Dyspareunia
| Dyspareunia | |
|---|---|
Gynecology | |
Dyspareunia ( It can affect a small portion of the vulva or vagina or be felt all over the surface. Understanding the duration, location, and nature of the pain is important in identifying the causes of the pain.
Numerous physical, psychological, and social or relationship causes can contribute to pain during sexual encounters. Commonly, multiple underlying causes contribute to the pain. The pain can be acquired or
Underlying causes determine treatment. Many patients experience relief when physical causes are identified and treated.
In 2020, dyspareunia has been estimated to globally affect 35% of women at some point in their lives.[2]
Signs and symptoms
Those who experience pelvic pain upon attempted vaginal intercourse describe their pain in many ways. This reflects how many different and overlapping causes there are for dyspareunia.[3] The location, nature, and time course of the pain help to understand potential causes and treatments.[4]
Some describe superficial pain at the opening of the vagina or surface of the genitalia when penetration is initiated. Others feel deeper pain in the vault of the vagina or deep within the pelvis upon deeper penetration. Some feel pain in more than one of these places. Determining whether the pain is more superficial or deep is important in understanding what may be causing the pain.[5] Some patients have always experienced pain with intercourse from their very first attempt, while others begin to feel pain with intercourse after an injury or infection or cyclically with menstruation. Sometimes the pain increases over time.[citation needed]
Pain may distract from feeling pleasure and excitement. Both vaginal lubrication and vaginal dilation decrease. When the vagina is dry and undilated, penetration is more painful. Fear of being in pain can make the discomfort worse. Pain may continue despite the original source being removed, due to the learned expectation of pain. Fear, avoidance, and psychological distress around attempting intercourse can become large parts of the experience of dyspareunia.[6]
Physical examination of the vulva (external genitalia) may reveal clear reasons for pain including lesions, thin skin, ulcerations or discharge associated with vulvovaginal infections or vaginal atrophy. An internal pelvic exam may also reveal physical reasons for pain including lesions on the cervix or anatomic variation.[7]
When there are no visible findings on vulvar exam that would suggest a cause for superficial dyspareunia, a cotton-swab test may be performed. This is a test to assess for localized provoked vulvodynia.[6] A cotton tip applicator is applied at several points around the opening of the vagina; the patient reports the resulting pain on a scale from 0–10.[citation needed]
Causes
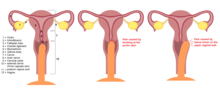
Dyspareunia in women
The cause of the pain may be anatomic or physiologic, including but not limited to lesions of the vagina, retroversion of the uterus, urinary tract infection, lack of lubrication, scar tissue, abnormal growths, or tender pelvic sites.[8] Some cases may be psychosomatic, which can include fear of pain or injury, feelings of guilt or shame, ignorance of sexual anatomy and physiology, and fear of pregnancy.[9]
Common causes for discomfort on vaginal penetration include:
- chlamydia, trichomoniasis, urinary tract infections, or herpes tend to cause more superficial pain. Infections of the cervix, or fallopian tubes like pelvic inflammatory disease[10]tend to cause deeper pain.
- Cancer of the reproductive tract, including the ovaries, cervix, uterus, or vagina.
- Tissue Injury. Pain after trauma to the pelvis from injury, surgery or childbirth.[11]
- Anatomic variations. can contribute to discomfort.
- Hormonal causes:
- Endometriosis[13] and adenomyosis
- vaginal atrophy among postmenopausal patients, and may be a result of similar changes in menstruating patients on hormonal birth control.[14] Estrogen deficiency is associated with lubrication inadequacy, which can lead to painful friction during intercourse. Vaginal dryness is often also reported alongside lactation.[15]Patients undergoing radiation therapy for pelvic malignancy often experience severe dyspareunia due to the atrophy of the vaginal walls and their susceptibility to trauma.
- Pelvic masses, including
- Pain from bladder irritation: Dyspareunia is a symptom of interstitial cystitis (IC). Patients may struggle with bladder pain and discomfort during or after sex. For an IC patient with a penis, pain occurs at the moment of ejaculation and is focused at the tip of the penis. If the IC patient has a vagina, pain usually occurs the following day and is the result of painful, spasming pelvic floor muscles. Interstitial cystitis patients also struggle with urinary frequency and/or urinary urgency.
- Vulvodynia: Vulvodynia is a diagnosis of exclusion involving either generalized or localized vulvar pain most often described as burning without physical evidence of other causes on exam. Pain can be constant or only when provoked (as with intercourse). Localized provoked vulvodynia is the most recent terminology for what used to be called vulvar vestibulitis when the pain is localized to the vaginal opening.
- Conditions that affect the surface of the vulva including Sjögren's syndrome, an autoimmune disorder that characteristically attacks the exocrine glands that produce saliva and tears.
- Muscular dysfunction: For example, levator ani myalgia
- Psychological, such as vaginismus. Most vaginal pain disorders were officially discovered or coined during a time when rape was more normalized than it is now[18] (marital rape was only recognized as non-consensual by all 50 US states in 1993[19]). Some in the medical community are now starting to take into account factors like rape/sexual assault/ fear of rape/sexual harassment as strong enough psychological stressors to cause such pain disorders.[20]
Dyspareunia in men
There are a number of physical factors that may cause sexual discomfort. Pain is sometimes experienced in the
Diagnosis
Differential diagnosis
Dyspareunia is a condition that has many causes and is not a diagnosis of itself. It is combined with vaginismus into genito-pelvic pain/penetration disorder in the DSM-5. Criteria for genito-pelvic pain/penetration disorder include multiple episodes of difficulty with vaginal penetration, pain associated with intercourse attempts, anticipation of pain due to attempted intercourse, and tensing of the pelvis in response to attempted penetration. To meet criteria for this disorder, a patient must experience the symptoms for at least six months and experience "significant distress".[24]
The differential diagnosis for dyspareunia is long because of its complicated and multifactorial nature. Often there are physiologic conditions underlying the pain, as well as psychosocial components that must be assessed to find appropriate treatment. A differential diagnosis of underlying physical causes can be guided by whether the pain is deep or superficial:[citation needed]
- Superficial dyspareunia or vulvar pain: infection, inflammation, anatomic causes, tissue destruction, psychosocial factors, muscular dysfunction
- Superficial dyspareunia without visible exam findings: When no other physical cause is found the diagnosis of vulvodynia should be considered. Vaginal atrophy may also not be seen clearly on exam but commonly affects postmenopausal patients and is generally associated with estrogen deficiency.
- Deep dyspareunia or pelvic pain: endometriosis, ovarian cysts, pelvic adhesions, inflammatory diseases (interstitial cystitis, pelvic inflammatory disease), infections, congestion, psychosocial factors,
Treatment
The treatment for pain with intercourse depends on what is causing the pain. After proper diagnosis one or more treatments for specific causes may be necessary.
For example:
- For pain due to yeast or fungal infections, a clinician may prescribe mycogen cream (nystatin and triamcinolone acetonide), which treats both a yeast infection and associated painful inflammation and itching because it contains both an antifungal and a steroid.
- For pain that is likely due to post-menopausal vaginal dryness, estrogen treatment can be used.[25]
- For patients with diagnostic criteria for endometriosis, medications or surgery are possible options.[26]
In addition, the following may reduce discomfort with intercourse:[citation needed]
- Clearly explain to the patient what has happened, including identifying sites and causes of pain. Make clear that the pain, in almost all cases, disappears over time, or at least greatly lessens. If there is a partner, explain the causes and treatment and encourage them to be supportive.
- Encourage the patient to learn about her body, explore her own anatomy and learn how she likes to be caressed and touched.
- Encourage the couple to add pleasant, sexually exciting experiences to their regular interactions, such as bathing together (in which the primary goal is not cleanliness), or mutual caressing without intercourse. Such activities tend to increase both natural lubrication and vaginal dilation, both of which decrease friction and pain. Prior to intercourse, oral sex may relax and lubricate the vagina (provided both partners are comfortable with it).
- For those who have pain on deep penetration because of pelvic injury or disease, recommend a change in coital position to one with less penetration, such as missionary position. A device has also been described for limiting penetration.[27]
- Recommend water-soluble sexual or surgical lubricant during intercourse. Discourage petroleum jelly. Lubricant should be liberally applied (two tablespoons full) to both the penis and the orifice. A folded bath towel under the receiving partner's hips helps prevent spillage on bedclothes.
- Instruct the receiving partner to take the penis of the penetrating partner in their hand and control insertion themselves, rather than let the penetrating partner do it.
History
Etymology
The word "dyspareunia" comes from Greek δυσ-, dys- "bad" and πάρευνος, pareunos "bedfellow", meaning "badly mated".[12][28]
Classification
The previous Diagnostic and Statistical Manual of Mental Disorders, the DSM-IV,[29] stated that the diagnosis of dyspareunia is made when the patient complains of recurrent or persistent genital pain before, during, or after sexual intercourse that is not caused exclusively by lack of lubrication or by vaginal spasm (vaginismus). After the text revision of the fourth edition of the DSM, a debate arose, with arguments to recategorize dyspareunia as a pain disorder instead of a sex disorder,[30] with Charles Allen Moser, a physician, arguing for the removal of dyspareunia from the manual altogether.[31] The most recent version, the DSM 5,[32] has grouped dyspareunia under the diagnosis of Genito-Pelvic Pain/Penetration Disorder.
See also
References
- ^ Multiple sources:
- JM, Vaughan CP, Goode PS, et al. Prevalence and trends of symptomatic pelvic floor disorders in US women. Obstet Gynecol. 2014;123(1):141–148.
- Bump RC, Norton PA. Epidemiology and natural history of pelvic floor dysfunc-tion. Obstet Gynecol Clin North Am. 1998;25(4):723–746.
- Basson R, Berman J, Burnett A, et al. Report of the international consensus development conference on female sexual dysfunction: definitions and clas-sifications. J Sex Marital Ther. 2001;27(2):83–94
- Vegunta S, Kling JM, Faubion SS. Sexual health matters: management of female sexual dysfunction. J Womens Health (Larchmt). 2016;25(9):952–954.
- Latif EZ, Diamond MP. Arriving at the diagnosis of female sexual dysfunction. Fertil Steril. 2013;100(4):898–904.
- Gorniak G, Conrad W. An anatomical and functional perspective of the pelvic floor and urogenital organ support system. J Womenʼs Health Phys Ther. 2015;39(2):65–82
- Happel-Parkins A., Azim K.A., Moses A. "i just beared through it": Southern US christian women's experiences of chronic dyspareunia. J. Women's Health Phys. Ther.. 2020;44(2):72-86.
- S2CID 228088155.
- )
- ^ Katz, Ditza (2020). "Painful Sex (Dyspareunia) Treatment | Women's Therapy Center". Retrieved 2021-01-22.
- PMID 20393420.
- ^ PMID 25329756.
- PMID 20393420.
- PMID 28778678.
- ISBN 978-0-8036-2505-1.
- ^ a b c d familydoctor.org editorial staff. "Dyspareunia: Painful Sex for Women".
- PMID 25605464.
- ^ PMID 13651780.
- PMID 17609078.
- PMID 24286545.
- PMID 6433154.
- ^ David Delvin (23 October 2019). "Painful intercourse (dyspareunia)".
- ^ ISBN 978-0-443-03455-8.[page needed]
- ^ "Vulvodynia: A Common and Under-Recognized Pain Disorder in Women and Female Adolescents -- Integrating Current Knowledge into Clinical Practice | Dannemiller Education Center".
- ^ Bergen, Raquel Kennedy, "Marital Rape" Archived 2011-10-06 at the Wayback Machine on the site of the Applied Research Forum, National Electronic Network on Violence Against Women. Article dated March 1999. (Retrieved September 3, 2020.)
- PMID 22698980.)
{{cite journal}}: CS1 maint: multiple names: authors list (link - ^ Whelan. "Male dyspareunia due to short frenulum: an indication for adult circumcision". BMJ 1977; 24–31: 1633-4
- S2CID 42381244.
- ^ Douglas E. "JQuad". Archived from the original on 2018-08-31. Retrieved 2014-09-23.
- ISBN 978-0-89042-555-8.
- PMID 21091878.
- PMID 23442755.
- S2CID 37484326.
- ^ From δυσ-, dys- "bad" and πάρευνος, pareunos "bedfellow".
- ISBN 978-0-89042-062-1.
- S2CID 28497075.
- S2CID 12297902.
- ISBN 978-0-89042-554-1.
- The original text for this article is taken from a public domain CDC document PDF).
Further reading
- Sandra Risa Leiblum Sexual Pain Disorders - Dyspareunia
- Binik YM, Bergeron S, Khalifé S (2000). "Dyspareunia". In Leiblum SR, Rosen RC (eds.). Principles and Practice of Sex Therapy (3rd ed.). New York: The Guilford Press. pp. 154–80. ISBN 978-1-57230-574-8.
