Diffuse large B-cell lymphoma
| Diffuse large B cell lymphoma | |
|---|---|
| Other names | DLBCL or DLBL |
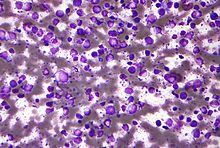 | |
| Micrograph (Field stain) of a diffuse large B cell lymphoma. | |
| Specialty | Hematology, oncology, dermatology |
Diffuse large B-cell lymphoma (DLBCL) is a cancer of B cells, a type of lymphocyte that is responsible for producing antibodies. It is the most common form of non-Hodgkin lymphoma among adults,[1] with an annual incidence of 7–8 cases per 100,000 people per year in the US and UK.[2][3] This cancer occurs primarily in older individuals, with a median age of diagnosis at ~70 years,[3] although it can occur in young adults and, in rare cases, children.[4] DLBCL can arise in virtually any part of the body and, depending on various factors, is often a very aggressive malignancy.[5] The first sign of this illness is typically the observation of a rapidly growing mass or tissue infiltration that is sometimes associated with systemic B symptoms, e.g. fever, weight loss, and night sweats.[6]
The causes of diffuse large B-cell lymphoma are not well understood. Usually DLBCL arises from normal B cells, but it can also represent a
Diagnosis of DLBCL is made by removing a portion of the tumor through a biopsy, and then examining this tissue using a microscope. Usually a hematopathologist makes this diagnosis.[15] Numerous subtypes of DLBCL have been identified which differ in their clinical presentations, biopsy findings, aggressive characteristics, prognoses, and recommended treatments.[16] However, the usual treatment for most subtypes of DLBCL is chemotherapy combined with a monoclonal antibody drug that targets the disease's cancerous B-cells, usually rituximab.[17] Through these treatments, more than half of all patients with DLBCL can be cured;[18] the overall cure rate for older adults is less than this but their five-year survival rate has been around 58%.[19]
Subtypes of diffuse large B-cell lymphoma
Diffuse large B-cell lymphoma encompasses a biologically and clinically diverse set of disease subtypes,
Diffuse large B-cell lymphoma, not otherwise specified
DLBCL cases that do not fit the distinctive clinical presentation, tissue morphology, neoplastic cell phenotype, and/or pathogen-associated criteria of other DLBCL subtypes are termed Diffuse large B-cell lymphoma, not otherwise specified: DLBCL, NOS, while representing 80–85% of all DLBCL cases, is a diagnosis of exclusion. In general, DLBCL, NOS is an aggressive disease with an overall long-term survival rate in patients treated with standard chemotherapy regimens of ~65%. However, this disease has many variants that differ not only in the just cited parameters but also in their aggressiveness and responsiveness to treatment.[24]
Presenting signs and symptoms
About 70% of DLBCL, NOS cases present primarily with lymph node disease. In these cases, the most typical presenting symptom at the time of diagnosis is a mass that is rapidly enlarging and located in a part of the body with multiple lymph nodes such as the groin, arm pits, or neck. In the remaining ~30% of other cases, the disease begins as an extranodal lymphoma, most commonly in the stomach,
Prognostic indicators based on clinical presentation
The
Pathophysiology
Most cases of DLBCL, NOS appear to result at least in part from the step-wise development of
- Bcl-2-associated X protein and Bcl-2 homologous antagonist killer.[27]
- BCL6: This genes' product, Bcl-6, is a repressor of transcription that regulates the expression of other genes which control cell maturation, proliferation, and survival.[27]
- MYC: This proto-oncogene's product, Myc, encodes a transcription factor which regulates the expression of other genes whose products stimulate cell proliferation and expansion to extra-nodal tissues.[28]
- EZH2: This gene's product, the EZH2 protein, is a histone-lysine N-methyltransferase. It thereby regulates the expression of other genes which control lymphocyte maturation.[22]
- MYD88: This gene's product is a signal transducing adaptor protein essential for the transduction of interleukin-1 and toll-like receptor signaling pathways. It thereby regulates NF-κB and MAPK/ERK signaling pathways that control cell proliferation and survival.[27]
- coactivator; it activates numerous transcription factors, some of which control cell proliferation.[14]
- CD79A and CD79B: these genes' products are critical components of the B-cell receptor. Mutations in either gene can cause uncontrolled cell activation and proliferation.[14]
- PAX5: this gene's product, Pax-5, is a transcription factor that controls the development, maturation, and survival of B-cells; it also controls expression of the MYC gene in these cells.[29]
As a consequence of these gene changes and possibly other changes that have not yet been identified, the neoplastic cells in DLBCL, NOS exhibit pathologically overactive NF-κB, PI3K/AKT/mTOR, JAK-STAT0, MAPK/ERK, B-cell receptor, toll-like receptor, and NF-κB signaling pathways and thereby uncontrolled pro-malignant behaviors.[27]
Diagnosis
Microscopic examinations of involved tissues reveal large neoplastic cells that are typically classified as B-cells based on their expression of B-cell marker proteins (e.g.
Variants of DLBCL, NOS
The World Health Organization, 2016, requires that the neoplastic cells in DLBCL, NOS be further defined based on whether they are derived from germinal center B-cells (i.e. GBC) or activated B-cells (i.e. ABC) as identified by gene expression profiling (GEP) or are GBC or non-GBC as identified by immunohistochemical (IHC) analyses. As identified by GEP, which measures all cellular messenger RNAs, GBC and ABC represent about 50 and ~35% of DLBCL, NOS cases, respectively, with ~15% of cases being unclassifiable.[30] IHC analyses measure the cellular expression of specific proteins using a panel of fluorescent antibodies that bind to and therefore stain a set of key proteins. For example, one commercially available panel uses three antibodies to detect CD10, BCL6, and MUM1 proteins; GBC express whereas ABC and unidentified cells do not express these proteins; accordingly, this as well as other IHC panels classify ABC and undetermined neoplastic cell types together as non-GBC.[27] Individuals with the ABC, unclassifiable, and non-GBC variants have significantly worse prognoses than individuals with the GBC variant:[24] respective 5 year progression-free and overall survival rates have been reported to be 73–80% for GBC variants and 31–56% for ABC variants. Clinically, however, most DLBCL, NOS cases are analyzed by IHC and therefore classified as either GBC or non-GBC variants with non-GBC variants having progression-free and overall survival rates similar to those of the ABC variants.[22]
Gene and protein
The neoplastic cells in almost all cases of DLBCL, NOS express CD20. Commercially available anti-CD20 antibody agents such as rituximab or Obinutuzumab (which is sometimes used in place of rituximab) kill cells that express high levels of CD20 by binding to this cell-surface protein and thereby targeting them for attack by the hosts adaptive immune system. The addition of one of these immunotherapy agents to chemotherapy protocols has greatly improved the prognosis of most DLBCL, NOS variants.[22] Neoplastic cell expression of CD30, found in 10–15% of DLBCL, NOS cases is a favorable prognostic indicator. As indicated in the following Treatments and prognoses section, expression of the CD20 and CD30 proteins as well as the CD19, CD20 CD22, CD30, CD79A, CD79B, and D-L1 proteins, expression of the MYC, BCL2, MYD88nd, and CREBBP genes, and expression of the PI3K/AKT/mTOR, JAK-STAT, B-cell receptor, toll-like receptor, and NF-κB signaling pathways are being studied as potential therapeutic targets for the individualized treatment of GBC and ABC/non-GBC DLBCL, NOS cases.[14][22]
Treatments and prognoses
First-line therapy
First-line therapy for patients with the GBC variant of DLBCL, NOS is
A phase I clinical research trial found that the addition of lenalidomide to the R-CHOP regimen produce an ~80% complete response rate in GBC as well as non- GBC DLBCL, NOS variants.[14] Two phase III clinical research trials are underway to confirm these results and determine if the R-CHOP + lenalidomide regimen is superior to R-CHOP in the up-front treatment of GBC and/or non-GBC variants.[14]
Treatment of recurrent and refractory DLBCL, NOS
Patients with DLBCL, NOS who relapse or progress following first-line therapy have been treated with "salvage regimens" consisting of high-dose (also termed high-intensity) chemotherapy conditioning drugs followed by autologous stem cell transplantation. This regimen has attained 3-year progression-free survival rates of 21–37%.[14] Relapse following this treatment carries a very poor prognosis with median overall survival times of ~10 months.[31] Patients who have failed or because of health issues are ineligible for autologous stem cell transplantation have been treated with low-dose (i.e. low-intensity) chemotherapy conditioning regimens followed by allogeneic stem cell transplantation. This regimen has achieved 3 year progression-free and overall survival rates of 41% and 52%, respectively.[33] Further studies are underway to determine the best treatment regimens for these cases.[14][33] Patients refractory to first-line therapy or who relapse within 12 months of receiving salvage therapy (including bone marrow transplant) for recurrent disease have had poor prognoses with median overall survival rates of 3.3 and 6.3 months, respectively.[14] The prognosis of these patients appears to be improved by using CAR-T therapy.
Chimeric antigen receptor T cell (i.e. CAR-T)
CAR-T therapy for DLBCL, NOS has been used on patients who are refractory to and/or have progressed on first-line as well as salvage (including autologous stem cell transplantation) treatment regimens. Patients are treated first with a conditioning chemotherapy regimen, usually cyclophosphamide and
Glofitamab (Columvi) is a bispecific monoclonal antibody that was approved for medical use in Canada in March 2023.[41]
Emerging therapies
Neoplastic cell expression of CD30 in DLBCL, NOS is a favorable prognostic indicator; in these cases, brentuximab vedotin may be a useful addition to chemotherapy treatment protocols. This agent is a CD30-targeting antibody that delivers a toxin, monomethyl auristatin E, to CD30-expressing cells, has therapeutic efficacy against other CD30-expressing lymphomas, and may prove useful in treating the 10–15% of DLBCL, NOS cases expressing this protein. The neoplastic cells in the GBC variant of DLBCL, NOS often have mutations in the EZH2, BCL2 and CREBBP genes and overactive PI3K/AKT/mTOR and JAK-STAT signaling pathways while neoplastic cells in the ABC variant often have mutations in the MYD88, CD79A and CD79B (polatuzumab vedotin) genes and overactive B-cell receptor, toll-like receptor, and NF-κB signaling pathways.[22] These different gene mutations and dysregulated signaling pathways are also being studied as potential therapeutic targets for the individualized treatment of GBC and ABC/non-GBC cases.[14] CUDC-907, an inhibitor of PI3K and histone deacetylases, is being evaluated in two separate clinical trials[42][43] for the treatment of refractory and/or relapsed DLBCL, NOS including cases with alterations in the MYC gene.[44] GSK525762, an inhibitor of the BET family of proteins, suppresses expression of the MYC gene and is undergoing a phase I clinical trial[45] for the treatment of high-grade B-cell lymphoma with MYC, BL2, and/or BL6 rearrangements (i.e. DH/THL). RO6870810, another BET inhibitor, in combination with Venetoclax, an inhibitor of the Bcl-2 protein, is likewise in a phase I clinical trial[46] for the treatment of DH/THL.[44] Pharmacological inhibition of BCL-2 is effective in most B cell lymphomas, but often leads to acquired resistance due to the expression of other major anti-apoptotic BCL-2 family proteins like BCL-XL and MCL-1.[47] Combined therapy using MCL-1 inhibitor (S63845) or BCL-XL inhibitor (A-1331852) in addition to Venetoclax can be a solution to overcome this issue.[48]
Subtypes of diffuse large B-cell lymphoma
DLBCL subtypes have been sorted into groups based on their distinctive morphology or immunophenotype, distinctive clinical issues, and distinctive virus-driven etiology. The prognoses and treatment of these subtypes varies with their severity. Most subtypes are aggressive diseases and consequently treated in a manner similar to DLBCL, NOS. Further details on these subtypes, including their treatments, can be found in their respective main article linkages.[citation needed]
DLBCL with a distinctive morphology or immunophenotype
T cell/histiocyte-rich large B-cell lymphoma
T-cell/histiocyte-rich large B-cell lymphoma (THRLBCL) is a DLBCL in which tumors containing small numbers of usually large neoplastic
ALK+ large B-cell lymphoma
ALK+ large B-cell lymphoma (ALK+ LBCL) is a DLBCL in which neoplastic lymphocytes that express the
Plasmablastic lymphoma
Plasmablastic lymphoma (PBL) is a DLBCL in which neoplastic immunoblastic or plasmablastic cells embedded in a background of other cell types infiltrate the oral/nasal cavity or much less often the gastrointestinal tract.[12] Some 70% of individuals with PBL are infected with EBV[49] and/or (particularly those with oral/nasal cavity disease) human immunodeficiency virus (HIV).[12] PBL is an aggressive disease with a median survival time of ~15 months.[12]
Intravascular large B-cell lymphoma
Intravascular large B-cell lymphoma (IVLBCL) is a DLBCL in which medium- to large-sized neoplastic B-cells infiltrate small- to medium-sized blood vessels and sinusoids in the liver, spleen, and/or bone marrow. IVLBCL may be associated with the hemophagic syndrome (i.e. excessive cytokine secretion and systemic inflammation). Patients with the latter syndrome have very short survival times.[12] The poor prognosis of this disease has been significantly improved by rituximab or similar immunochemotherapy drugs but significant proportions of these responding cases relapse, often with central nervous system involvement.[50]
Large B-cell lymphoma with IRF4 rearrangement
Large B-cell lymphoma with IRF4 rearrangement (LBCL with IRF4 rearrangement) is a DLBCL in which tissue infiltrates containing intermediate- or large-sized neoplastic B-cells strongly express a chromosomal translocation involving the IRF4 gene on the short arm of chromosome 6. These cells form follicular, follicular and diffuse, or entirely diffuse infiltrates[12] in Waldeyer's tonsillar ring or other regions of the head and neck. The disease, which represents ~0.05% of all DLBCL, occurs primarily in children and young adults and typically has a good prognoses.[24] Cases with a follicular pattern of tissue infiltrates often have indolent disease and an excellent prognosis following excision and may not need chemotherapy. Cases with a purely diffuse tissue infiltrate pattern, in contrast, often do require chemotherapy.[12]
DLBCL with distinctive clinical issues
Primary mediastinal large B-cell lymphoma
Primary mediastinal large B-cell lymphoma (PMBL), also termed primary mediastinal (thymic) large B-cell lymphoma, is a DLBCL in which neoplastic B-cells infiltrates are commonly located in
Primary cutaneous diffuse large B-cell lymphoma, leg type
Primary cutaneous diffuse large B-cell lymphoma, leg type (PCDLBCL-LT) is a DLBCL in which diffuse patterns of immunoblastic and/or centroblastic B-cells infiltrate the dermis and/or subcutaneous tissue principally, but not exclusively, of the legs. This disease's 5-year overall survival rate is 50–60%.[12]
Primary diffuse large B-cell lymphoma of the central nervous system
Primary diffuse large B-cell lymphoma of the central nervous system (DLBCL-CNS, also termed primary central nervous system lymphoma [PCNSL]) is a DLBCL in which diffuse patterns of neoplastic B-cells with centroblastic, immunoblastic, or poorly
Diffuse large B-cell lymphoma associated with chronic inflammation
Diffuse large B-cell lymphoma associated with chronic inflammation (DLBCL-CI) is an
Lymphomatoid granulomatosis
Lymphomatoid granulomatosis (LYG) is a DLBCL in which large, atypical B-cells with immunoblastic or
Primary effusion lymphoma
Primary effusion lymphoma (PEL) is a DLBCL in which neoplastic B cells that resemble immunoblasts, plasmablasts, or Reed–Sternberg cells infiltrate the pleural, pericardial, or peritoneal membranes that surround the lungs, heart, and abdominal organs, respectively. This infiltration leads to the seeping of fluid into the cavities which are encased by these membranes, i.e. it leads to pleural effusions, pericardial effusions, and abdominal ascites. Some cases of PEL also involve the gastrointestinal tract and lymph nodes. The disease occurs primarily in people who are immunosuppressed or test positive for HIV[12] and are also latently infected with Kaposi's sarcoma-associated herpesvirus;[13] PEL is an aggressive disease with an overall 1 year survival rate of ~30%.[13]
DLBCL driven by viruses
Epstein–Barr virus-positive diffuse large B-cell lymphoma, not otherwise specified
Epstein–Barr virus-positive diffuse large B cell lymphoma, not otherwise specified (EBV+ DLBCL, NOS) is a B-cell lymphoma in which neoplastic B-cells that are infected with the Epstein-Barr virus cause a disease that does not fit into other subtypes of DLBCL. In EBV+ DLBCL, small neoplastic B-cells, other lymphocyte typess, plasma cells, histiocytes and epithelioid cells interspersed with Reed–Sternberg-like cells[24] infiltrate, almost exclusively, lymph nodes.[11] Elderly patients with the disease have median survival times of ~2 years while young patients have long-term treatment-related remissions in >80% of cases.[24]
HHV8-positive diffuse large B-cell lymphoma, NOS
HHV8-positive diffuse large B-cell lymphoma, NOS (HHV8+ DLBCL, NOS; also termed HHV8-positive diffuse large B-cell lymphoma [HHV8+ DLBCL]) is a DLBCL in which
Related disorders
Helicobactor pylori associated diffuse large B-cell lymphoma
Rare cases of DLBCL are associated with the presence of the bacterium, Helicobacter pylori, in the neoplastic B-cells.
Recent studies suggest that localized, early-stage H. pylori+ DLBCL, when limited to the stomach, is successfully treated with H. pylori eradication protocols consisting of two or more antibiotics plus a proton pump inhibitor.[53][52][54][23] However, these studies also agree that patients treated with one of these H. pylori eradication regimes need to be carefully followed: those unresponsive to, or worsening on, these regimens should be switched to a chemotherapy regimen (e.g. R-CHOP) and/or, for complicated bulky disease, surgery and/or local radiotherapy.[52][23]
Epstein–Barr virus-positive mucocutaneous ulcer
Epstein-Barr virus-positive mucocutaneous ulcer (EBVMCU) was first described as a lymphoproliferative disorder in which Epstein–Barr virus-infected B-cells proliferate and cause
See also
References
- PMID 9166827.
- PMID 16150940.
- ^ PMID 22045184.
- PMID 19958356.
- ISBN 978-1-4377-2015-0.
- ^ Freeman AS, Aster JS (2012). "Epidemiology, clinical manifestations, pathologic features, and diagnosis of diffuse large B cell lymphoma". In Basow DS (ed.). UpToDate. Waltham, MA: UpToDate.
- ^ PMID 28288708.
- PMID 29524963.
- ^ Swerdlow et al. 2008, p. 233.
- PMID 29984868.
- ^ PMID 25999451.
- ^ S2CID 208142227.
- ^ PMID 30154110.
- ^ PMID 30859597.
- ^ Goldman & Schafer 2012, p. 1222.
- ^ PMID 26980727.
- ^ Goldman & Schafer 2012, p. 1225.
- S2CID 19134744.
- S2CID 23556248.
- S2CID 4382833.
- ^ Swerdlow et al. 2008, pp. 233–7.
- ^ S2CID 20839613.[permanent dead link]
- ^ PMID 31455250.
- ^ S2CID 53196244.
- ^ PMID 29931605.
- PMID 28288717.
- ^ PMID 31287161.
- PMID 28985567.
- S2CID 7127158.
- ^ S2CID 25304758.
- ^ PMID 29909914.
- ^ PMID 29289361.
- ^ PMID 29808921.
- S2CID 73475110.
- PMID 31923107.
- PMID 31723824.
- ^ PMID 31619548.
- S2CID 53249281.
- ^ "Monjuvi: FDA Approved Drugs". US FDA. Retrieved August 20, 2020.
- FDA. 11 June 2021.
- ^ "Columvi (Glofitamab for Injection) Receives Health Canada Authorization with Conditions for Adult Patients with Relapsed or Refractory Diffuse Large B-cell Lymphoma" (Press release). Roche Canada. 25 March 2023. Retrieved 24 April 2023 – via Cision Canada.
- ^ "Study to Evaluate the Efficacy and Safety of CUDC-907 in Patients With RR DLBCL, Including Patients With MYC Alterations". ClinicalTrials.gov. 30 August 2019.
- ^ "Study to Assess the Safety, Tolerability and Pharmacokinetics of Fimepinostat (CUDC-907) in Patients With Lymphoma". ClinicalTrials.gov. 5 May 2021.
- ^ S2CID 208144461.
- ^ "Testing a New Anti-cancer Drug Combination, Entinostat and GSK525762C, for Advanced and Refractory Solid Tumors and Lymphomas". ClinicalTrials.gov. 25 September 2020.
- ^ "A Study to Evaluate Safety, Pharmacokinetics, and Clinical Activity of Combination of RO6870810 and Venetoclax, With or Without Rituximab, in Participants With Relapsed/Refractory DLBCL and/or High-Grade B-Cell Lymphoma and/or High Grade B-Cell Lymphoma With MYC and/or BCL2 and/or BCL6". ClinicalTrials.gov. 27 January 2021.
- PMID 31085176.
- S2CID 208302779.
- S2CID 47010934.
- PMID 30111607.
- PMID 27521314.
- ^ PMID 24949857.
- PMID 25852262.
- PMID 31727764.
- PMID 31257347.
- ^ PMID 28477890.
- PMID 29518976.
Sources
- Swerdlow SH, Campo E, Jaffe ES, Pileri SA, eds. (2008). WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Lyon: IARC. ISBN 978-92-832-2431-0.
- Goldman L, Schafer AI (2012). Goldman's Cecil Medicine (24th ed.). ISBN 978-1-4377-1604-7.
- Turgeon ML (2005). Clinical hematology: theory and procedures. Hagerstown, MD: Lippincott Williams & Wilkins. ISBN 978-0-7817-5007-3.
