Diarrhea
| Diarrhea | |
|---|---|
| Other names | Diarrhoea (or diarrhœa) |
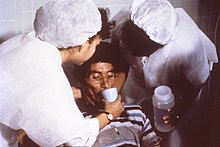
zinc supplementation[2] | |
| Frequency | ≈2.4 billion (2015)[3] |
| Deaths | 1.53 million (2019)[4] |
Diarrhea (American English), also spelled diarrhoea or diarrhœa (British English), is the condition of having at least three loose, liquid, or watery bowel movements in a day.[2] It often lasts for a few days and can result in dehydration due to fluid loss.[2] Signs of dehydration often begin with loss of the normal stretchiness of the skin and irritable behaviour.[2] This can progress to decreased urination, loss of skin color, a fast heart rate, and a decrease in responsiveness as it becomes more severe.[2] Loose but non-watery stools in babies who are exclusively breastfed, however, are normal.[2]

The most common cause is an infection of the
Diarrhea can be prevented by improved
About 1.7 to 5 billion cases of diarrhea occur per year.
Terminology
The word diarrhea is from the Ancient Greek διάρροια from διά dia "through" and ῥέω rheo "flow".
Diarrhea is the spelling in American English, whereas diarrhoea is the spelling in British English.
Slang terms for the condition include "the runs", "the squirts" (or "squits" in Britain[13]) and "the trots".[14][15]
The word is often pronounced as /ˌdaɪəˈriːə/ DY-ə-REE-ə.
Definition
Diarrhea is defined by the World Health Organization as having three or more loose or liquid stools per day, or as having more stools than is normal for that person.[2]
Acute diarrhea is defined as an abnormally frequent discharge of semisolid or fluid fecal matter from the bowel, lasting less than 14 days, by World Gastroenterology Organization.[16] Acute diarrhea that is watery may be known as AWD (Acute Watery Diarrhoea.)[17]
Secretory
Secretory diarrhea means that there is an increase in the active secretion, or there is an inhibition of absorption. There is little to no structural damage. The most common cause of this type of diarrhea is a
Osmotic
Osmotic diarrhea occurs when too much water is drawn into the bowels. If a person drinks solutions with excessive sugar or excessive salt, these can draw water from the body into the bowel and cause osmotic diarrhea.
Exudative
Exudative diarrhea occurs with the presence of blood and pus in the stool. This occurs with
Inflammatory
Inflammatory diarrhea occurs when there is damage to the mucosal lining or brush border, which leads to a passive loss of protein-rich fluids and a decreased ability to absorb these lost fluids. Features of all three of the other types of diarrhea can be found in this type of diarrhea.[21] It can be caused by bacterial infections, viral infections, parasitic infections, or autoimmune problems such as inflammatory bowel diseases. It can also be caused by tuberculosis, colon cancer, and enteritis.[19]
Dysentery
If there is blood visible in the stools, it is also known as dysentery. The blood is a trace of an invasion of bowel tissue. Dysentery is a symptom of, among others, Shigella, Entamoeba histolytica, and Salmonella.[19]
Health effects
Diarrheal disease may have a negative impact on both physical fitness and mental development. "Early childhood malnutrition resulting from any cause reduces physical fitness and work productivity in adults,"
Diarrhea can cause
Causes
In the latter stages of human digestion, ingested materials are inundated with water and digestive fluids such as gastric acid, bile, and digestive enzymes in order to break them down into their nutrient components, which are then absorbed into the bloodstream via the intestinal tract in the small intestine. Prior to defecation, the large intestine reabsorbs the water and other digestive solvents in the waste product in order to maintain proper hydration and overall equilibrium.[25] Diarrhea occurs when the large intestine is prevented, for any number of reasons, from sufficiently absorbing the water or other digestive fluids from fecal matter, resulting in a liquid, or "loose", bowel movement.[26]
Chronic diarrhea can be the part of the presentations of a number of chronic medical conditions affecting the intestine. Common causes include
Infections
There are many causes of infectious diarrhea, which include
Campylobacter spp. are a common cause of bacterial diarrhea, but infections by Salmonella spp., Shigella spp. and some strains of Escherichia coli are also a frequent cause.[36]
In the elderly, particularly those who have been treated with antibiotics for unrelated infections, a toxin produced by
Parasites, particularly protozoa e.g., Cryptosporidium spp., Giardia spp., Entamoeba histolytica, Blastocystis spp., Cyclospora cayetanensis, are frequently the cause of diarrhea that involves chronic infection. The broad-spectrum antiparasitic agent nitazoxanide has shown efficacy against many diarrhea-causing parasites.[38]
Other infectious agents, such as
Sanitation

Open defecation is a leading cause of infectious diarrhea leading to death.[40]
Poverty is a good indicator of the rate of infectious diarrhea in a population. This association does not stem from poverty itself, but rather from the conditions under which impoverished people live. The absence of certain resources compromises the ability of the poor to defend themselves against infectious diarrhea. "Poverty is associated with poor housing, crowding, dirt floors, lack of access to clean water or to sanitary disposal of fecal waste (sanitation), cohabitation with domestic animals that may carry human pathogens, and a lack of refrigerated storage for food, all of which increase the frequency of diarrhea ... Poverty also restricts the ability to provide age-appropriate, nutritionally balanced diets or to modify diets when diarrhea develops so as to mitigate and repair nutrient losses. The impact is exacerbated by the lack of adequate, available, and affordable medical care."[41]
One of the most common causes of infectious diarrhea is a lack of clean water. Often, improper fecal disposal leads to contamination of groundwater. This can lead to widespread infection among a population, especially in the absence of water filtration or purification. Human feces contains a variety of potentially harmful human
Nutrition
Proper nutrition is important for health and functioning, including the prevention of infectious diarrhea. It is especially important to young children who do not have a fully developed immune system.
Malabsorption
Malabsorption is the inability to absorb food fully, mostly from disorders in the small bowel, but also due to maldigestion from diseases of the pancreas.
Causes include:[citation needed]
- enzyme deficiencies or mucosal abnormality, as in celiac disease (gluten intolerance), lactose intolerance (intolerance to milk sugar, common in non-Europeans), and fructose malabsorption.
- pernicious anemia, or impaired bowel function due to the inability to absorb vitamin B12,
- loss of pancreatic secretions, which may be due to cystic fibrosis or pancreatitis,
- structural defects, like short bowel syndrome (surgically removed bowel) and radiation fibrosis, such as usually follows cancer treatment and other drugs, including agents used in chemotherapy; and
- certain drugs, like orlistat, which inhibits the absorption of fat.
Inflammatory bowel disease
The two overlapping types here are of unknown origin:
- colon near the rectum.
- Crohn's disease typically affects fairly well demarcated segments of bowel in the colon and often affects the end of the small bowel.
Irritable bowel syndrome
Another possible cause of diarrhea is irritable bowel syndrome (IBS), which usually presents with abdominal discomfort relieved by defecation and unusual stool (diarrhea or constipation) for at least three days a week over the previous three months.[49] Symptoms of diarrhea-predominant IBS can be managed through a combination of dietary changes, soluble fiber supplements and medications such as loperamide or codeine. About 30% of patients with diarrhea-predominant IBS have bile acid malabsorption diagnosed with an abnormal SeHCAT test.[50]
Other diseases
Diarrhea can be caused by other diseases and conditions, namely:
- Chronic ethanol ingestion[51]
- Hyperthyroidism[52]
- Certain medications[52]
- Bile acid malabsorption[52]
- Ischemic bowel disease: This usually affects older people and can be due to blocked arteries.
- Microscopic colitis, a type of inflammatory bowel disease where changes are seen only on histological examination of colonic biopsies.
- colonproduce a secretory diarrhea.
- Hormone-secreting tumors: some hormones, e.g. serotonin, can cause diarrhea if secreted in excess (usually from a tumor).
- Chronic mild diarrhea in infants and toddlers may occur with no obvious cause and with no other ill effects; this condition is called toddler's diarrhea.
- Environmental enteropathy
- Radiation enteropathy following treatment for pelvic and abdominal cancers.
Medications
Over 700 medications, such as penicillin, are known to cause diarrhea.[53][54] The classes of medications that are known to cause diarrhea are laxatives, antacids, heartburn medications, antibiotics, anti-neoplastic drugs, anti-inflammatories as well as many dietary supplements.[19]
Pathophysiology
| Function | Transporter |
|---|---|
| Absorption | DRA
|
| Secretion | CFTR
|
| Absorption and secretion | Sodium potassium ATPase
|
Evolution
According to two researchers,
Diagnostic approach
The following types of diarrhea may indicate further investigation is needed:
- In infants
- Moderate or severe diarrhea in young children
- Associated with blood
- Continues for more than two days
- Associated non-cramping abdominal pain, fever, weight loss, etc.
- In travelers
- In food handlers, because of the potential to infect others;
- In institutions such as hospitals, child care centers, or geriatric and convalescent homes.
A severity score is used to aid diagnosis in children.[58]
When diarrhea lasts for more than four weeks a number of further tests may be recommended including:[59]
- Complete blood count and a ferritin if anemia is present
- Thyroid stimulating hormone
- celiac disease
- Fecal calprotectin to exclude inflammatory bowel disease
- Clostridioides difficile
- A colonoscopy or fecal immunochemical testing for cancer, including biopsies to detect microscopic colitis
- Testing for bile acidsdepending on availability
- Hydrogen breath test looking for lactose intolerance
- Further tests if pelvic radiation disease or small intestinal bacterial overgrowthsuspected.
A 2019 guideline recommended that testing for ova and parasites was only needed in people who are at high risk though they recommend routine testing for giardia.[60] Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) were not recommended.[60]
Epidemiology


Worldwide in 2004, approximately 2.5 billion cases of diarrhea occurred, which resulted in 1.5 million deaths among children under the age of five.[1] Greater than half of these were in Africa and South Asia.[1] This is down from a death rate of 4.5 million in 1980 for gastroenteritis.[62] Diarrhea remains the second leading cause of infant mortality (16%) after pneumonia (17%) in this age group.[1]
The majority of such cases occur in the developing world, with over half of the recorded cases of childhood diarrhea occurring in Africa and Asia, with 696 million and 1.2 billion cases, respectively, compared to only 480 million in the rest of the world.[63]
Infectious diarrhea resulted in about 0.7 million deaths in children under five years old in 2011 and 250 million lost school days.[64][65] In the Americas, diarrheal disease accounts for a total of 10% of deaths among children aged 1–59 months while in South East Asia, it accounts for 31.3% of deaths.[66] It is estimated that around 21% of child mortalities in developing countries are due to diarrheal disease.[67]
Prevention
Sanitation
Numerous studies have shown that improvements in drinking water and sanitation (WASH) lead to decreased risks of diarrhoea.[68] Such improvements might include for example use of water filters, provision of high-quality piped water and sewer connections.[68]
In institutions, communities, and households, interventions that promote hand washing with soap lead to significant reductions in the incidence of diarrhea.[69] The same applies to preventing open defecation at a community-wide level and providing access to improved sanitation.[64][70] This includes use of toilets and implementation of the entire sanitation chain connected to the toilets (collection, transport, disposal or reuse of human excreta).
There is limited evidence that safe disposal of child or adult feces can prevent diarrheal disease.[71][72]
Hand washing
Basic sanitation techniques can have a profound effect on the transmission of diarrheal disease. The implementation of hand washing using soap and water, for example, has been experimentally shown to reduce the incidence of disease by approximately 30–48%.[73][74][69] Hand washing in developing countries, however, is compromised by poverty as acknowledged by the CDC: "Handwashing is integral to disease prevention in all parts of the world; however, access to soap and water is limited in a number of less developed countries. This lack of access is one of many challenges to proper hygiene in less developed countries." Solutions to this barrier require the implementation of educational programs that encourage sanitary behaviours.[75]
Water
Given that water contamination is a major means of transmitting diarrheal disease, efforts to provide clean water supply and improved sanitation have the potential to dramatically cut the rate of disease incidence. In fact, it has been proposed that we might expect an 88% reduction in child mortality resulting from diarrheal disease as a result of improved water sanitation and hygiene.[42][76] Similarly, a meta-analysis of numerous studies on improving water supply and sanitation shows a 22–27% reduction in disease incidence, and a 21–30% reduction in mortality rate associated with diarrheal disease.[77]
Chlorine treatment of water, for example, has been shown to reduce both the risk of diarrheal disease, and of contamination of stored water with diarrheal pathogens.[78]
Vaccination
Immunization against the pathogens that cause diarrheal disease is a viable prevention strategy, however it does require targeting certain pathogens for vaccination. In the case of Rotavirus, which was responsible for around 6% of diarrheal episodes and 20% of diarrheal disease deaths in the children of developing countries, use of a Rotavirus vaccine in trials in 1985 yielded a slight (2–3%) decrease in total diarrheal disease incidence, while reducing overall mortality by 6–10%. Similarly, a Cholera vaccine showed a strong reduction in morbidity and mortality, though the overall impact of vaccination was minimal as Cholera is not one of the major causative pathogens of diarrheal disease.[79] Since this time, more effective vaccines have been developed that have the potential to save many thousands of lives in developing nations, while reducing the overall cost of treatment, and the costs to society.[80][81]
Rotavirus vaccine decreases the rates of diarrhea in a population.[1][82] New vaccines against rotavirus, Shigella, Enterotoxigenic Escherichia coli (ETEC), and cholera are under development, as well as other causes of infectious diarrhea.[medical citation needed]
Nutrition
Dietary deficiencies in developing countries can be combated by promoting better eating practices. Zinc supplementation proved successful showing a significant decrease in the incidence of diarrheal disease compared to a control group.[83][84] The majority of the literature suggests that vitamin A supplementation is advantageous in reducing disease incidence.[85] Development of a supplementation strategy should take into consideration the fact that vitamin A supplementation was less effective in reducing diarrhea incidence when compared to vitamin A and zinc supplementation, and that the latter strategy was estimated to be significantly more cost effective.[86]
Breastfeeding
Breastfeeding practices have been shown to have a dramatic effect on the incidence of diarrheal disease in poor populations. Studies across a number of developing nations have shown that those who receive exclusive breastfeeding during their first 6 months of life are better protected against infection with diarrheal diseases.[87] One study in Brazil found that non-breastfed infants were 14 times more likely to die from diarrhea than exclusively breastfed infants.[88] Exclusive breastfeeding is currently recommended for the first six months of an infant's life by the WHO,[89][90] with continued breastfeeding until at least two years of age.[90]
Others
Management
In many cases of diarrhea, replacing lost fluid and salts is the only treatment needed. This is usually by mouth –
Medications such as
Fluids
Oral rehydration solution (ORS) (a slightly sweetened and salty water) can be used to prevent dehydration. Standard home solutions such as salted rice water, salted yogurt drinks, vegetable and chicken soups with salt can be given. Home solutions such as water in which cereal has been cooked, unsalted soup, green coconut water, weak tea (unsweetened), and unsweetened fresh fruit juices can have from half a teaspoon to full teaspoon of salt (from one-and-a-half to three grams) added per liter. Clean plain water can also be one of several fluids given.[20] There are commercial solutions such as Pedialyte, and relief agencies such as UNICEF widely distribute packets of salts and sugar. A WHO publication for physicians recommends a homemade ORS consisting of one liter water with one teaspoon salt (3 grams) and two tablespoons sugar (18 grams) added[20] (approximately the "taste of tears"[98]). Rehydration Project recommends adding the same amount of sugar but only one-half a teaspoon of salt, stating that this more dilute approach is less risky with very little loss of effectiveness.[99] Both agree that drinks with too much sugar or salt can make dehydration worse.[20][99]
Appropriate amounts of supplemental zinc and potassium should be added if available. But the availability of these should not delay rehydration. As WHO points out, the most important thing is to begin preventing dehydration as early as possible.[20] In another example of prompt ORS hopefully preventing dehydration, CDC recommends for the treatment of cholera continuing to give Oral Rehydration Solution during travel to medical treatment.[95]
Vomiting often occurs during the first hour or two of treatment with ORS, especially if a child drinks the solution too quickly, but this seldom prevents successful rehydration since most of the fluid is still absorbed. WHO recommends that if a child vomits, to wait five or ten minutes and then start to give the solution again more slowly.[20]
Drinks especially high in simple sugars, such as
Eating
The WHO recommends a child with diarrhea continue to be fed. Continued feeding speeds the recovery of normal intestinal function. In contrast, children whose food is restricted have diarrhea of longer duration and recover intestinal function more slowly. The WHO states "Food should never be withheld and the child's usual foods should not be diluted. Breastfeeding should always be continued."[20] In the specific example of cholera, the CDC makes the same recommendation.[95] Breast-fed infants with diarrhea often choose to breastfeed more, and should be encouraged to do so.[20] In young children who are not breast-fed and live in the developed world, a lactose-free diet may be useful to speed recovery.[102] Eating food containing fibers may help.[103]
Medications
Antidiarrheal agents can be classified into four different groups: antimotility, antisecretory, adsorbent, and anti-infectious.
While bismuth compounds (
Diosmectite, a natural aluminomagnesium silicate clay, is effective in alleviating symptoms of acute diarrhea in children,[111] and also has some effects in chronic functional diarrhea, radiation-induced diarrhea, and chemotherapy-induced diarrhea.[52] Another absorbent agent used for the treatment of mild diarrhea is kaopectate.
Racecadotril an antisecretory medication may be used to treat diarrhea in children and adults.[104] It has better tolerability than loperamide, as it causes less constipation and flatulence.[112] However, it has little benefit in improving acute diarrhea in children.[113]
Alternative therapies
Zinc supplementation may benefit children over six months old with diarrhea in areas with high rates of malnourishment or zinc deficiency.[115] This supports the World Health Organization guidelines for zinc, but not in the very young.
A Cochrane Review from 2020 concludes that probiotics make little or no difference to people who have diarrhea lasting 2 days or longer and that there is no proof that they reduce its duration.[116] The probiotic lactobacillus can help prevent antibiotic-associated diarrhea in adults but possibly not children.[117] For those with lactose intolerance, taking digestive enzymes containing lactase when consuming dairy products often improves symptoms.
See also
- Dysentery – Inflammation of the intestine causing diarrhea with blood
- Fernando Mazariegos – Guatemalan scientist (1938–2018)
References
- ^ a b c d e f g h "whqlibdoc.who.int" (PDF). World Health Organization. Archived (PDF) from the original on 8 November 2010.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z "Diarrhoeal disease Factsheet". World Health Organization. 2 May 2017. Archived from the original on 11 November 2020. Retrieved 29 October 2020.
- PMID 27733282.
- ^ a b Dadonaite B, Ritchie H, Roser M (1 November 2018). "Diarrheal diseases". Our World in Data. Archived from the original on 19 June 2022. Retrieved 28 April 2022.
- ^ ISBN 978-1-107-01867-9.
- PMID 22313950.

- (PDF) from the original on 9 May 2020. Retrieved 23 September 2019.
- ^ PMID 24738670.
- ISBN 978-1-4557-3985-1.
- ^ ACEP (14 October 2013). "Nation's Emergency Physicians Announce List of Test and Procedures to Question as Part of Choosing Wisely Campaign". Choosing Wisely. Archived from the original on 17 May 2014. Retrieved 18 June 2014.
- PMID 26063472.
- ^ a b "Global Diarrhea Burden". CDC. 24 January 2013. Archived from the original on 7 July 2014. Retrieved 18 June 2014.
- ^
 The dictionary definition of squits at Wiktionary
The dictionary definition of squits at Wiktionary
- ^
 The dictionary definition of runs at Wiktionary
The dictionary definition of runs at Wiktionary
- Merriam Webster. Archivedfrom the original on 11 December 2018. Retrieved 11 December 2018.
- ^ "WGO Practice Guideline – Acute diarrhea". Archived from the original on 22 February 2011. Retrieved 9 March 2011.
- ^ "Cholera outbreak toobox" (PDF). WHO. June 2019. Archived (PDF) from the original on 30 May 2022. Retrieved 2 May 2022.
- ^ a b c "The Basics of Diarrhea". Webmd.com. 17 February 2011. Archived from the original on 11 March 2011. Retrieved 9 March 2011.
- ^ PMID 26429773.
- ^ a b c d e f g h i j k "The Treatment Of Diarrhea, A manual for physicians and other senior health workers" (PDF). Sometimes needs to be downloaded twice. See "4.2 Treatment Plan A: home therapy to prevent dehydration and malnutrition," "4.3 Treatment Plan B: oral rehydration therapy for children with some dehydration," and "4.4 Treatment Plan C: for patients with severe dehydration" on pages 8 to 16 (12–20 in PDF). See also "8. Management of Diarrhoea with Severe Malnutrition" on pages 22–24 (26–30 in PDF) and "Annex 2: Oral and Intravenous Rehydration Solutions" on pages 33–37 (37–41 in PDF). World Health Organization. 2005. Archived (PDF) from the original on 19 October 2011.
- PMID 22677080.
- ^ a b Disease Control Priorities Project. "Public Health Significance of Diarrheal Illnesses". The World Bank Group. Archived from the original on 25 January 2014. Retrieved 12 October 2013.
- PMID 1632474.
- PMID 10828173.
- OCLC 32308337.
- ^ "Diarrhea: Types, Causes, Complications & Treatment". Cleveland Clinic. Archived from the original on 19 July 2022. Retrieved 19 July 2022.
- ^ PMID 16267716.
- ^ "Microscopic colitis - Symptoms and causes". Mayo Clinic. Archived from the original on 3 April 2022. Retrieved 19 July 2022.
- S2CID 34096072.
- ISBN 978-1-139-57665-9. Archivedfrom the original on 14 January 2023. Retrieved 9 September 2017.
- PMID 19084472.
- PMID 19457420.
- PMID 1962727.
- S2CID 3177998.
- from the original on 15 June 2022, retrieved 19 July 2022
- PMID 19116615.
- S2CID 23376891.
- PMID 22301075.
- S2CID 26076784.
- ^ "WHO | Diarrhoeal disease". Who.int. Archived from the original on 1 April 2014. Retrieved 10 March 2014.
- ISBN 978-0-8213-6179-5.
- ^ PMID 23761692.
- PMID 11509100.
- PMID 9701160.
- PMID 9701154.
- ^ Rice AL, West KP, Black RE (2004). "Vitamin A deficiency" (PDF). In Ezzati M, Lopez AD, Rodgers A, Murray CJ (eds.). Comparative quantification of health risks: global and regional burden of disease attributes to selected major risk factors. Vol. 1. Geneva: World Health Organization. pp. 211–56, especially 238–240. Archived (PDF) from the original on 31 July 2020. Retrieved 30 December 2018.
- PMID 6496388.
- PMID 12221262.
- PMID 16678561.
- S2CID 11327665.
- ISBN 978-0-07-139140-5.
- ^ PMID 26576135.
- ISBN 978-0-8036-5705-2.
- ^ Dekel R, Sperber AD. "Diarrhea & Incontinence Caused by Medication". International Foundation for Gastrointestinal Disorders (IFFGD). Archived from the original on 24 February 2017. Retrieved 18 May 2017.
- PMID 29928670.
- ISBN 978-0-679-74674-4.
- PMID 4587313.
- PMID 2371542.
- PMID 29653941.
- ^ PMID 31302098.
- ^ "Mortality and Burden of Disease Estimates for WHO Member States in 2004" (xls). World Health Organization. Archived from the original on 28 August 2021. Retrieved 4 October 2020.
- ISBN 978-0-443-06643-6. Archivedfrom the original on 18 October 2013.
- ^ "Diarrhoea: why children are still dying and what can be done" (PDF). World Health Organization. Archived (PDF) from the original on 19 October 2013. Retrieved 12 October 2013.
- ^ a b "Call to action on sanitation" (PDF). United Nations. Archived from the original (PDF) on 19 August 2014. Retrieved 15 August 2014.
- PMID 23582727.
- PMID 22235266.
- PMID 12764516.
- ^ (PDF) from the original on 13 April 2020. Retrieved 17 December 2019.
- ^ PMID 33539552.
- PMID 24066070.
- PMID 31549742.
- PMID 20556776.
- PMID 12726975.
- PMID 20348121.
- ^ "Diarrheal Diseases in Less Developed Countries". CDC. Archived from the original on 4 November 2013. Retrieved 28 October 2013.
- S2CID 14509705.
- PMID 3878742.
- PMID 17297049.
- PMID 3876173.
- PMID 19817595.
- ISBN 978-92-4-150043-2. Archived(PDF) from the original on 3 September 2014.
- PMID 14973994.
- PMID 12730449.
- PMID 10586170.
- PMID 21868478.
- PMID 23930984.
- S2CID 30952224.
- ISBN 978-0-323-35776-0.
- ^ Sguassero Y. "Optimal duration of exclusive breastfeeding: RHL commentary". WHO. Archived from the original on 3 November 2013. Retrieved 14 October 2013.
- ^ a b "Infant and young child feeding". World Health Organization. 3 October 2017. Archived from the original on 8 February 2015. Retrieved 5 January 2018.
- PMID 22570464.
- PMID 30556598.
- from the original on 28 October 2014.
- ^ "BestBets: Does Withholding milk feeds reduce the duration of diarrhoea in children with acute gastroenteritis?". Archived from the original on 4 May 2009.
- ^ a b c Community Health Worker Training Materials for Cholera Prevention and Control Archived 20 October 2011 at the Wayback Machine, CDC, slides at back are dated 17 November 2010. Page 7 states "... Continue to breastfeed your baby if the baby has watery diarrhea, even when traveling to get treatment. Adults and older children should continue to eat frequently."
- PMID 21735409.
- PMID 18192963.
- ^ A Guide on Safe Food for Travellers Archived 9 July 2012 at the Wayback Machine, Welcome to South Africa, Host to the 2010 FIFA World Cup (bottom left of page 1).
- ^ a b Rehydration Project, "Diarrhoea, Diarrhea, Dehydration, Oral Rehydration, Mother and Child Nutrition, Water, Sanitation, Hygiene – Rehydration Project". Archived from the original on 8 June 2015. Retrieved 22 June 2015. Homemade Oral Rehydration Solution Recipe.
- ^ a b "Management of acute diarrhoea and vomiting due to gastroenteritis in children under 5". National Institute of Clinical Excellence. April 2009. Archived from the original on 2 August 2009.
- PMID 15861741.
- PMID 24173771.
- ^ "The Facts About Fiber". Archived from the original on 27 July 2020. Retrieved 25 January 2020.
- ^ S2CID 56519371.
- PMID 8783703.
- ^ PMID 19450323.
- PMID 10874060.
- ^ "Diarrhoeal Diseases". World Health Organization. February 2009. Archived from the original on 15 December 2008.
- PMID 19538576.
- PMID 19457416.
- PMID 19301931.
- ISBN 978-3-7741-9846-3.
- PMID 31858591.
- S2CID 12016216.
- PMID 27996088.
- PMID 33295643.
- S2CID 21836205.
