Dihydrotestosterone

| |
| |
| Names | |
|---|---|
| IUPAC name
17β-Hydroxy-5α-androstan-3-one
| |
| Systematic IUPAC name
(1S,3aS,3bR,5aS,9aS,9bS,11aS)-1-Hydroxy-9a,11a-dimethylhexadecahydro-7H-cyclopenta[a]phenanthren-7-one | |
| Other names
DHT; 5α-Dihydrotestosterone; 5α-DHT; Androstanolone; Stanolone; 5α-Androstan-17β-ol-3-one
| |
| Identifiers | |
3D model (
JSmol ) |
|
| ChEBI | |
| ChEMBL | |
| ChemSpider | |
| DrugBank | |
ECHA InfoCard
|
100.007.554 |
| KEGG | |
PubChem CID
|
|
| UNII | |
CompTox Dashboard (EPA)
|
|
| |
| |
| Properties | |
| C19H30O2 | |
| Molar mass | 290.447 g·mol−1 |
| Pharmacology | |
| A14AA01 (WHO) | |
| Transdermal (gel), in the cheek, under the tongue, intramuscular injection (as esters) | |
| Pharmacokinetics: | |
| Oral: very low (due to extensive first pass metabolism)[1] | |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa).
| |
Dihydrotestosterone (DHT, 5α-dihydrotestosterone, 5α-DHT, androstanolone or stanolone) is an
The
In addition to its role as a natural hormone, DHT has been used as a medication, for instance in the treatment of low testosterone levels in men; for information on DHT as a medication, see the androstanolone article.
Biological function
DHT is biologically important for
DHT signals act mainly in an
| Testosterone | DHT |
|---|---|
| Spermatogenesis and fertility | Prostate enlargement and prostate cancer risk |
| Male musculoskeletal development | Facial, axillary, pubic, and body hair growth |
| Voice deepening | Scalp temporal recession and pattern hair loss |
| Increased sebum production and acne | |
| Increased sex drive and erections |
In addition to normal biological functions, DHT also plays an important causative role in a number of
DHT may play a function in skeletal muscle amino acid transporter recruitment and function.[18]
5α-Reductase 2 deficiency
Much of the biological role of DHT has been elucidated in studies of individuals with
Genetic males (46,XY) with 5α-reductase type 2 deficiency are born with
Nonetheless, males with 5α-reductase type 2 deficiency exhibit signs of continued undervirilization in a number of domains.
In genetic males with 5α-reductase type 2 deficiency, the
Unlike males, genetic females with 5α-reductase type 2 deficiency are phenotypically normal. However, similarly to genetic males with the condition, they show reduced body hair growth, including an absence of hair on the arms and legs, slightly decreased axillary hair, and moderately decreased pubic hair.
5α-Reductase inhibitors
5α-Reductase inhibitors like finasteride and dutasteride inhibit 5α-reductase type 2 and/or other isoforms and are able to decrease circulating DHT levels by 65 to 98% depending on the 5α-reductase inhibitor in question.[28][29][30][22] As such, similarly to the case of 5α-reductase type 2 deficiency, they provide useful insights in the elucidation of the biological functions of DHT.[31] 5α-Reductase inhibitors were developed and are used primarily for the treatment of BPH. The drugs are able to significantly reduce the size of the prostate gland and to alleviate symptoms of the condition.[14][32] Long-term treatment with 5α-reductase inhibitors is also able to significantly reduce the overall risk of prostate cancer, although a simultaneous small increase in the risk of certain high-grade tumors has been observed.[15] In addition to prostate diseases, 5α-reductase inhibitors have subsequently been developed and introduced for the treatment of pattern hair loss in men.[33] They are able to prevent further progression of hair loss in most men with the condition and to produce some recovery of hair in about two-thirds of men.[13] 5α-Reductase inhibitors seem to be less effective for pattern hair loss in women on the other hand, although they do still show some effectiveness.[34] Aside from pattern hair loss, the drugs are also useful in the treatment of hirsutism and can greatly reduce facial and body hair growth in women with the condition.[35][16]
5α-Reductase inhibitors are overall
MK-386 is a selective 5α-reductase type 1 inhibitor which was never marketed.[42] Whereas 5α-reductase type 2 inhibitors achieve much higher reductions in circulating DHT production, MK-386 decreases circulating DHT levels by 20 to 30%.[43] Conversely, it was found to decrease sebum DHT levels by 55% in men versus a modest reduction of only 15% for finasteride.[44][45] However, MK-386 failed to show significant effectiveness in a subsequent clinical study for the treatment of acne.[46]
Biological activity
DHT is a
The
Unlike other androgens such as testosterone, DHT cannot be converted by the enzyme aromatase into an estrogen like estradiol. Therefore, it is frequently used in research settings to distinguish between the effects of testosterone caused by binding to the AR and those caused by testosterone's conversion to estradiol and subsequent binding to and activation of ERs.[53] Although DHT cannot be aromatized, it is still transformed into metabolites with significant ER affinity and activity. These are 3α-androstanediol and 3β-androstanediol, which are predominant agonists of the ERβ.[19]
Biochemistry
Biosynthesis
DHT is synthesized
There are two major
Backdoor pathway

DHT under certain normal and pathological conditions can additionally be produced via a route that does not involve testosterone as an intermediate but instead goes through other intermediates.[17] This route is called the "backdoor pathway".[64]
The pathway can start from
This pathway is not always considered in the clinical evaluation of patients with
As with the conventional pathway of DHT synthesis, the backdoor pathway similarly requires
Distribution
The
| Compound | Group | Level (nM) | Free (%) | SHBG (%) | CBG (%) |
Albumin (%) |
|---|---|---|---|---|---|---|
| Testosterone | Adult men | 23.0 | 2.23 | 44.3 | 3.56 | 49.9 |
| Adult women | ||||||
| Follicular phase | 1.3 | 1.36 | 66.0 | 2.26 | 30.4 | |
| Luteal phase | 1.3 | 1.37 | 65.7 | 2.20 | 30.7 | |
| Pregnancy | 4.7 | 0.23 | 95.4 | 0.82 | 3.6 | |
| Dihydrotestosterone | Adult men | 1.70 | 0.88 | 49.7 | 0.22 | 39.2 |
| Adult women | ||||||
| Follicular phase | 0.65 | 0.47 | 78.4 | 0.12 | 21.0 | |
| Luteal phase | 0.65 | 0.48 | 78.1 | 0.12 | 21.3 | |
| Pregnancy | 0.93 | 0.07 | 97.8 | 0.04 | 21.2 | |
| Sources: See template. | ||||||
Metabolism
Testosterone metabolism in humans
hydroxyl (–OH) groups . |
DHT is inactivated in the liver and extrahepatic tissues like the skin into
Unlike testosterone, DHT cannot be
Excretion
DHT is
Levels
Ranges for circulating total DHT levels tested with
- Men: 30–85 ng/dL
- Women: 4–22 ng/dL
- Prepubertal children: <3 ng/dL
- Pubertal boys: 3–65 ng/dL (mean at Tanner stage 5: 43 ng/dL)
- Pubertal girls: 3–19 ng/dL (mean at Tanner stage 5: 9 ng/dL)
Ranges for circulating free DHT levels tested with HPLC–MS/MS and
- <18 years of age: not established
- Adult males: 2.30–11.60 pg/mL (0.54–2.58% free)
- Adult females: 0.09–1.02 pg/mL (<1.27% free)
Other studies and labs assessing circulating total DHT levels with
Levels of total testosterone, free testosterone, and free DHT, but not total DHT, all measured with
Circulating DHT levels in eugonadal men are about 7- to 10-fold lower than those of testosterone, and plasma levels of testosterone and DHT are highly correlated (
Medical use
DHT is available in
Performance enhancement
DHT has been used as a
Chemistry
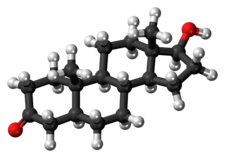
DHT, also known as 5α-androstan-17β-ol-3-one, is a
History
DHT was first synthesized by Adolf Butenandt and his colleagues in 1935.[84][85] It was prepared via hydrogenation of testosterone,[85] which had been discovered earlier that year.[86] DHT was introduced for medical use as an AAS in 1953, and was noted to be more potent than testosterone but with reduced androgenicity.[87][88][89] It was not elucidated to be an endogenous substance until 1956, when it was shown to be formed from testosterone in rat liver homogenates.[85][90] In addition, the biological importance of DHT was not realized until the early 1960s, when it was found to be produced by 5α-reductase from circulating testosterone in target tissues like the prostate gland and seminal vesicles and was found to be more potent than testosterone in bioassays.[91][92][93][94] The biological functions of DHT in humans became much more clearly defined upon the discovery and characterization of 5α-reductase type 2 deficiency in 1974.[14] DHT was the last major sex hormone, the others being testosterone, estradiol, and progesterone, to be discovered, and is unique in that it is the only major sex hormone that functions principally as an intracrine and paracrine hormone rather than as an endocrine hormone.[95]
DHT was[when?] one of the original "underground" methods used to falsify drug testing in sport, as DHT does not alter the ratio of testosterone to epistestosterone in an athlete's urinary steroid profile, a measurement that was once the basis of drug tests used to detect steroid use. However, DHT use can still be detected by other means which are now universal in athletic drug tests, such as metabolite analysis.[96]
In 2004, Richard Auchus, in a review published in
In 2011, Chang et al.
References
- PMID 9365393.
- ^ PMID 16985920.
- PMID 1551803.
- ^ S2CID 41352599.
- ^ PMID 28472278.
- ISBN 978-0-471-13320-9.
- ^ ISBN 978-1-4443-0023-9.
- ^ ISBN 978-0-323-29738-7.
- PMID 11469812.
- ISBN 978-0-9679304-7-3. Archivedfrom the original on 10 January 2023. Retrieved 6 November 2016.
- ISBN 978-1-4020-7188-1.
- ^ S2CID 8325257.
- ^ ISBN 978-3-540-46911-7. Archivedfrom the original on 11 January 2023. Retrieved 27 September 2016.
- ^ S2CID 205537645.
- ^ PMID 22446342.
- ^ ISBN 978-3-662-45139-7.
- ^ S2CID 257943362.
- PMID 27239418.
- ^ PMID 22231829.
- S2CID 43499796.
- ^ S2CID 1093345.
- ^ ISBN 978-3-319-25430-2.
- ^ S2CID 54356569.
- PMID 431680.
- PMID 24412121.
- ^ PMID 7593420.
- ^ S2CID 73167928.
- ISBN 978-3-540-33120-9.
- ISBN 978-0-323-34026-7. Archivedfrom the original on 12 January 2023. Retrieved 16 July 2017.
- ISBN 978-0-323-08619-6.
- PMID 9667860.
- PMID 21756226.
- PMID 26370642.
- S2CID 32583007.
- ISBN 978-3-540-46911-7. Archivedfrom the original on 10 January 2023. Retrieved 16 December 2017.
- ^ PMID 27672412.
- PMID 27475241.
- ^ PMID 24955220.
- PMID 28319231.
- PMID 28319227.
- PMID 28232919.
- S2CID 85073794.
- PMID 8768856.
- PMID 9141518.
- ISSN 1530-8200.
- ^ PMID 22235201.
- ^ ISBN 978-1-61779-222-9.
- ISBN 978-1-903737-05-7. Archivedfrom the original on 24 February 2024. Retrieved 8 October 2020.
- PMID 2298157.
- ISBN 978-0-444-53199-5.
- PMID 10495361.
- ISBN 978-1-59259-654-6.
- PMID 10332569.
- ISSN 2002-4436.
- ISBN 978-1-60913-427-3.
- ISBN 978-1-4557-2503-8.
- ISBN 978-1-139-42645-9.
- ^ PMID 17326004.
- ^ ISBN 978-0-7020-5182-1.
- ISBN 978-1-60761-171-4.
- S2CID 242987808.
- PMID 30763313.
- ^ PMID 30943210.
- ^ S2CID 10631647.
- PMID 12538619.
- PMID 32610579.
- ISBN 978-1-107-01290-5. Archivedfrom the original on 11 January 2023. Retrieved 8 March 2018.
- ^ PMID 7195404.
- ISBN 978-0-683-30737-5.
- PMID 12810547.
- ISBN 978-0-471-38403-8.
- ISBN 978-3-540-33713-3.
- ^ a b "Endocrinology: Expected Values" (PDF). www.esoterix.com. LabCorp. Archived from the original (PDF) on 30 March 2020. Retrieved 3 October 2022.
- ^ PMID 16772150.
- PMID 25387259.
- ^ ISBN 978-0-7637-3252-3.
- ^ a b c d "Androstanolone Drug Profile". Adis Insight. 4 December 2006. Archived from the original on 15 February 2021. Retrieved 13 December 2016.
- ^ ISBN 978-1-4757-2085-3.
- ^ ISBN 978-3-88763-075-1.
- ^ ISBN 978-3-642-66377-2.
- ^ "Drugs@FDA: FDA Approved Drug Products". United States Food and Drug Administration. Archived from the original on 16 November 2016. Retrieved 16 November 2016.
- ^ "Drug Product Database". Health Canada. 18 March 2010. Archived from the original on 19 November 2016. Retrieved 13 November 2016.
- ^ Mottram 2003.
- ISBN 978-0-323-14611-1.
- ^ ISBN 978-1-4832-6504-9.
- ISBN 978-0-7864-1128-3.
- ISBN 978-0-8155-1526-5.
- ^ Newsweek. Newsweek. 1953.
- ^ New and Nonofficial Drugs. Lippincott. 1958.
- S2CID 36534106.
- ISBN 978-0-08-054938-5.
- ISBN 978-94-011-1822-4.
- ISBN 978-1-4200-1841-7.
- ISBN 978-1-4614-8978-8.
- PMID 28582536.
- ISBN 978-1-134-53575-0. Archivedfrom the original on 21 January 2023. Retrieved 21 January 2023.
- PMID 21795608.
- PMID 22064602.
- PMID 18471780.

