Epidemic

An epidemic (from
Epidemics of infectious disease are generally caused by several factors including a change in the ecology of the host population (e.g., increased stress or increase in the density of a vector species), a genetic change in the pathogen reservoir or the introduction of an emerging pathogen to a host population (by movement of pathogen or host). Generally, an epidemic occurs when host immunity to either an established pathogen or newly emerging
An epidemic may be restricted to one location; however, if it spreads to other countries or continents and affects a substantial number of people, it may be termed as a
Definition

The United States Centers for Disease Control and Prevention defines epidemic broadly: "Epidemic refers to an increase, often sudden, in the number of cases of a disease above what is normally expected in that population in that area." The term "outbreak" can also apply, but is usually restricted to smaller events.[1]: §1:72 [2]
Any sudden increase in disease prevalence may generally be termed an epidemic. This may include
The term epidemic derives from a word form attributed to Homer's Odyssey, which later took its medical meaning from the Epidemics, a treatise by Hippocrates.[5] Before Hippocrates, epidemios, epidemeo, epidamos, and other variants had meanings similar to the current definitions of "indigenous" or "endemic".[5] Thucydides' description of the Plague of Athens is considered one of the earliest accounts of a disease epidemic.[5] By the early 17th century, the terms endemic and epidemic referred to contrasting conditions of population-level disease, with the endemic condition a "common sicknesse" and the epidemic "hapning in some region, or countrey, at a certaine time, ....... producing in all sorts of people, one and the same kind of sicknesse".[6]
The term "epidemic" is often applied to diseases in non-human animals, although "epizootic" is technically preferable.[7][8]
Causes
There are several factors that may contribute (individually or in combination) to causing an epidemic. There may be changes in a pathogen, in the population that it can infect, in the environment, or in the interaction between all three. Factors include the following:[9]: §1:72
Antigenic Change

An antigen is a protein on the virus' surface that host antibodies can recognize and attack. Changes in the antigenic characteristics of the agent make it easier for the changed virus to spread throughout a previously immune population. There are two natural mechanisms for change - antigenic drift and antigenic shift. Antigenic drift arises over a period of time as an accumulation of mutations in the virus genes, possibly through a series of hosts, and eventually gives rise to a new strain of virus which can evade existing immunity. Antigenic shift is abrupt - in this, two or more different strains of a virus, coinfecting a single host, combine to form a new subtype having a mixture of characteristics of the original strains. The best known and best documented example of both processes is influenza.[10] SARS-CoV2 has demonstrated antigenic drift and possibly shift as well.[11]
Drug resistance
Changes in transmission

Pathogen transmission is a term used to describe the mechanisms by which a disease-causing agent (virus, bacterium, or parasite) spreads from one host to another. Common modes of transmission include:[16] -
- airborne (as with influenza and COVID-19),
- fecal-oral (as with cholera and typhoid),
- vector-borne(malaria, Zika) and
- sexual (syphilis, HIV)
The first three of these require that pathogen must survive away from its host for a period of time; an evolutionary change which increases survival time will result in increased virulence.[17]
Another possibility, although rare, is that a pathogen may adapt to take advantage of a new mode of transmission[18][19]
Seasonality
Seasonal diseases arise due to the change in the environmental conditions, especially such as humidity and temperature, during different seasons. Many diseases display seasonality,[20][21] This may be due to one or more of the following underlying factors: -[22]
- The ability of the pathogen to survive outside the host - e.g. water-borne cholera[23] which becomes prevalent in tropical wet seasons, or influenza which peaks in temperate regions during winter.[24][25]
- The behaviour of people susceptible to the disease - such as spending more time in close contact indoors.[26]
- Changes in immune function during winter - one possibility is a reduction in vitamin D, and another is the effect of cold on mucus membranes in the nose.[27][28]
- Abundance of vectors such as mosquitoes.[29]
Human behaviour

Changes in behaviour can affect the likelihood or severity of epidemics. The classic example is the
Changes in the host population
The level of immunity to a disease in a population - herd immunity - is at its peak after a disease outbreak or a vaccination campaign. In the following years, immunity will decline, both within individuals and in the population as a whole as older individuals die and new individuals are born. Eventually, unless there is another vaccination campaign, an outbreak or epidemic will recur.[34]
It's also possible for disease which is endemic in one population to become epidemic if it is introduced into a novel setting where the host population is not immune. An example of this was the introduction European diseases such as smallpox into indigenous populations during the 16th century.[35]
Zoonosis
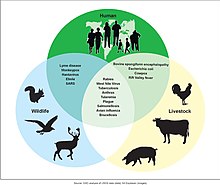
A
Types
This section needs expansion with: fuller description, examples, less jargon. You can help by adding to it. (September 2023) |
Common source outbreak
In a common source outbreak epidemic, the affected individuals had an exposure to a common agent. If the exposure is singular and all of the affected individuals develop the disease over a single exposure and incubation course, it can be termed as a point source outbreak. If the exposure was continuous or variable, it can be termed as a continuous outbreak or intermittent outbreak, respectively.[1]: 56
Propagated outbreak
In a propagated outbreak, the disease spreads person-to-person. Affected individuals may become independent reservoirs leading to further exposures.[1]: 56 Many epidemics will have characteristics of both common source and propagated outbreaks (sometimes referred to as mixed outbreak).[citation needed]
For example, secondary person-to-person spread may occur after a common source exposure or an environmental vector may spread a
Preparation
This section needs to be updated. The reason given is: Needing update to reflect changes in theory and practice since the COVID-19 pandemic. (September 2023) |
Preparations for an epidemic include having a disease surveillance system; the ability to quickly dispatch emergency workers, especially local-based emergency workers; and a legitimate way to guarantee the safety and health of health workers.[39][40]
Effective preparations for a response to a pandemic are multi-layered. The first layer is a disease surveillance system. Tanzania, for example, runs a national lab that runs testing for 200 health sites and tracks the spread of infectious diseases. The next layer is the actual response to an emergency. According to U.S.-based columnist Michael Gerson in 2015, only the U.S. military and NATO have the global capability to respond to such an emergency.[39] Still, despite the most extensive preparatory measures, a fast-spreading pandemic may easily exceed and overwhelm existing health-care resources.[41] Consequently, early and aggressive mitigation efforts, aimed at the so-called "epidemic curve flattening" need to be taken.[41] Such measures usually consist on non-pharmacological interventions such as social/physical distancing, aggressive contact tracing, "stay-at-home" orders, as well as appropriate personal protective equipment (i.e., masks, gloves, and other physical barriers to spread).[41]
See also
- List of epidemics
- Epidemiology
- Endemic (epidemiology)
- Pandemic
- Syndemic
- European Centre for Disease Prevention and Control
- Centers for Disease Control and Prevention
- Mathematical modelling of infectious disease
- Epidemic model
- Biosecurity
- Pathogen transmission
References
- ^ a b c d e f Dicker RC, Coronado F, Koo D, Parrish RG (2012). Principles of epidemiology in public health practice; an introduction to applied epidemiology and biostatistics. 3rd ed (Third ed.). Atlanta, Georgia: Centers for Disease Control and Prevention.
- ^ PMID 11802306.
- ISBN 0-86542-838-7.
- ^ Controlling the global obesity epidemic, the World Health Organization
- ^ PMID 16707055.
- ^ Lodge T (1603). A treatise of the plague: containing the nature, signes, and accidents of the same, with the certaine and absolute cure of the fevers, botches and carbuncles that raigne in these times. London: Edward White.
CHAP. 1. Of the nature and essence of the Plague
- ISSN 0029-7712. Retrieved 2023-09-11.
- ^ "Emergency response for epizootic diseases". Agri-Food and Biosciences Institute. 11 December 2005. Retrieved 11 September 2023.
- ^ Dicker RC, Coronado F, Koo D, Parrish RG (2012). Principles of epidemiology in public health practice; an introduction to applied epidemiology and biostatistics. 3rd ed (Third ed.). Atlanta, Georgia: Centers for Disease Control and Prevention.
- ^ CDC (12 December 2022). "How Flu Viruses Can Change". Centers for Disease Control and Prevention. Retrieved 9 September 2023.
- PMID 36653446.
- ^ "Antimicrobial resistance Fact sheet N°194". who.int. April 2014. Archived from the original on 10 March 2015. Retrieved 7 March 2015.
- ^ "General Background: About Antibiotic Resistance". www.tufts.edu. Archived from the original on 23 October 2015. Retrieved 30 October 2015.
- ^ "Tuberculosis (TB)". who.int. Archived from the original on 30 July 2020. Retrieved 8 May 2020.
- PMID 27788414.
- ^ "FAQ: Methods of Disease Transmission". Department of Microbiology, Mount Sinai Hospital. Retrieved 10 January 2024.
- ISSN 0362-4331. Retrieved 12 September 2023.
- PMID 36940331.
- PMID 28289251.
- PMID 30408114.
- ^ "Mark Your Calendar: All Infectious Diseases Are Seasonal". Columbia University Mailman School of Public Health. 8 November 2018. Retrieved 13 September 2023.
- PMID 16959647.
- ^ Leitzell K (20 November 2011). "The Time of Cholera". NASA Earthdata.
- ^ CDC (2022-09-20). "Learn more about the flu season". Centers for Disease Control and Prevention. Retrieved 2023-09-13.
- PMID 30958176.
- ^ Robson D (19 October 2015). "The real reason germs spread in the winter". www.bbc.com. Retrieved 14 September 2023.
- ^ Kashef Z (2019-05-13). "Flu virus' best friend: low humidity". YaleNews. Retrieved 2023-09-13.
- ^ LaMotte S (6 December 2022). "Scientists finally know why people get more colds and flu in winter". CNN. Retrieved 2023-09-14.
- ISBN 978-0-309-17770-2.
- PMC 7150208.
- PMID 26112265.
- S2CID 207998081.
- ^ Maxmen A (30 January 2015). "How the Fight Against Ebola Tested a Culture's Traditions". National Geographic. Archived from the original on March 8, 2021. Retrieved 14 September 2023.
- S2CID 220414525.
- ^ "Stacy Goodling, "Effects of European Diseases on the Inhabitants of the New World"". Archived from the original on 10 May 2008.
- ^ "Zoonoses". World Health Organization. 29 July 2020. Retrieved 14 September 2023.
- PMID 22229120.
- PMID 21912985.
- ^ a b Gerson M (26 March 2015). "The next epidemic". The Washington Post.
- PMID 25853741.
- ^ S2CID 218754925.
Further reading
- Brook, Timothy; et al. "Comparative pandemics: the Tudor–Stuart and Wanli–Chongzhen years of pestilence, 1567–1666" Journal of Global History (2020) 14#3 pp 363–379 emphasis on Chinese history, compared to England
- Eisenberg, Merle, and Lee Mordechai. "The Justinianic Plague and Global Pandemics: The Making of the Plague Concept." American Historical Review 125.5 (2020): 1632–1667.
- Honigsbaum M (18 October 2020). "How do pandemics end? In different ways, but it's never quick and never neat". The Guardian. ISSN 0261-3077. Retrieved 28 October 2020.
- Lietaert Peerbolte BJ (September 2021). "The Book of Revelation: Plagues as Part of the Eschatological Human Condition". S2CID 237332665.
- McKenna, Maryn, "Return of the Germs: For more than a century drugs and vaccines made astounding progress against infectious diseases. Now our best defenses may be social changes", Scientific American, vol. 323, no. 3 (September 2020), pp. 50–56. "What might prevent or lessen [the] possibility [of a virus emerging and finding a favorable human host] is more prosperity more equally distributed – enough that villagers in South Asia need not trap and sell bats to supplement their incomes and that, low-wage workers in the U.S. need not go to work while ill because they have no sick leave." (p. 56.)
- "Escaping the 'Era of Pandemics': Experts Warn Worse Crises to Come Options Offered to Reduce Risk". Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services. 2020.
External links
- "European Centre for Disease Prevention and Control".
- "International Epidemiological Association (IEA)". Archived from the original on 2010-11-27.
- A Dictionary of Epidemiology (IEA). Oxford University Press. 20 June 2014. ISBN 978-0-19-997672-0.
- "People's Epidemiology Library". Archived from the original on 2012-03-23.
- "Video Discussion of the Prostate Cancer Epidemic".
- "Simulations of epidemic spread across a landscape". Monash Virtual Laboratory. Archived from the original on 2007-11-04.
