Major depressive disorder
| Major depressive disorder | |
|---|---|
| Other names | Clinical depression, major depression, unipolar depression, unipolar disorder, recurrent depression |
antidepressant medication, electroconvulsive therapy, transcranial magnetic stimulation, exercise[1][7] | |
| Medication | Antidepressants |
| Frequency | 163 million (2017)[8] |
Major depressive disorder (MDD), also known as clinical depression, is a mental disorder[9] characterized by at least two weeks of pervasive low mood, low self-esteem, and loss of interest or pleasure in normally enjoyable activities. Introduced by a group of US clinicians in the mid-1970s,[10] the term was adopted by the American Psychiatric Association for this symptom cluster under mood disorders in the 1980 version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III), and has become widely used since.
The diagnosis of major depressive disorder is based on the person's reported experiences, behavior reported by relatives or friends, and a mental status examination.[11] There is no laboratory test for the disorder, but testing may be done to rule out physical conditions that can cause similar symptoms.[11] The most common time of onset is in a person's 20s,[3][4] with females affected about twice as often as males.[4] The course of the disorder varies widely, from one episode lasting months to a lifelong disorder with recurrent major depressive episodes.
Those with major depressive disorder are typically treated with
Major depressive disorder is believed to be caused by a combination of
Symptoms and signs
A person having a major depressive episode usually exhibits a low mood, which pervades all aspects of life, and an inability to experience pleasure in previously enjoyable activities.[15] Depressed people may be preoccupied with or ruminate over thoughts and feelings of worthlessness, inappropriate guilt or regret, helplessness or hopelessness.[16]
Other symptoms of depression include poor concentration and memory,[17] withdrawal from social situations and activities, reduced sex drive, irritability, and thoughts of death or suicide. Insomnia is common; in the typical pattern, a person wakes very early and cannot get back to sleep. Hypersomnia, or oversleeping, can also happen,[18] as well as day-night rhythm disturbances, such as diurnal mood variation.[19] Some antidepressants may also cause insomnia due to their stimulating effect.[20] In severe cases, depressed people may have psychotic symptoms. These symptoms include delusions or, less commonly, hallucinations, usually unpleasant.[21] People who have had previous episodes with psychotic symptoms are more likely to have them with future episodes.[22]
A depressed person may report multiple physical symptoms such as fatigue, headaches, or digestive problems; physical complaints are the most common presenting problem in developing countries, according to the World Health Organization's criteria for depression.[23] Appetite often decreases, resulting in weight loss, although increased appetite and weight gain occasionally occur.[24]
Major depression significantly affects a person's family and personal relationships, work or school life, sleeping and eating habits, and general health.[25] Family and friends may notice agitation or lethargy.[18] Older depressed people may have cognitive symptoms of recent onset, such as forgetfulness,[26] and a more noticeable slowing of movements.[27]
Depressed children may often display an irritable rather than a depressed mood;[18] most lose interest in school and show a steep decline in academic performance.[28] Diagnosis may be delayed or missed when symptoms are interpreted as "normal moodiness".[24] Elderly people may not present with classical depressive symptoms.[29] Diagnosis and treatment is further complicated in that the elderly are often simultaneously treated with a number of other drugs, and often have other concurrent diseases.[29]
Cause
The etiology of depression is not yet fully understood.
Genetics
Genes play a major role in the development of depression.[41] Family and twin studies find that nearly 40% of individual differences in risk for major depressive disorder can be explained by genetic factors.[42] Like most psychiatric disorders, major depressive disorder is likely influenced by many individual genetic changes.[43] In 2018, a genome-wide association study discovered 44 genetic variants linked to risk for major depression;[44] a 2019 study found 102 variants in the genome linked to depression.[45] However, it appears that major depression is less heritable compared to bipolar disorder and schizophrenia.[46][47] Research focusing on specific candidate genes has been criticized for its tendency to generate false positive findings.[48] There are also other efforts to examine interactions between life stress and polygenic risk for depression.[49]
Other health problems
Depression can also arise after a chronic or terminal medical condition, such as
Substance use in early age is associated with increased risk of developing depression later in life.[56] Depression occurring after giving birth is called postpartum depression and is thought to be the result of hormonal changes associated with pregnancy.[57] Seasonal affective disorder, a type of depression associated with seasonal changes in sunlight, is thought to be triggered by decreased sunlight.[58] Vitamin B2, B6 and B12 deficiency may cause depression in females.[59]
Environmental
Adverse childhood experiences (incorporating childhood abuse, neglect and family dysfunction) markedly increase the risk of major depression, especially if more than one type.[5] Childhood trauma also correlates with severity of depression, poor responsiveness to treatment and length of illness. Some are more susceptible than others to developing mental illness such as depression after trauma, and various genes have been suggested to control susceptibility.[60] Couples in unhappy marriages have a higher risk of developing clinical depression.[61]
There appears to be a link between
Pathophysiology
The pathophysiology of depression is not completely understood, but current theories center around
Derived from the effectiveness of monoaminergic drugs in treating depression, the monoamine theory posits that insufficient activity of
One proposed explanation for the therapeutic lag, and further support for the deficiency of monoamines, is a desensitization of self-inhibition in raphe nuclei by the increased serotonin mediated by antidepressants.[70] However, disinhibition of the dorsal raphe has been proposed to occur as a result of decreased serotonergic activity in tryptophan depletion, resulting in a depressed state mediated by increased serotonin. Further countering the monoamine hypothesis is the fact that rats with lesions of the dorsal raphe are not more depressive than controls, the finding of increased jugular 5-HIAA in people who are depressed that normalized with selective serotonin reuptake inhibitor (SSRI) treatment, and the preference for carbohydrates in people who are depressed.[71] Already limited, the monoamine hypothesis has been further oversimplified when presented to the general public.[72] A 2022 review found no consistent evidence supporting the serotonin hypothesis, linking serotonin levels and depression.[73]
Theories unifying neuroimaging findings have been proposed. The first model proposed is the limbic-cortical model, which involves hyperactivity of the ventral paralimbic regions and hypoactivity of frontal regulatory regions in emotional processing.[83] Another model, the cortico-striatal model, suggests that abnormalities of the prefrontal cortex in regulating striatal and subcortical structures result in depression.[84] Another model proposes hyperactivity of salience structures in identifying negative stimuli, and hypoactivity of cortical regulatory structures resulting in a negative emotional bias and depression, consistent with emotional bias studies.[85]
Diagnosis
Assessment
A diagnostic assessment may be conducted by a suitably trained
A doctor generally performs a medical examination and selected investigations to rule out other causes of depressive symptoms. These include blood tests measuring
DSM and ICD criteria
The most widely used criteria for diagnosing depressive conditions are found in the
Under mood disorders, ICD-11 classifies major depressive disorder as either single episode depressive disorder (where there is no history of depressive episodes, or of mania) or recurrent depressive disorder (where there is a history of prior episodes, with no history of mania).[106] ICD-11 symptoms, present nearly every day for at least two weeks, are a depressed mood or anhedonia, accompanied by other symptoms such as "difficulty concentrating, feelings of worthlessness or excessive or inappropriate guilt, hopelessness, recurrent thoughts of death or suicide, changes in appetite or sleep, psychomotor agitation or retardation, and reduced energy or fatigue."[106] These symptoms must affect work, social, or domestic activities. The ICD-11 system allows further specifiers for the current depressive episode: the severity (mild, moderate, severe, unspecified); the presence of psychotic symptoms (with or without psychotic symptoms); and the degree of remission if relevant (currently in partial remission, currently in full remission).[106] These two disorders are classified as "Depressive disorders", in the category of "Mood disorders".[106]
According to DSM-5, at least one of the symptoms is either depressed mood or loss of interest or pleasure. Depressed mood occurs nearly every day as subjective feelings like sadness, emptiness, and hopelessness or observations made by others (e.g. appears tearful). Loss of interest or pleasure occurs in all, or almost all activities of the day, nearly every day. These symptoms, as well as five out of the nine more specific symptoms listed, must frequently occur for more than two weeks (to the extent in which it impairs functioning) for the diagnosis
Major depressive episode
A major depressive episode is characterized by the presence of a severely depressed mood that persists for at least two weeks.[24] Episodes may be isolated or recurrent and are categorized as mild (few symptoms in excess of minimum criteria), moderate, or severe (marked impact on social or occupational functioning). An episode with psychotic features—commonly referred to as psychotic depression—is automatically rated as severe.[109] If the person has had an episode of mania or markedly elevated mood, a diagnosis of bipolar disorder is made instead. Depression without mania is sometimes referred to as unipolar because the mood remains at one emotional state or "pole".[111]
Subtypes
The DSM-5 recognizes six further subtypes of MDD, called specifiers, in addition to noting the length, severity and presence of psychotic features:
- "Melancholic depression" is characterized by a loss of pleasure in most or all activities, a failure of reactivity to pleasurable stimuli, a quality of depressed mood more pronounced than that of grief or loss, a worsening of symptoms in the morning hours, early-morning waking, psychomotor retardation, excessive weight loss (not to be confused with anorexia nervosa), or excessive guilt.[117]
- "Atypical depression" is characterized by mood reactivity (paradoxical anhedonia) and positivity, significant weight gain or increased appetite (comfort eating), excessive sleep or sleepiness (hypersomnia), a sensation of heaviness in limbs known as leaden paralysis, and significant long-term social impairment as a consequence of hypersensitivity to perceived interpersonal rejection.[118]
- "Catatonic depression" is a rare and severe form of major depression involving disturbances of motor behavior and other symptoms. Here, the person is mute and almost stuporous, and either remains immobile or exhibits purposeless or even bizarre movements. Catatonic symptoms also occur in schizophrenia or in manic episodes, or may be caused by neuroleptic malignant syndrome.[119]
- "Depression with anxious distress" was added into the DSM-5 as a means to emphasize the common co-occurrence between depression or mania and anxiety, as well as the risk of suicide of depressed individuals with anxiety. Specifying in such a way can also help with the prognosis of those diagnosed with a depressive or bipolar disorder.[109]
- "Depression with peri-partum onset" refers to the intense, sustained and sometimes disabling depression experienced by women after giving birth or while a woman is pregnant. DSM-IV-TR used the classification "postpartum depression", but this was changed to not exclude cases of depressed woman during pregnancy. Depression with peripartum onset has an incidence rate of 3–6% among new mothers. The DSM-5 mandates that to qualify as depression with peripartum onset, onset occurs during pregnancy or within one month of delivery.[120]
- "Seasonal affective disorder" (SAD) is a form of depression in which depressive episodes come on in the autumn or winter, and resolve in spring. The diagnosis is made if at least two episodes have occurred in colder months with none at other times, over a two-year period or longer.[121]
Differential diagnoses
To confirm major depressive disorder as the most likely diagnosis, other potential diagnoses must be considered, including dysthymia, adjustment disorder with depressed mood, or bipolar disorder. Dysthymia is a chronic, milder mood disturbance in which a person reports a low mood almost daily over a span of at least two years. The symptoms are not as severe as those for major depression, although people with dysthymia are vulnerable to secondary episodes of major depression (sometimes referred to as double depression).[112] Adjustment disorder with depressed mood is a mood disturbance appearing as a psychological response to an identifiable event or stressor, in which the resulting emotional or behavioral symptoms are significant but do not meet the criteria for a major depressive episode.[116]
Other disorders need to be ruled out before diagnosing major depressive disorder. They include depressions due to physical illness,
Screening and prevention
Preventive efforts may result in decreases in rates of the condition of between 22 and 38%.
Behavioral interventions, such as
The Netherlands mental health care system provides preventive interventions, such as the "Coping with Depression" course (CWD) for people with sub-threshold depression. The course is claimed to be the most successful of psychoeducational interventions for the treatment and prevention of depression (both for its adaptability to various populations and its results), with a risk reduction of 38% in major depression and an efficacy as a treatment comparing favorably to other psychotherapies.[128][131]
Management
The most common and effective treatments for depression are psychotherapy, medication, and electroconvulsive therapy (ECT); a combination of treatments is the most effective approach when depression is resistant to treatment.[132] American Psychiatric Association treatment guidelines recommend that initial treatment should be individually tailored based on factors including severity of symptoms, co-existing disorders, prior treatment experience, and personal preference. Options may include pharmacotherapy, psychotherapy, exercise, ECT, transcranial magnetic stimulation (TMS) or light therapy. Antidepressant medication is recommended as an initial treatment choice in people with mild, moderate, or severe major depression, and should be given to all people with severe depression unless ECT is planned.[133] There is evidence that collaborative care by a team of health care practitioners produces better results than routine single-practitioner care.[134]
Psychotherapy is the treatment of choice (over medication) for people under 18,
- People with a history of moderate or severe depression
- Those with mild depression that has been present for a long period
- As a second line treatment for mild depression that persists after other interventions
- As a first line treatment for moderate or severe depression.
The guidelines further note that antidepressant treatment should be continued for at least six months to reduce the risk of relapse, and that SSRIs are better tolerated than tricyclic antidepressants.[135]
Treatment options are more limited in developing countries, where access to mental health staff, medication, and psychotherapy is often difficult. Development of mental health services is minimal in many countries; depression is viewed as a phenomenon of the developed world despite evidence to the contrary, and not as an inherently life-threatening condition.[137] There is insufficient evidence to determine the effectiveness of psychological versus medical therapy in children.[138]
Lifestyle

Talking therapies
The most-studied form of psychotherapy for depression is CBT, which teaches clients to challenge self-defeating, but enduring ways of thinking (cognitions) and change counter-productive behaviors. CBT can perform as well as antidepressants in people with major depression.
Psychoanalysis is a school of thought, founded by Sigmund Freud, which emphasizes the resolution of unconscious mental conflicts.[162] Psychoanalytic techniques are used by some practitioners to treat clients presenting with major depression.[163] A more widely practiced therapy, called psychodynamic psychotherapy, is in the tradition of psychoanalysis but less intensive, meeting once or twice a week. It also tends to focus more on the person's immediate problems, and has an additional social and interpersonal focus.[164] In a meta-analysis of three controlled trials of Short Psychodynamic Supportive Psychotherapy, this modification was found to be as effective as medication for mild to moderate depression.[165]
Antidepressants

Conflicting results have arisen from studies that look at the effectiveness of antidepressants in people with acute, mild to moderate depression.[166] A review commissioned by the National Institute for Health and Care Excellence (UK) concluded that there is strong evidence that SSRIs, such as escitalopram, paroxetine, and sertraline, have greater efficacy than placebo on achieving a 50% reduction in depression scores in moderate and severe major depression, and that there is some evidence for a similar effect in mild depression.[167] Similarly, a Cochrane systematic review of clinical trials of the generic tricyclic antidepressant amitriptyline concluded that there is strong evidence that its efficacy is superior to placebo.[168] Antidepressants work less well for the elderly than for younger individuals with depression.[161]
To find the most effective antidepressant medication with minimal side-effects, the dosages can be adjusted, and if necessary, combinations of different classes of antidepressants can be tried. Response rates to the first antidepressant administered range from 50 to 75%, and it can take at least six to eight weeks from the start of medication to improvement.[133][169] Antidepressant medication treatment is usually continued for 16 to 20 weeks after remission, to minimize the chance of recurrence,[133] and even up to one year of continuation is recommended.[170] People with chronic depression may need to take medication indefinitely to avoid relapse.[25]
SSRIs are the primary medications prescribed, owing to their relatively mild side-effects, and because they are less toxic in overdose than other antidepressants.[171] People who do not respond to one SSRI can be switched to another antidepressant, and this results in improvement in almost 50% of cases.[172] Another option is to augment the atypical antidepressant bupropion to the SSRI as an adjunctive treatment.[173] Venlafaxine, an antidepressant with a different mechanism of action, may be modestly more effective than SSRIs.[174] However, venlafaxine is not recommended in the UK as a first-line treatment because of evidence suggesting its risks may outweigh benefits,[175] and it is specifically discouraged in children and adolescents as it increases the risk of suicidal thoughts or attempts.[176][177][178][179][180][181][182]
For children and adolescents with moderate-to-severe depressive disorder, fluoxetine seems to be the best treatment (either with or without cognitive behavioural therapy) but more research is needed to be certain.[183][177][184][178] Sertraline, escitalopram, duloxetine might also help in reducing symptoms. Some antidepressants have not been shown to be effective.[185][177] Medications are not recommended in children with mild disease.[186]
There is also insufficient evidence to determine effectiveness in those with depression complicated by dementia.[187] Any antidepressant can cause low blood sodium levels;[188] nevertheless, it has been reported more often with SSRIs.[171] It is not uncommon for SSRIs to cause or worsen insomnia; the sedating atypical antidepressant mirtazapine can be used in such cases.[189][190]
Irreversible monoamine oxidase inhibitors, an older class of antidepressants, have been plagued by potentially life-threatening dietary and drug interactions. They are still used only rarely, although newer and better-tolerated agents of this class have been developed.[191] The safety profile is different with reversible monoamine oxidase inhibitors, such as moclobemide, where the risk of serious dietary interactions is negligible and dietary restrictions are less strict.[192]
It is unclear whether antidepressants affect a person's risk of suicide.
Other medications and supplements
The combined use of antidepressants plus benzodiazepines demonstrates improved effectiveness when compared to antidepressants alone, but these effects may not endure. The addition of a benzodiazepine is balanced against possible harms and other alternative treatment strategies when antidepressant mono-therapy is considered inadequate.[201]
For treatment-resistant depression, adding on the
Ketamine may have a rapid antidepressant effect lasting less than two weeks; there is limited evidence of any effect after that, common acute side effects, and longer-term studies of safety and adverse effects are needed.[203][204] A nasal spray form of esketamine was approved by the FDA in March 2019 for use in treatment-resistant depression when combined with an oral antidepressant; risk of substance use disorder and concerns about its safety, serious adverse effects, tolerability, effect on suicidality, lack of information about dosage, whether the studies on it adequately represent broad populations, and escalating use of the product have been raised by an international panel of experts.[205][206]
There is insufficient high quality evidence to suggest
Electroconvulsive therapy
A usual course of ECT involves multiple administrations, typically given two or three times per week, until the person no longer has symptoms. ECT is administered under anesthesia with a muscle relaxant.[223] Electroconvulsive therapy can differ in its application in three ways: electrode placement, frequency of treatments, and the electrical waveform of the stimulus. These three forms of application have significant differences in both adverse side effects and symptom remission. After treatment, drug therapy is usually continued, and some people receive maintenance ECT.[217]
ECT appears to work in the short term via an
Other
There is a small amount of evidence that
The microbiome of people with major depressive disorder differs from that of healthy people, and probiotic and synbiotic treatment may achieve a modest depressive symptom reduction.[238][239]
Prognosis
Studies have shown that 80% of those with a first major depressive episode will have at least one more during their life,
A high proportion of people who experience full symptomatic remission still have at least one not fully resolved symptom after treatment.[246] Recurrence or chronicity is more likely if symptoms have not fully resolved with treatment.[246] Current guidelines recommend continuing antidepressants for four to six months after remission to prevent relapse. Evidence from many randomized controlled trials indicates continuing antidepressant medications after recovery can reduce the chance of relapse by 70% (41% on placebo vs. 18% on antidepressant). The preventive effect probably lasts for at least the first 36 months of use.[247]
Major depressive episodes often resolve over time, whether or not they are treated. Outpatients on a waiting list show a 10–15% reduction in symptoms within a few months, with approximately 20% no longer meeting the full criteria for a depressive disorder.[248] The median duration of an episode has been estimated to be 23 weeks, with the highest rate of recovery in the first three months.[249] According to a 2013 review, 23% of untreated adults with mild to moderate depression will remit within 3 months, 32% within 6 months and 53% within 12 months.[250]
Ability to work
Depression may affect people's ability to work. The combination of usual clinical care and support with return to work (like working less hours or changing tasks) probably reduces sick leave by 15%, and leads to fewer depressive symptoms and improved work capacity, reducing sick leave by an annual average of 25 days per year.[155] Helping depressed people return to work without a connection to clinical care has not been shown to have an effect on sick leave days. Additional psychological interventions (such as online cognitive behavioral therapy) lead to fewer sick days compared to standard management only. Streamlining care or adding specific providers for depression care may help to reduce sick leave.[155]
Life expectancy and the risk of suicide
Depressed individuals have a shorter life expectancy than those without depression, in part because people who are depressed are at risk of dying of suicide.[251] About 50% of people who die of suicide have a mood disorder such as major depression, and the risk is especially high if a person has a marked sense of hopelessness or has both depression and borderline personality disorder.[252][253] About 2–8% of adults with major depression die by suicide.[2][254] In the US, the lifetime risk of suicide associated with a diagnosis of major depression is estimated at 7% for men and 1% for women,[255] even though suicide attempts are more frequent in women.[256]
Depressed people also have a higher
Epidemiology

Major depressive disorder affected approximately 163 million people in 2017 (2% of the global population).[8] The percentage of people who are affected at one point in their life varies from 7% in Japan to 21% in France.[4] In most countries the number of people who have depression during their lives falls within an 8–18% range.[4]
In the United States, 8.4% of adults (21 million individuals) have at least one episode within a year-long period; the probability of having a major depressive episode is higher for females than males (10.5% to 6.2%), and highest for those aged 18 to 25 (17%).[261] Among adolescents between the ages of 12 and 17, 17% of the U.S. population (4.1 million individuals) had a major depressive episode in 2020 (females 25.2%, males 9.2%).[261] Among individuals reporting two or more races, the US prevalence is highest.[261]
Major depression is about twice as common in women as in men, although it is unclear why this is so, and whether factors unaccounted for are contributing to this.
People are most likely to develop their first depressive episode between the ages of 30 and 40, and there is a second, smaller peak of incidence between ages 50 and 60.[264] The risk of major depression is increased with neurological conditions such as stroke, Parkinson's disease, or multiple sclerosis, and during the first year after childbirth.[265] It is also more common after cardiovascular illnesses, and is related more to those with a poor cardiac disease outcome than to a better one.[266][267] Depressive disorders are more common in urban populations than in rural ones and the prevalence is increased in groups with poorer socioeconomic factors, e.g., homelessness.[268] Depression is common among those over 65 years of age and increases in frequency beyond this age.[29] The risk of depression increases in relation to the frailty of the individual.[269] Depression is one of the most important factors which negatively impact quality of life in adults, as well as the elderly.[29] Both symptoms and treatment among the elderly differ from those of the rest of the population.[29]
Major depression was the leading cause of disease burden in North America and other high-income countries, and the fourth-leading cause worldwide as of 2006. In the year 2030, it is predicted to be the second-leading cause of disease burden worldwide after HIV, according to the WHO.[270] Delay or failure in seeking treatment after relapse and the failure of health professionals to provide treatment are two barriers to reducing disability.[271]
Comorbidity
Major depression frequently
Depression and
History
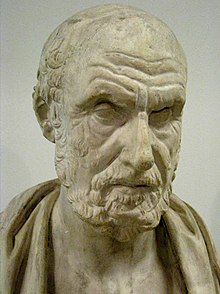
The Ancient Greek physician Hippocrates described a syndrome of melancholia (μελαγχολία, melankholía) as a distinct disease with particular mental and physical symptoms; he characterized all "fears and despondencies, if they last a long time" as being symptomatic of the ailment.[283] It was a similar but far broader concept than today's depression; prominence was given to a clustering of the symptoms of sadness, dejection, and despondency, and often fear, anger, delusions and obsessions were included.[284]
The term depression itself was derived from the Latin verb deprimere, meaning "to press down".
Although melancholia remained the dominant diagnostic term, depression gained increasing currency in medical treatises and was a synonym by the end of the century; German psychiatrist
The term unipolar (along with the related term bipolar) was coined by the neurologist and psychiatrist Karl Kleist, and subsequently used by his disciples Edda Neele and Karl Leonhard.[293]
The term Major depressive disorder was introduced by a group of US clinicians in the mid-1970s as part of proposals for diagnostic criteria based on patterns of symptoms (called the "Research Diagnostic Criteria", building on earlier
The new definitions of depression were widely accepted, albeit with some conflicting findings and views. There have been some continued empirically based arguments for a return to the diagnosis of melancholia.[296][297] There has been some criticism of the expansion of coverage of the diagnosis, related to the development and promotion of antidepressants and the biological model since the late 1950s.[298]
Society and culture
Terminology
The term "depression" is used in a number of different ways. It is often used to mean this syndrome but may refer to other mood disorders or simply to a low mood. People's conceptualizations of depression vary widely, both within and among cultures. "Because of the lack of scientific certainty," one commentator has observed, "the debate over depression turns on questions of language. What we call it—'disease,' 'disorder,' 'state of mind'—affects how we view, diagnose, and treat it."[300] There are cultural differences in the extent to which serious depression is considered an illness requiring personal professional treatment, or an indicator of something else, such as the need to address social or moral problems, the result of biological imbalances, or a reflection of individual differences in the understanding of distress that may reinforce feelings of powerlessness, and emotional struggle.[301][302]
Cultural dimension
Cultural differences contribute to different prevalence of symptoms. "Do the Chinese
Stigma
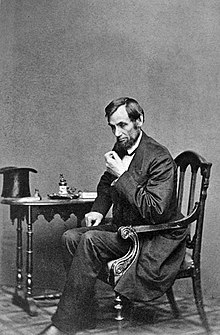
Historical figures were often reluctant to discuss or seek treatment for depression due to social stigma about the condition, or due to ignorance of diagnosis or treatments. Nevertheless, analysis or interpretation of letters, journals, artwork, writings, or statements of family and friends of some historical personalities has led to the presumption that they may have had some form of depression. People who may have had depression include English author Mary Shelley,[304] American-British writer Henry James,[305] and American president Abraham Lincoln.[306] Some well-known contemporary people with possible depression include Canadian songwriter Leonard Cohen[307] and American playwright and novelist Tennessee Williams.[308] Some pioneering psychologists, such as Americans William James[309][310] and John B. Watson,[311] dealt with their own depression.
There has been a continuing discussion of whether neurological disorders and mood disorders may be linked to creativity, a discussion that goes back to Aristotelian times.[312][313] British literature gives many examples of reflections on depression.[314] English philosopher John Stuart Mill experienced a several-months-long period of what he called "a dull state of nerves", when one is "unsusceptible to enjoyment or pleasurable excitement; one of those moods when what is pleasure at other times, becomes insipid or indifferent". He quoted English poet Samuel Taylor Coleridge's "Dejection" as a perfect description of his case: "A grief without a pang, void, dark and drear, / A drowsy, stifled, unimpassioned grief, / Which finds no natural outlet or relief / In word, or sigh, or tear."[315][316] English writer Samuel Johnson used the term "the black dog" in the 1780s to describe his own depression,[317] and it was subsequently popularized by British Prime Minister Sir Winston Churchill, who also had the disorder.[317] Johann Wolfgang von Goethe in his Faust, Part I, published in 1808, has Mephistopheles assume the form of a black dog, specifically a poodle.

Social stigma of major depression is widespread, and contact with mental health services reduces this only slightly. Public opinions on treatment differ markedly to those of health professionals; alternative treatments are held to be more helpful than pharmacological ones, which are viewed poorly.[318] In the UK, the Royal College of Psychiatrists and the Royal College of General Practitioners conducted a joint Five-year Defeat Depression campaign to educate and reduce stigma from 1992 to 1996;[319] a MORI study conducted afterwards showed a small positive change in public attitudes to depression and treatment.[320]
While serving his first term as Prime Minister of Norway, Kjell Magne Bondevik attracted international attention in August 1998 when he announced that he was suffering from a depressive episode, becoming the highest ranking world leader to admit to suffering from a mental illness while in office. Upon this revelation, Anne Enger became acting Prime Minister for three weeks, from 30 August to 23 September, while he recovered from the depressive episode. Bondevik then returned to office. Bondevik received thousands of supportive letters, and said that the experience had been positive overall, both for himself and because it made mental illness more publicly acceptable.[321][322]
References
- ^ a b c d e f g h i "Depression". U.S. National Institute of Mental Health (NIMH). May 2016. Archived from the original on 5 August 2016. Retrieved 31 July 2016.
- ^ ISBN 978-0-19-979704-2.
- ^ a b American Psychiatric Association 2013, p. 165.
- ^ PMID 23514317.
- ^ a b c d e f g American Psychiatric Association 2013, p. 166.
- ^ American Psychiatric Association 2013, pp. 167–168.
- ^ PMID 24026850.
- ^ PMID 30496104.
- ^ Sartorius N, Henderson AS, Strotzka H, et al. "The ICD-10 Classification of Mental and Behavioural Disorders Clinical descriptions and diagnostic guidelines" (PDF). World Health Organization. Archived from the original (PDF) on 5 February 2022. Retrieved 23 June 2021.
- ^ a b Spitzer RL, Endicott J, Robins E (1975). "The development of diagnostic criteria in psychiatry" (PDF). Archived (PDF) from the original on 14 December 2005. Retrieved 8 November 2008.
- ^ ISBN 978-1-118-92928-5.
- PMID 20051569.
- PMID 18303940.
- PMID 26063472.
- ^ American Psychiatric Association 2013, p. 160.
- ^ American_Psychiatric_Association 2013, p. 161.
- S2CID 253306482.
- ^ a b c American Psychiatric Association 2013, p. 163.
- PMID 17239958.
- ^ "Insomnia: Assessment and Management in Primary Care". American Family Physician. 59 (11): 3029–3038. 1999. Archived from the original on 26 July 2011. Retrieved 12 November 2014.
- ^ American Psychiatric Association 2000a, p. 412
- S2CID 43951278.
- PMID 11222428.
- ^ a b c American Psychiatric Association 2000a, p. 349
- ^ a b c d e Depression (PDF). National Institute of Mental Health (NIMH). Archived (PDF) from the original on 28 August 2021. Retrieved 13 October 2021.
- ^ Delgado PL, Schillerstrom J (2009). "Cognitive Difficulties Associated With Depression: What Are the Implications for Treatment?". Psychiatric Times. 26 (3). Archived from the original on 22 July 2009.
- ISBN 978-0-7347-3341-2. Archived(PDF) from the original on 1 April 2015.
- ^ American Psychiatric Association 2013, p. 164.
- ^ a b c d e "Depression treatment for the elderly". Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU). 27 January 2015. Archived from the original on 18 June 2016. Retrieved 16 June 2016.
- ISBN 978-1-4129-0490-2.
- S2CID 4047310.
Despite advances in our understanding of the neuro-biology of MDD, no established mechanism can explain all aspects of the disease.
- OCLC 1264172789.
Although there is no single unifying theory, several theories have emerged over the last century that attempt to account for the various clinical, psychological, and biologic findings in depression.
- OCLC 1260160457.
A number of risk factors for depression are known or suspected, but only in rare cases is the link to disease strong.
- OCLC 843944119.
Although genes are an important cause of major depression and bipolar disorder, we have not confirmed the identity of the responsible genes.
- ^ Department of Health and Human Services (1999). "The fundamentals of mental health and mental illness" (PDF). Mental Health: A Report of the Surgeon General. Archived (PDF) from the original on 17 December 2008. Retrieved 11 November 2008.
- S2CID 146500484.
- (PDF) from the original on 17 December 2008.
- ^ Slavich GM (2004). "Deconstructing depression: A diathesis-stress perspective (Opinion)". APS Observer. Archived from the original on 11 May 2011. Retrieved 11 November 2008.
- ISBN 0-89862-000-7. Retrieved 26 February 2022.
- S2CID 226243519.
- OCLC 982958263.
Depression is highly heritable, as youths with a parent with a history of depression are approximately 4 times as likely to develop the disorder as youths who do not have a parent with depression.
- PMID 11007705.
- S2CID 12566638.
It is clear from studies of families that major depression is not caused by any single gene but is a disease with complex genetic features.
- PMID 29700475.
- PMID 30718901.
- PMID 11007705.
The heritability of major depression is likely to be in the range of 31%–42%. This is probably the lower bound, and the level of heritability is likely to be substantially higher for reliably diagnosed major depression or for subtypes such as recurrent major depression. In comparison, the heritabilities of schizophrenia and bipolar disorder are estimated to be approximately 70%.
- OCLC 1138027525.
Thus it appears that bipolar disorder is more strongly influenced by genetic factors than is major depressive disorder.
- PMID 21890791.
- PMID 29129318.
- PMID 11694462.
- PMID 6455456.
- PMID 19180246.
- PMID 19724774.
- ^ Botts S, Ryan M. Drug-Induced Diseases Section IV: Drug-Induced Psychiatric Diseases Chapter 18: Depression. pp. 1–23. Archived from the original on 23 December 2010.
- PMID 25922673.
- PMID 12418937.
- PMID 21485749.
- PMID 26688752.
- PMID 33912967.
- PMID 22370490.
- PMID 3826462.
- PMID 31850801.
- PMID 17389902.
- PMID 10703757.
- PMID 22691454.
- PMID 20975857.
- S2CID 26550661.
- PMID 17088501.
- ISBN 978-0-7817-2837-9.
- PMID 25825168.
- S2CID 23980182.
- PMID 16268734.
- S2CID 250646781. Lay source Medicalxpress
- PMID 22423117.
- PMID 23995180.
- S2CID 230209.
- (PDF) from the original on 20 July 2018.
- S2CID 24215407.
- PMID 3000317.
- PMID 15014598.
- PMID 19406581.
- PMID 25999722.
- PMID 9276848.
- PMID 23890584.
- PMID 22535198.
- PMID 8219844.
- ^ "Call for action over Third World depression". BBC News (Health). British Broadcasting Corporation (BBC). 1 November 1999. Archived from the original on 13 May 2008. Retrieved 11 October 2008.
- PMID 12358212.
- S2CID 24291799.
- PMID 20100303.
- S2CID 11477277.
- PMID 17968628.
- S2CID 72755878.
- PMID 15508552.
- ^ PMID 27750060.
- S2CID 9328852.
- PMID 9720486.
- S2CID 33714179.
- ^ Sadock 2002, p. 108
- ^ Sadock 2002, p. 260
- ^ Sadock 2002, p. 288
- ^ American Psychiatric Association 2013, p. xii.
- ^ ISBN 978-3-527-61967-2. Archived(PDF) from the original on 3 May 2005. Retrieved 30 October 2008.
- ^ "Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR)". American Psychiatric Association. Retrieved 9 July 2022.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) features the most current text updates based on scientific literature with contributions from more than 200 subject matter experts.
- ^ "International Statistical Classification of Diseases and Related Health Problems (ICD)". World Health Organization. Retrieved 9 July 2022.
... the latest version of the ICD, ICD-11, was adopted by the 72nd World Health Assembly in 2019 and came into effect on 1st January 2022.
- ^ a b c d ICD-11, 6A70 Single episode depressive disorder and 6A71 Recurrent depressive disorder
- ISBN 978-0-89042-554-1.
- ^ "Diagnostic Criteria for Major Depressive Disorder and Depressive Episodes" (PDF). City of Palo Alto Project Safety Net. Archived from the original (PDF) on 3 August 2020. Retrieved 21 February 2019.
- ^ PMID 24986345.
- ^ American Psychiatric Association 2013, p. 162
- ^ Parker 1996, p. 173
- ^ a b Sadock 2002, p. 552
- ^ American Psychiatric Association 2013, p. 183.
- S2CID 26860606.
- PMID 11925303.
- ^ a b American Psychiatric Association 2013, p. 168.
- ^ American Psychiatric Association 2013, p. 185.
- ^ American Psychiatric Association 2013, pp. 185–186.
- ^ American Psychiatric Association 2013, pp. 119–120.
- ^ American Psychiatric Association 2013, pp. 186–187.
- ^ American Psychiatric Association 2013, p. 187.
- ^ American_Psychiatric_Association 2013, p. 167.
- ^ PMID 18765483.
- PMID 26813211.
- PMID 26858097.
- PMID 16235301.
- S2CID 104296515.
- ^ PMID 22583342.
- ^ Cuijpers P (20 September 2012). Prevention and early treatment of mental ill-health (PDF). Psychology for Health: Contributions to Policy Making, Brussels. Archived from the original (PDF) on 12 May 2013. Retrieved 16 June 2013.
- (PDF) from the original on 12 November 2014. Retrieved 12 November 2014.
- PMID 19450912.
- PMID 34877271.
- ^
- PMID 23076925.
- ^ a b c "Depression". National Institute for Health and Care Excellence. December 2004. Archived from the original on 15 November 2008. Retrieved 20 March 2013.
- PMID 27501438.
- S2CID 73073889.
- PMID 25433518.
- S2CID 29351791.
- PMID 22945926.
- (PDF) from the original on 9 January 2017.
- PMID 24524926.
- PMID 22860015.
- S2CID 45091134.
- ISBN 978-1-4020-8264-1.
- PMID 29761488.
- PMID 18254062.
- S2CID 14778731.
- PMID 28615268.
- ^ Childhood Depression. abct.org. Last updated: 30 July 2010
- ISBN 978-1-84629-074-9. Archivedfrom the original on 24 September 2008. Retrieved 16 August 2008.
- ^ Becker SJ (2008). "Cognitive-Behavioral Therapy for Adolescent Depression: Processes of Cognitive Change". Psychiatric Times. 25 (14).
- PMID 15328551.
- PMID 16787553.
- ^ PMID 33052607.
- ^ Beck et al. 1987, p. 10.
- PMID 18085916.
- PMID 23796855.
- PMID 25591492.
- PMID 24975623.
- ^ PMID 31383842.
- ISBN 978-0-314-20412-7.
- S2CID 25110425.
- ^ Barlow & Durand 2005, p. 20.
- S2CID 20373635.
- PMID 28985309.
- NICE. October 2009. Archivedfrom the original on 12 November 2014. Retrieved 12 November 2014.
- PMID 23235671.
- PMID 29952277.
- S2CID 2347144.
- ^ a b Royal Pharmaceutical Society of Great Britain 2008, p. 204
- PMID 11136266.
- S2CID 20997303.
- S2CID 45621773.
- ^ Duff G (31 May 2006). "Updated prescribing advice for venlafaxine (Efexor/Efexor XL)". Medicines and Healthcare products Regulatory Agency (MHRA). Archived from the original on 13 November 2008.
- S2CID 253347210.
- ^ PMID 32563306.
- ^ PMID 34029378.
- PMID 32394557.
- PMID 32982805.
- PMID 34002501.
- ^ "Depression in children and young people: Identification and management in primary, community and secondary care". NICE Clinical Guidelines (28). NHS National Institute for Health and Clinical Excellence. 2005. Archived from the original on 12 November 2014. Retrieved 12 November 2014.
- S2CID 242952585.
- PMID 32982805.
- S2CID 19728203.
- PMID 29483201.
- S2CID 2592434.
- S2CID 37965495.
- PMID 17636748.
- PMID 10760555.
- PMID 17640156.
- PMID 12595913.
- S2CID 40682753.
- ^ Hammad TA (16 August 2004). "Review and evaluation of clinical data. Relationship between psychiatric drugs and pediatric suicidality" (PDF). FDA. pp. 42, 115. Archived (PDF) from the original on 25 June 2008. Retrieved 29 May 2008.
- PMID 23152227.
- PMID 15718537.
- PMID 15718539.
- PMID 19671933.
- FDA. 2 May 2007. Archivedfrom the original on 23 February 2008. Retrieved 29 May 2008.
- Medics and Foods Department. Pharmaceuticals and Medical Devices Safety Information (PDF) (Report). 261 (in Japanese). Ministry of Health, Labour and Welfare (Japan). Archived from the original(PDF) on 29 April 2011. Retrieved 19 May 2010.
- PMID 31158298.
- ^ PMC 10406422.
- PMID 31695324.
- PMID 30844397.
- S2CID 232262694.
- PMID 31160868.
- PMID 34817851.
- PMID 23814104.
- ISBN 978-0-07-803538-8.
- ^ Gelenberg AJ, Freeman MP, Markowitz JC. "Practice Guideline for the Treatment of Patients with Major Depressive Disorder" (PDF) (3rd ed.). American Psychiatric Association (APA). Retrieved 3 November 2014.
- PMID 25295426.
- S2CID 45341424.
- PMID 12804463.
- PMID 30427999.
- ^ Rudorfer, MV, Henry, ME, Sackeim, HA (2003). "Electroconvulsive therapy". In A Tasman, J Kay, JA Lieberman (eds) Psychiatry, Second Edition. Chichester: John Wiley & Sons Ltd, 1865–1901.
- S2CID 36643014.
- ^ a b c FDA. FDA Executive Summary Archived 24 September 2015 at the Wayback Machine. Prepared for the 27–28 January 2011 meeting of the Neurological Devices Panel Meeting to Discuss the Classification of Electroconvulsive Therapy Devices (ECT). Quote, p38: "Three major practice guidelines have been published on ECT. These guidelines include: APA Task Force on ECT (2001); Third report of the Royal College of Psychiatrists' Special Committee on ECT (2004); National Institute for Health and Clinical Excellence (NICE 2003; NICE 2009). There is significant agreement between the three sets of recommendations."
- S2CID 44280002.
- PMID 23774532.
- ^ Surgeon General (1999). Mental Health: A Report of the Surgeon General Archived 12 January 2007 at the Wayback Machine, chapter 4.
- ISBN 978-0-89042-206-9.
- S2CID 31209001.
- ^ "5 Outdated Beliefs About ECT". Psych Central.com. 17 May 2016. Archived from the original on 8 August 2013.
- PMID 24381234.
- ^ "NiCE. January 2014 Transcranial magnetic stimulation for treating and preventing migraine". Archived from the original on 4 October 2015.
- ^ Melkerson MN (16 December 2008). "Special Premarket 510(k) Notification for NeuroStar® TMS Therapy System for Major Depressive Disorder" (PDF). Food and Drug Administration. Archived (PDF) from the original on 31 March 2010. Retrieved 16 July 2010.
- (PDF) from the original on 23 July 2022.
- ^ Gelenberg AJ, Freeman MP, Markowitz JC, Rosenbaum JF, Thase ME, Trivedi MH, Van Rhoads RS, eds. (2010). "Practice Guidelines for the Treatment of Patients with Major Depressive Disorder" (PDF) (3rd ed.). American Psychiatric Association.
- PMID 19682750. Archived from the original(PDF) on 23 August 2015.
- S2CID 22066326.
- PMID 32710772.
- S2CID 209373871.
- PMID 33145770.
- PMID 12531127.
- PMID 25835541.
- PMID 25695871.
- PMID 31672337.
- PMID 32056863.
- PMID 35562885.
- S2CID 22808803.
- PMID 17555914.
- PMID 18458203.
- PMID 18251627.
- S2CID 10490348.
- ^ "Depression, Major: Prognosis". MDGuidelines. The Guardian Life Insurance Company of America. Archived from the original on 20 April 2010. Retrieved 16 July 2010.
- ^ PMID 26337210.
- S2CID 20198748.
- PMID 11578666.
- S2CID 22891687.
- S2CID 11068930.
- PMID 12377293.
- ^ Barlow & Durand 2005, pp. 248–49.
- PMID 29986446.
Half of all completed suicides are related to depressive and other mood disorders
- ISBN 978-0-19-026432-1.
- S2CID 36975913.
- PMID 17202555.
- PMID 17640152.
- PMID 21208573.
- ^ Schulman J, Shapiro BA (2008). "Depression and Cardiovascular Disease: What Is the Correlation?". Psychiatric Times. 25 (9). Archived from the original on 6 March 2020. Retrieved 10 June 2009.
- ^ "WHO Disease and injury country estimates". World Health Organization. 2009. Archived from the original on 11 November 2009. Retrieved 11 November 2009.
- ^ a b c "Major depression". U.S. National Institute of Mental Health (NIMH). January 2022. Archived from the original on 9 August 2022. Retrieved 14 August 2022.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ^ S2CID 19538251.
- ^ Institute for Health Metrics and Evaluation (2020), Global Burden of Disease 2019 Cause and Risk Summary: Major depressive disorder — Level 4 cause, Seattle, US: University of Washington, Table 3, retrieved 9 July 2022
- PMID 9366655.
- PMID 15718222.
- S2CID 11051637.
- S2CID 45722423.
- ^ Gelder, M, Mayou, R and Geddes, J (2005). Psychiatry. 3rd ed. New York: Oxford. p. 105.
- S2CID 205668529.
- PMID 17132052.
- PMID 18674396.
- S2CID 19525295.
- PMID 15014592.
- PMID 8838629.
- PMID 21382111.
- ISBN 978-0-345-44231-4.
- ^ Brunsvold GL, Oepen G (2008). "Comorbid Depression in ADHD: Children and Adolescents". Psychiatric Times. 25 (10). Archived from the original on 24 May 2009.
- PMID 11874213.
- PMID 29093037.
- S2CID 205642153.
- PMID 14609780.
- ^ Yohannes AM, Baldwin RC (2008). "Medical Comorbidities in Late-Life Depression". Psychiatric Times. 25 (14). Archived from the original on 14 June 2020. Retrieved 10 June 2009.
- ^ Hippocrates, Aphorisms, Section 6.23
- ^ S2CID 143684460.
- ^ "Definition of depress | Dictionary.com". www.dictionary.com. Retrieved 14 August 2022.
- ^ Wolpert L (1999). "Malignant Sadness: The Anatomy of Depression". The New York Times. Archived from the original on 9 April 2009. Retrieved 30 October 2008.
- S2CID 145445990.
- .
- PMID 18652673.
- ISBN 978-0-14-021740-7.
- .
- doi:10.1176/appi.books.9780890420355.dsm-ii (inactive 31 January 2024).)
{{cite book}}: CS1 maint: DOI inactive as of January 2024 (link - ^ Angst J. Terminology, history and definition of bipolar spectrum. In: Maj M, Akiskal HS, López-Ibor JJ, Sartorius N (eds.), Bipolar disorders. Chichester: Wiley & Sons, LTD; 2002. pp. 53–55.
- ^ S2CID 36768744.
- ^ ISBN 978-0-470-17356-5.
- S2CID 221452354.
- PMID 17244171.
- ISBN 978-0-674-03958-2.
- ^ Wolf, Joshua "Lincoln's Great Depression" Archived 9 October 2011 at the Wayback Machine, The Atlantic, October 2005. Retrieved 10 October 2009
- ^ Maloney F (3 November 2005). "The Depression Wars: Would Honest Abe Have Written the Gettysburg Address on Prozac?". Slate. Archived from the original on 25 September 2008. Retrieved 3 October 2008.
- PMID 15652693.
- S2CID 145545714.
- S2CID 24932164.
- ISBN 978-0-8021-3948-1.
- PBS. Archived from the originalon 8 October 2008. Retrieved 19 August 2008.
- ISBN 978-0-252-06667-2.
- ^ Pita E (26 September 2001). "An Intimate Conversation with...Leonard Cohen". Archived from the original on 11 October 2008. Retrieved 3 October 2008.
- PMID 15249274.
- ISBN 978-0-7661-7566-2.
- ^ Hergenhahn 2005, p. 311
- ISBN 978-0-7100-0054-5.
- PMID 18689294.
- ^ Simonton DK (2005). "Are genius and madness related? Contemporary answers to an ancient question". Psychiatric Times. 22 (7). Archived from the original on 14 January 2009.
- ISBN 978-0-8207-0262-9.
- ISBN 978-1-4212-4200-2. Archivedfrom the original on 21 September 2008. Retrieved 9 August 2008.
- ^ Sterba R (1947). "The 'Mental Crisis' of John Stuart Mill". Psychoanalytic Quarterly. 16 (2): 271–72. Archived from the original on 12 January 2009. Retrieved 5 November 2008.
- ^ a b "Churchill's Black Dog?: The History of the 'Black Dog' as a Metaphor for Depression" (PDF). Black Dog Institute website. Black Dog Institute. 2005. Archived from the original (PDF) on 10 September 2008. Retrieved 18 August 2008.
- ISBN 978-0-521-66229-1.
- PMID 9167546.
- S2CID 21172113.
- PMID 22271941. Archived from the originalon 31 October 2013. Retrieved 19 July 2013.
- ^ BBC Newsnight, 21 January 2008.
Cited works
- American Psychiatric Association (2000a). Diagnostic and statistical manual of mental disorders (Fourth Edition, Text Revision: DSM-IV-TR ed.). Washington, DC: American Psychiatric Publishing, Inc. ISBN 978-0-89042-025-6.
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (Fifth Edition: DSM-5 ed.). Washington, DC: American Psychiatric Publishing, Inc. ISBN 978-0-89042-555-8.
- Barlow DH, Durand VM (2005). Abnormal psychology: An integrative approach (5th ed.). Belmont, CA: Thomson Wadsworth. ISBN 978-0-534-63356-1.
- Beck AT, Rush J, Shaw BF, Emery G (1987) [1979]. Cognitive therapy of depression. New York: Guilford Press. ISBN 978-0-89862-919-4.
- Hergenhahn BR (2005). An Introduction to the History of Psychology (5th ed.). Belmont, CA: Thomson Wadsworth. ISBN 978-0-534-55401-9.
- Parker G, Hadzi-Pavlovic D, eds. (1996). Melancholia: a disorder of movement and mood: a phenomenological and neurobiological review. Cambridge: Cambridge University Press. ISBN 978-0-521-47275-3.
- Royal Pharmaceutical Society of Great Britain (2008). British National Formulary (BNF 56). UK: BMJ Group and RPS Publishing. ISBN 978-0-85369-778-7.
- Sadock VA, Sadock BJ, Kaplan HI (2003). Kaplan & Sadock's synopsis of psychiatry: behavioral sciences/clinical psychiatry. Philadelphia: Lippincott Williams & Wilkins. ISBN 978-0-7817-3183-6.
- "6A70 Single episode depressive disorder". International Classification of Diseases 11th Revision. World Health Organization. February 2022 [adopted in 2019]. Retrieved 9 July 2022.
- "6A71 Recurrent depressive disorder". International Classification of Diseases 11th Revision. World Health Organization. February 2022 [adopted in 2019]. Retrieved 9 July 2022.
