of institutionalized psychiatric patients who had a history of biting.[15]
Orthodontic
- In preparation for teeth are the most commonly extracted teeth for this purpose.
Aesthetics
- Cosmetic: to remove teeth of poor appearance, unsuitable for restoration.
Types

Extractions are often categorized as "simple" or "surgical".
Simple extractions are performed on teeth that are visible in the mouth, usually with the patient under local

Surgical extractions involve the removal of teeth that cannot be easily accessed or removed via simple extraction, for example because they have broken under the
Common risks after any extraction include pain, swelling, bleeding, bruising, infection, trismus (not being able to open as wide as normal) and dry socket. There are additional risks associated with the surgical extraction of wisdom teeth in particular: permanent or temporary damage to the inferior alveolar nerve +/- lingual nerve, causing permanent or temporary numbness, tingling or altered sensation to the lip, chin +/- tongue.[16][17]
Surgical procedure
- Incisions are made full thickness through mucosa and periosteum to bone. In general, the flap is extended from one tooth behind the tooth concerned to one tooth in front, including the interdental papilla.
- An anterior relieving incision is made extending down into the sulcus. This flap design is called “two sided”. A “three sided” flap includes an additional relieving incision posteriorly.
- The flap is raised using periosteal elevator to expose the area of interest.
- The flap is held out of the way with an instrument such as a rake retractor.
- A small gutter of bone is drilled away around the tooth to make space into which an application point for instruments can be achieved. It is important that copious amount of saline is used to cool the bone during this process.
- The tooth concerned can be removed using a combination of luxators, elevators and extraction forceps.
- Any sharp bone is smoothed off and the wound is irrigated with saline.
- The flap is repositioned and sutured in place.[2]
Pre-extraction consideration
Anticoagulant/Antiplatelet Use
Antibiotic Prescribing
Individual patient circumstances should be evaluated prior to the use of
Assessing risk of nerve damage
The inferior alveolar nerve (IAN), a branch of the trigeminal nerve (cranial nerve V), is a nerve that runs through the mandible (lower jaw) and supplies sensation to all the lower teeth, the lip and the chin. The lower teeth, and in particular the lower wisdom teeth, can therefore be in close proximity to this nerve. Damage to the inferior alveolar nerve is a risk of lower wisdom tooth removal (and other surgical procedures in the mandible).[20] This means there is a risk of temporary or permanent numbness or altered sensation to the lip +/- chin on the side the surgery is taking place. Therefore, in order to assess this risk and inform the patient, the position of the inferior alveolar nerve in relation to a lower wisdom tooth needs to be assessed radiographically prior to extraction.[20]
The proximity of the root to the canal can be assessed radiographically and there are several factors which can indicate high risk of nerve damage:[21]
- Darkening of the tooth root where it crosses the canal[21]
- Deviation of the canal[21]
- Narrowing of the roots[21]
- Loss of the lamina dura of the canal[21]
- Juxta apical area: a radiolucency associated with the root of the tooth which is not caused by periapical infection[21]
The lingual nerve can also be damaged (temporary or permanent) during surgical procedures in the mandible, in particular lower wisdom tooth removal. This would present as temporary or permanent numbness/altered sensation/altered taste to the side of tongue (side corresponding to side of surgery).[22]
Post-extraction healing

Immediate management
Immediately following the removal of a tooth, bleeding or oozing very commonly occurs. Pressure is applied by the patient biting on a
Complications
Talking, which moves the mandible and hence removes the pressure applied on the socket, instead of keeping constant pressure, is a very common reason that bleeding might not stop. This is likened to someone with a bleeding wound on their arm, when being instructed to apply pressure, instead holds the wound intermittently every few moments.
The most serious post extraction healing complication is that slow or halted healing caused by the adverse effects of use of bisphosphonates which can cause osteochemonecrosis of the bone.
Healing process
The chance of further bleeding reduces as healing progresses, and is unlikely after 24 hours. The blood clot is covered by
Post-extraction management
Post-operative instructions
Post-operative instructions following tooth extractions can be provided to encourage healing of the socket and prevent post-operative complications from arising. The advice listed below is usually given verbally, and can be supplemented with instructions in the written form. The combination of both methods of delivery has been found to reduce the severity of pain experienced by patients post-extraction and results in higher levels of patient satisfaction compared to verbal post-operative instructions alone.[25]
General advice

The following can be recommended to encourage healing after a tooth extraction.
- Avoid exploration of the tooth socket with the tongue, a finger or toothbrush - otherwise this might disturb clot formation
- Avoid rinsing mouth for 24 hours to prevent dislodging the blood clot.[2] After 24 hours has passed use warm salty mouthwashes especially after meals to keep the wound clean.[26] Patients may be advised to use a plastic syringe with a curved tip to clean the sockets during the healing process, though evidence for the effectiveness of this practice is limited.[27]
- Avoid alcohol for at least 24 hours[28]
- Try to relax for the remainder of the day, avoiding strenuous activities that will cause an increase in blood pressure as this might disrupt clot formation[29]
- For a few days, adopt a diet consisting of soft foods[26]
Pain management
Many drug therapies are available for pain management after third molar extractions including NSAIDS (
Socket preservation
Post-extraction bleeding
Post-extraction bleeding is bleeding that occurs 8–12 hours after tooth extraction.[36] It is normal for bleeding to occur for up to 30 minutes following the extraction. It is not uncommon for the extraction site to discharge a small amount of blood or to see saliva blood-stained for up to 8 hours.[37]
Should post-extraction bleeding occur, UK guidance recommends biting onto a piece of damp gauze for at least 20 minutes whilst sitting in an upright position.[28] It is important that the gauze is damp, but not soaking, to avoid disrupting clot formation and consequently inducing a rebound bleed. If the socket continues to bleed, it is recommended to repeat the process with a fresh piece of damp gauze for 20 minutes again. Should both attempts fail to stem the bleed, it is advised to seek professional advice.
Factors
Various factors contribute to post-extraction bleeding.[38][39][40]
Local factors
- Laceration of blood vessels
- Osseousbleeding from nutrients canal/ central vessels
- Inflammation
- Infection
- Traumatic extraction
- Failure of patient to follow post-extraction instructions
Systemic factors
- Platelet problem
- Coagulation disorder/ excessive fibrinolysis
- Inherited/medication-induced problems
Type of bleeding
1. Primary prolonged bleeding
This type of bleeding occurs during/immediately after extraction, because true haemostasis has not been achieved. It is usually controlled by conventional techniques, such as applying pressure packs or
2. Reactionary bleeding
This type of bleeding starts 2 to 3 hours after tooth extraction, as a result of cessation of vasoconstriction. Systemic intervention might be required.
3. Secondary bleeding
This type of bleeding usually begins 7 to 10 days post extraction, and is most likely due to infection destroying the blood clot or ulcerating local vessels.
Interventions
There is no clear evidence from clinical trials comparing the effects of different interventions for the treatment of post-extraction bleeding.[41] In view of the lack of reliable evidence, clinicians must use their clinical experience to determine the most appropriate means of treating this condition, depending on patient-related factors.[41]
Complications
- antibiotics pre- and/or post-operatively if he or she determines the patient to be at risk of infection.[42]
- Prolonged bleeding: The dentist has a variety of means at his/her disposal to address bleeding; however, small amounts of blood mixed in the saliva after extraction are normal, even up to 72 hours after extraction. Usually, however, bleeding will almost completely stop within eight hours of the surgery, with only minuscule amounts of blood mixed with saliva coming from the wound. A gauze compress will significantly reduce bleeding over a period of a few hours.[43]

- Swelling: Often dictated by the amount of surgery performed, to extract a tooth (e.g., surgical insult to the tissues, both hard and soft, surrounding a tooth). Generally, when a surgical flap must be elevated (i.e., the periosteumcovering the bone is thus injured), minor to moderate swelling will occur. A poorly cut soft tissue flap, for instance, where the periosteum is torn off rather than cleanly elevated off the underlying bone, will often increase such swelling. Similarly, when bone must be removed using a drill, more swelling is likely to occur.
- Bruising: Bruising may occur as a complication after tooth extraction.[44] Bruising is more common in older people or people on aspirin or steroid therapy. It may take weeks for bruising to disappear completely.

Recovery of swelling and bruises over time - bacterial flora, decongestants, and careful instructions to follow during the healing period.[46]
- Displacement of tooth or part of the tooth into the maxillary sinus (upper teeth only). In such cases, the tooth or tooth fragment must almost always be retrieved. In some cases, the sinus cavity can be irrigated with saline (antral lavage) and the tooth fragment may be brought back to the site of the opening through which it entered the sinus, and may be retrievable. At other times, a window must be made into the sinus in the Canine fossa—a procedure referred to as a "Caldwell-Luc".[49]

- Dry-socket (Alveolar osteitis) is a painful phenomenon that most commonly occurs a few days after the removal of mandibular (lower) wisdom teeth. It typically occurs when the blood clot within the healing tooth extraction site is disrupted. More likely,[50] alveolar osteitis is a phenomenon of painful inflammation within the empty tooth socket because of the relatively poor blood supply to this area of the mandible (which explains why dry-socket is usually not experienced in other parts of the jaw). Inflamed alveolar bone, unprotected and exposed to the oral environment after tooth extraction, can become packed with food and debris. Dry-socket typically causes a sharp and sudden increase in pain commencing 2–5 days following the extraction of a mandibular molar, most commonly the third molar.[51] This is often extremely unpleasant for the patient; the only symptom of dry-socket is pain, which often radiates up and down the head and neck. A dry-socket is not an infection, and is not directly associated with swelling because it occurs entirely within bone – it is a phenomenon of inflammation, within the bony lining, of an empty tooth socket. Because dry-socket is not an infection, the use of antibiotics has no effect on its rate of occurrence. There is some evidence that rinsing with chlorhexidine before or after extraction or placing chlorhexidine gel in the sockets of extracted teeth provides a benefit in preventing dry-socket, but potential adverse effects of chlorhexidine have to be considered.[51][52] The risk factorfor alveolar osteitis can dramatically increase with smoking after an extraction.
- Bone fragments: Particularly when extraction of molars is involved, it is not uncommon for the bones which formerly supported the tooth to shift and in some cases to erupt through the gums, presenting protruding sharp edges which can irritate the tongue and cause discomfort. This is distinguished from a similar phenomenon, where, broken fragments of bone or tooth left over from the extraction can also protrude through the gums. In the latter case, the fragments will usually work their way out on their own. In the former case, the protrusions can either be snipped off by the dentist, or eventually the exposed bone will erode away on its own.
- Maxilla tuberosity fracture: Can occur especially during molar extractions. There can be a variety of factors causing this including single standing molar, extracting in the wrong order, inadequate alveolar support, pathological gemination or extension of maxillary sinus weakening the area.[53]
- Trismus: Trismus, also known as lockjaw, affects functions of the oral cavity by restricting opening of the mouth. A double blind, clinical study was done to test the effect of two different medications on post-extraction trismus. The patients who received a corticosteroid by IV had a statistically significant lower level of trismus when compared to patients receiving an NSAID by IV or no medication.[54]
- Loss of a tooth: If an extracted tooth slips out of the forceps, it may be swallowed or inhaled. The patient may be aware of swallowing it, or, they may cough, which suggests inhalation of the tooth. The patient must be referred for a chest X-ray in hospital if a tooth cannot be found. If it has been swallowed, no action is necessary as it usually passes through the alimentary canal without doing any harm. But if it has been inhaled, an urgent operation is necessary to recover it from the airway or lung before it causes serious complications such as pneumonia or a lung abscess.[12]
- Luxationof the adjacent tooth: The application of force during the extraction procedure must strictly be limited to the tooth that requires the extraction. Most cases of surgical extraction procedures require that the forces are diverted from the tooth itself to areas such as bone surrounding the tooth to ensure adequate bone removal before proceeding any further in the extraction procedure. Either way, the forces applied by various instruments during both simple and complicated surgical procedure may loosen the teeth present both in front of or behind the tooth depending upon the impact direction and location of the force being applied and that happening only if the forces divert from the actual tooth that needs extraction. Such deleterious forces may weaken the anchorage of adjacent teeth from within their bony socket, and hence result in weakening of the adjacent teeth.
- Extraction of the wrong tooth: Misdiagnosis, altered tooth morphology, faulty clinical examination, poor patient history, undetected/unmentioned previous extractions that may predispose the operator to consider another tooth to be a replicate of the one previously extracted are a few causes of extraction of a wrong tooth.
- Osteonecrosis: Osteonecrosis of the jaw is the slow destruction of bone in an extraction site. A case control study of 191 cases and 573 controls were used to understand the relationship between osteonecrosis of the jaw and prior usage of bisphosphonate drugs, which are commonly prescribed to treat osteoporosis. All of the participants were over 40 years of age, mostly female, and had been taking bisphosphonates for six months or longer. The presence of osteonecrosis of the jaw was reported by dentists' previous diagnosis of the participating case and control patient's medical records. Reports showed that women using bisphosphonates for more than two years are ten times more likely to experience osteonecrosis of the jaw, while women who have taken bisphosphonates for less than two years are four times more likely to suffer from osteonecrosis of the jaw when compared to women who were not taking bisphosphonates. Therefore, it is extremely important to report all medications used to the dentist before an extraction, so that osteonecrosis can be avoided.[55]
Atraumatic extraction
Atraumatic extraction is a novel technique for extracting teeth with minimal trauma to the bone and surrounding tissues. It is especially useful in patients who are highly susceptible to complications such as bleeding,
Replacement options for missing teeth
Following dental extraction, a gap is left. The options to fill this gap are commonly recorded as Bind, and the choice is made by dentist and patient based on several factors.
| Treatment option | Advantages | Disadvantages |
|---|---|---|
| Bridge | Fixed to adjacent teeth | Drilling usually required on one or both sides of the gap if conventional bridge (average lifespan about 10 years). Conservative bridge (average lifespan about 5 years) preparation may cause minimal damage to adjacent teeth. Expensive and complex treatment, not suited to all situations, e.g., large gaps in the back of the mouth Alveolar bone will still resorb, and eventually a gap may show under bridge.
|
| Implant | Fixed to jawbone. Maintains alveolar bone, which would otherwise undergo resorption. Usually a long-term lifespan. | Expensive and complex, requiring specialist. May involve other procedures such as bone grafting. Relatively contra-indicated in tobacco smokers. |
Denture |
Often a simple, quick, and relatively cheap treatment compared to bridge and implant. Not usually any drilling of other teeth required. It is far easier to replace several teeth with a denture than place multiple bridges or implants. | Denture is not fixed in mouth. Over time worsens gag reflex, xerostomia , etc.
|
| Nothing (i.e., not replacing the missing tooth) | Often the choice due to cost of other treatment or lack of motivation for other treatments. Part of a shortened dental arch plan, which revolves around the fact that not all teeth are required to eat comfortably, and only the incisors and premolars need be preserved for normal function. This is usually the choice taken if the reason of dental extraction is due to impacted wisdom teeth or orthodontics because of limited space. | The alveolar bone will slowly resorb over time once the tooth is lost. Potential esthetic concern. Potential for drifting and rotation of adjacent teeth into the gap over time. |
History
Historically, dental extractions have been used to treat a variety of illnesses. Before the discovery of
See also
- Tooth regeneration
- Dental evulsion
References
- ^ "Tooth extraction: MedlinePlus Medical Encyclopedia". MedlinePlus. Retrieved 3 February 2024.
tooth extraction is a procedure to remove a tooth from the gum socket. It is usually done by a general dentist, an oral surgeon, or a periodontist.
- ^ OCLC 45708690.
- S2CID 3343775.
- ISBN 0443070830.
- ^ PMID 24930250.
- ISBN 9780071808682.
- PMID 18718782.
- ^ ISBN 9781473131484. Archivedfrom the original on 7 April 2019. Retrieved 15 July 2019.
- ^ "Opposition to Prophylactic Removal of Third Molars (Wisdom Teeth)". Policy Statement Database. American Public Health Association. 12 May 2016. Archived from the original on 2 December 2018. Retrieved 12 May 2016.
- PMID 36943972.
A dental extraction would be indicated for a tooth with pulpal, or apical pathology that cannot be resolved with endodontic treatment or that would not be restorable following the endodontic treatment.
- ^ "Other Endodontic Treatment Options". American Association of Endodontists. 25 June 2022. Retrieved 3 February 2024.
Do everything possible to save your teeth before considering extraction – it should always be a last resort! If an endodontic procedure can't save your tooth and it must be extracted, you should consider a dental implant that will enable you to bite and chew properly,...
- ^ ISBN 978-1-4051-7557-9.
- ISBN 9780323049030.
- S2CID 22188815.
- ISBN 9780781734738.
- PMID 25635208.
- PMID 12222906.
- ^ "Management of Dental Patients Taking Anticoagulants or Antiplatelet Drugs" (PDF). Scottish Dental Clinical Effectiveness Programme. Archived (PDF) from the original on 28 March 2017. Retrieved 22 November 2016.
- ^ PMID 33624847.
- ^ PMID 24422029.
- ^ PMID 23909229.
- PMID 24157759.
- ^ "Management of Dental Patients taking Anticoagulant or Anti Platelet Drug" (PDF). Archived (PDF) from the original on 28 March 2017. Retrieved 22 November 2016.
- ISBN 9780323045575.
- S2CID 46888257.
- ^ PMID 15789315.
- PMID 28498604.
- ^ ISBN 978-1-905829-04-0.
- ^ "Management of Acute Dental Problems" (PDF). Scottish Dental Clinical Effectiveness Programme. 2013. Archived (PDF) from the original on 4 February 2022. Retrieved 25 January 2022.
- PMID 23904576.
- from the original on 12 June 2018. Retrieved 10 June 2018.
- PMID 22567435.
- ISSN 2314-4025.
- (PDF) from the original on 1 July 2015. Retrieved 18 June 2014.
- S2CID 4954931.
- PMID 29502332.
- PMID 29502332.
- PMID 27499028.
- S2CID 4237610.
- OCLC 316027998.
- ^ PMID 29502332.
- PMID 34211554.
- PMID 29502332.
- PMID 18088673.
- ^ MD, Philip Scolaro (4 May 2021). "How to Tell if Your Tooth Extraction is Causing Your Sinus Problem". Ear Nose and Throat Doctors. Retrieved 14 December 2023.
- PMID 22117943.
- PMID 25635208.
- PMID 24740534.
- from the original on 26 February 2022. Retrieved 25 February 2022.
- PMID 20652078.
- ^ PMID 36156769.
- PMID 23579300.
- PMID 19212477.
- PMID 24473372.
- PMID 21317246.
- PMID 24453455.
- ^ Syndesmotomy Archived 2021-01-19 at the Wayback Machine; medical-dictionary.the freedictionary.com; accessed 2020-08-27
- ^ "Dental pelican for tooth pulling, Europe, 1701–1800". sciencemuseum.org.uk. Brought to Life. Archived from the original on 4 October 2013. Retrieved 18 February 2014.
- ^ Ribitzky G. "Toothkey". Archived from the original on 23 June 2018. Retrieved 23 June 2018.
- ^ Ribitzky G. "Forceps". Archived from the original on 23 June 2018. Retrieved 23 June 2018.
- ISBN 9780812219487.
Further reading
- "Tooth Extraction". American Dental Association. 6 September 2013. Archived from the original on 16 March 2020. Retrieved 30 August 2019.
{{cite web}}: CS1 maint: bot: original URL status unknown (link)

