Adrenaline
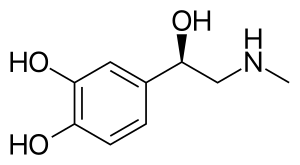 Skeletal formula of adrenaline | |
 | |
| Clinical data | |
|---|---|
| Trade names | EpiPen, Adrenaclick, others |
| Other names | Epinephrine, adrenaline, adrenalin |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a603002 |
| License data |
|
| Pregnancy category |
|
COMT) | |
| Legal status | |
| Legal status | |
COMT) | |
| Metabolites | Metanephrine[4] |
| Onset of action | Rapid[5] |
| Elimination half-life | 2 minutes |
| Duration of action | Few minutes[6] |
| Excretion | Urine |
| Identifiers | |
| |
JSmol) | |
| Density | 1.283±0.06 g/cm3 @ 20 °C, 760 Torr |
| |
| |
Adrenaline, also known as epinephrine, is a
Medical uses
As a medication, it is used to treat several conditions, including
A case has been made for the use of adrenaline infusion in place of the widely accepted treatment of
Epinephrine can also be used to treat open-angle glaucoma, as it has been found to lower the outflow of aqueous humor in the eye. This lowers the intraocular pressure in the eye and thus aids in treatment. [20]
Physiological effects
The
Pharmacological doses of adrenaline stimulate
Walter Bradford Cannon originally proposed the concept of the adrenal medulla and the sympathetic nervous system being involved in the flight, fight, and fright response.[30] But the adrenal medulla, in contrast to the adrenal cortex, is not required for survival. In adrenalectomized patients, hemodynamic and metabolic responses to stimuli such as hypoglycemia and exercise remain normal.[31][32]
Exercise
One physiological stimulus to adrenaline secretion is exercise. This was first demonstrated by measuring the dilation of a (denervated) pupil of a cat on a treadmill,[33] later confirmed using a biological assay of urine samples.[34] Biochemical methods for measuring catecholamines in plasma were published from 1950 onwards.[35] Although much valuable work has been published using fluorimetric assays to measure total catecholamine concentrations, the method is too non-specific and insensitive to accurately determine the very small quantities of adrenaline in plasma. The development of extraction methods and enzyme–isotope derivate radio-enzymatic assays (REA) transformed the analysis down to a sensitivity of 1 pg for adrenaline.[36] Early REA plasma assays indicated that adrenaline and total catecholamines rise late in exercise, mostly when anaerobic metabolism commences.[37][38][39]
During exercise, the adrenaline blood concentration rises partially from the increased secretion of the adrenal medulla and partly from the decreased metabolism of adrenaline due to reduced blood flow to the liver.[40] Infusion of adrenaline to reproduce exercise circulating concentrations of adrenaline in subjects at rest has little hemodynamic effect other than a slight β2-mediated fall in diastolic blood pressure.[41][42] Infusion of adrenaline well within the physiological range suppresses human airway hyper-reactivity sufficiently to antagonize the constrictor effects of inhaled histamine.[43]
A link between the sympathetic nervous system and the lungs was shown in 1887 when Grossman showed that stimulation of cardiac accelerator nerves reversed muscarine-induced airway constriction.[44] In experiments in the dog, where the sympathetic chain was cut at the level of the diaphragm, Jackson showed that there was no direct sympathetic innervation to the lung, but bronchoconstriction was reversed by the release of adrenaline from the adrenal medulla.[45] An increased incidence of asthma has not been reported for adrenalectomized patients; those with a predisposition to asthma will have some protection from airway hyper-reactivity from their corticosteroid replacement therapy. Exercise induces progressive airway dilation in normal subjects that correlates with workload and is not prevented by beta-blockade.[46] The progressive airway dilation with increasing exercise is mediated by a progressive reduction in resting vagal tone. Beta blockade with propranolol causes a rebound in airway resistance after exercise in normal subjects over the same time course as the bronchoconstriction seen with exercise-induced asthma.[47] The reduction in airway resistance during exercise reduces the work of breathing.[48]
Emotional responses
Every emotional response has a behavioral, an autonomic, and a hormonal component. The hormonal component includes the release of adrenaline, an adrenomedullary response to stress controlled by the
Memory
It has been found that adrenergic hormones, such as adrenaline, can produce retrograde enhancement of long-term memory in humans. The release of adrenaline due to emotionally stressful events, which is endogenous adrenaline, can modulate memory consolidation of the events, ensuring memory strength that is proportional to memory importance. Post-learning adrenaline activity also interacts with the degree of arousal associated with the initial coding.[51] There is evidence that suggests adrenaline does have a role in long-term stress adaptation and emotional memory encoding specifically. Adrenaline may also play a role in elevating arousal and fear memory under particular pathological conditions, including post-traumatic stress disorder.[50] Overall, "Extensive evidence indicates that epinephrine (EPI) modulates memory consolidation for emotionally arousing tasks in animals and human subjects."[52] Studies have also found that recognition memory involving adrenaline depends on a mechanism that depends on β adrenoceptors.[52] Adrenaline does not readily cross the blood-brain barrier, so its effects on memory consolidation are at least partly initiated by β adrenoceptors in the periphery. Studies have found that sotalol, a β adrenoceptor antagonist that also does not readily enter the brain, blocks the enhancing effects of peripherally administered adrenaline on memory.[53] These findings suggest that β adrenoceptors are necessary for adrenaline to have an impact on memory consolidation.[54][55]
Pathology
Increased adrenaline secretion is observed in pheochromocytoma, hypoglycemia, myocardial infarction, and to a lesser degree, in essential tremor (also known as benign, familial, or idiopathic tremor). A general increase in sympathetic neural activity is usually accompanied by increased adrenaline secretion, but there is selectivity during hypoxia and hypoglycemia, when the ratio of adrenaline to noradrenaline is considerably increased.[56][57][58] Therefore, there must be some autonomy of the adrenal medulla from the rest of the sympathetic system.
Myocardial infarction is associated with high levels of circulating adrenaline and noradrenaline, particularly in cardiogenic shock.[59][60]
Low or absent concentrations of adrenaline can be seen in autonomic neuropathy or following adrenalectomy. Failure of the adrenal cortex, as with Addison's disease, can suppress adrenaline secretion as the activity of the synthesizing enzyme, phenylethanolamine-N-methyltransferase, depends on the high concentration of cortisol that drains from the cortex to the medulla.[63][64][65]
Terminology
In 1901,
However, the pharmacologist
The terminology is now one of the few differences between the INN and BAN systems of names.[69] Although European health professionals and scientists preferentially use the term adrenaline, the converse is true among American health professionals and scientists. Nevertheless, even among the latter, receptors for this substance are called adrenergic receptors or adrenoceptors, and pharmaceuticals that mimic its effects are often called adrenergics. The history of adrenaline and epinephrine is reviewed by Rao.[70]
Mechanism of action
| Organ | Effects |
|---|---|
| Heart | Increases heart rate; contractility; conduction across AV node |
| Lungs | Increases respiratory rate; bronchodilation |
| Liver | Stimulates glycogenolysis |
| Muscle | Stimulates glycogenolysis and glycolysis |
| Brain | Increased cerebral tissue oxygenation |
| Systemic | Vasoconstriction and vasodilation |
| Triggers lipolysis | |
| Muscle contraction |
As a hormone, adrenaline acts on nearly all body tissues by binding to adrenergic receptors. Its effects on various tissues depend on the type of tissue and expression of specific forms of adrenergic receptors. For example, high levels of adrenaline cause smooth muscle relaxation in the airways but causes contraction of the smooth muscle that lines most arterioles.
Adrenaline is a nonselective
Adrenaline causes liver cells to release glucose into the blood, acting through both alpha and beta-adrenergic receptors to stimulate glycogenolysis. Adrenaline binds to β2 receptors on liver cells, which changes conformation and helps Gs, a heterotrimeric G protein, exchange GDP to GTP. This trimeric G protein dissociates to Gs alpha and Gs beta/gamma subunits. Gs alpha stimulates adenylyl cyclase, thus converting adenosine triphosphate into cyclic adenosine monophosphate (AMP). Cyclic AMP activates protein kinase A. Protein kinase A phosphorylates and partially activates phosphorylase kinase. Adrenaline also binds to α1 adrenergic receptors, causing an increase in inositol trisphosphate, inducing calcium ions to enter the cytoplasm. Calcium ions bind to calmodulin, which leads to further activation of phosphorylase kinase. Phosphorylase kinase phosphorylates glycogen phosphorylase, which then breaks down glycogen leading to the production of glucose.[76]
Adrenaline also has significant effects on the cardiovascular system. It increases peripheral resistance via α1 receptor-dependent vasoconstriction and increases cardiac output by binding to β1 receptors. The goal of reducing peripheral circulation is to increase coronary and cerebral perfusion pressures and therefore increase oxygen exchange at the cellular level.[77][78] While adrenaline does increase aortic, cerebral, and carotid circulation pressure, it lowers carotid blood flow and end-tidal CO2 or ETCO2 levels. It appears that adrenaline improves microcirculation at the expense of the capillary beds where perfusion takes place.[79]
Measurement in biological fluids
Adrenaline may be quantified in blood, plasma, or serum as a diagnostic aid, to monitor therapeutic administration, or to identify the causative agent in a potential poisoning victim. Endogenous plasma adrenaline concentrations in resting adults usually are less than 10 ng/L, but they may increase by 10-fold during exercise and by 50-fold or more during times of stress. Pheochromocytoma patients often have plasma adrenaline levels of 1000–10,000 ng/L. Parenteral administration of adrenaline to acute-care cardiac patients can produce plasma concentrations of 10,000 to 100,000 ng/L.[80][81]
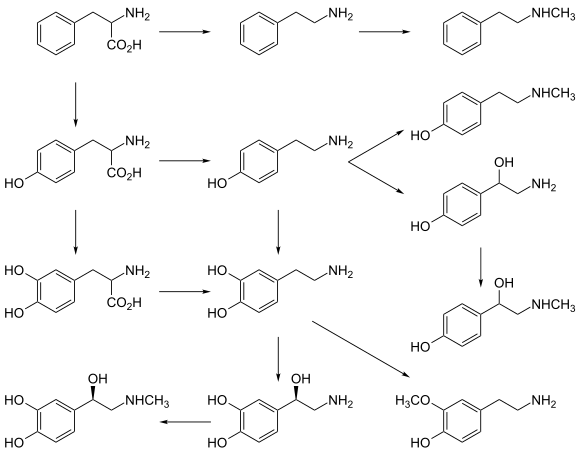
Biosynthesis
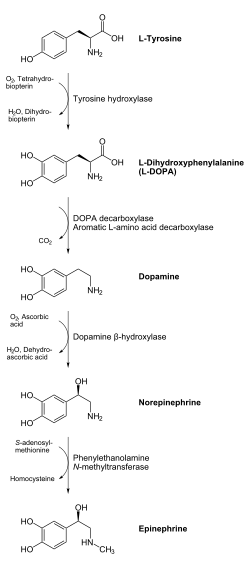
In chemical terms, adrenaline is one of a group of
Regulation
The major physiologic triggers of adrenaline release center upon
Unlike many other hormones, adrenaline (as with other catecholamines) does not exert
Its action is terminated with reuptake into nerve terminal endings, some minute dilution, and metabolism by
History
Extracts of the adrenal gland were first obtained by Polish physiologist Napoleon Cybulski in 1895.[91] These extracts, which he called nadnerczyna ("adrenalin"), contained adrenaline and other catecholamines.[92] American ophthalmologist William H. Bates discovered adrenaline's usage for eye surgeries prior to 20 April 1896.[93] In 1897, John Jacob Abel (1857–1938), the father of modern pharmacology, found a natural substance produced by the adrenal glands that he named epinephrine. The first hormone to be identified, it remains a crucial, first-line treatment for cardiac arrests, severe allergic reactions, and other conditions. In 1901, Jokichi Takamine successfully isolated and purified the hormone from the adrenal glands of sheep and oxen.[94] Adrenaline was first synthesized in the laboratory by Friedrich Stolz and Henry Drysdale Dakin, independently, in 1904.[95]
Although secretin is mentioned as the first hormone, adrenaline is the first hormone since the discovery of the activity of adrenal extract on blood pressure was observed in 1895 before that of secretin in 1902.[70] In 1895, George Oliver (1841–1915), a general practitioner in North Yorkshire, and Edward Albert Schäfer (1850–1935), a physiologist at University College of London published a paper about the active component of adrenal gland extract causing the increase in blood pressure and heart rate was from the medulla, but not the cortex of the adrenal gland.[96] In 1897, John Jacob Abel (1857–1938) of Johns Hopkins University, the first chairman of the first US department of pharmacology, found a compound called epinephrine with the molecular formula of C17H15NO4.[70] Abel claimed his principle from adrenal gland extract was active.
In 1900, Jōkichi Takamine (1854–1922), a Japanese chemist, worked with his assistant, Keizo Uenaka (1876–1960), to purify a 2000 times more active principle than epinephrine from the adrenal gland, named adrenaline with the molecular formula C10H15NO3.[70][96] Additionally, in 1900 Thomas Aldrich of Parke-Davis Scientific Laboratory also purified adrenaline independently. Takamine and Parke-Davis later in 1901 both got the patent for adrenaline. The fight for terminology between adrenaline and epinephrine was not ended until the first adrenaline structural discovery by Hermann Pauly (1870-1950) in 1903 and the first adrenaline synthesis by Friedrich Stolz (1860–1936), a German chemist in 1904. They both believed that Takamine's compound was the active principle while Abel's compound was the inactive one.[citation needed] Stolz synthesized adrenaline from its ketone form (adrenalone).[97]
Society and culture
Adrenaline junkie
An adrenaline junkie is someone who engages in sensation-seeking behavior through "the pursuit of novel and intense experiences without regard for physical, social, legal or financial risk".[98] Such activities include extreme and risky sports, substance abuse, unsafe sex, and crime. The term relates to the increase in circulating levels of adrenaline during physiological stress.[99] Such an increase in the circulating concentration of adrenaline is secondary to the activation of the sympathetic nerves innervating the adrenal medulla, as it is rapid and not present in animals where the adrenal gland has been removed.[100] Although such stress triggers adrenaline release, it also activates many other responses within the central nervous system reward system, which drives behavioral responses; while the circulating adrenaline concentration is present, it may not drive behavior. Nevertheless, adrenaline infusion alone does increase alertness[101] and has roles in the brain, including the augmentation of memory consolidation.[99]
Strength
Adrenaline has been implicated in feats of great strength, often occurring in times of crisis. For example, there are stories of a parent lifting part of a car when their child is trapped underneath.[102][103]
See also
- Noradrenaline
- Catecholamines
- Adrenal gland
References
- PMID 1136652.
- S2CID 9054777.
- PMID 5468075.
- S2CID 2330329.
- ^ a b c d "Epinephrine". The American Society of Health-System Pharmacists. Retrieved 15 August 2015.
- ISBN 9781449645861. Archivedfrom the original on 8 September 2017.
- ^ ISBN 9781608315727.
- ^ "Adrenaline". 21 August 2015.
- ^ ISBN 9780071481274.
Epinephrine occurs in only a small number of central neurons, all located in the medulla. Epinephrine is involved in visceral functions, such as the control of respiration. It is also produced by the adrenal medulla.
- ^ Larrañaga, M (2016). Hawley's Condensed Chemical Dictionary. New Jersey: John Wiley & Sons, Incorporated. p. 561.
- ^ "Adrenaline: physiology and pharmacology | DermNet". dermnetnz.org. Retrieved 20 March 2023.
- S2CID 4350616.
- ISBN 9780781768528.
- ^ ISBN 9788131215661.
- ISBN 9781483262888.
- ISBN 9781107268500.
- PMID 16595962.
- PMID 19135584.
- PMID 14974048.
- ^ Erickson, K (August 1992). "Epinephrine increases facility of outflow and cyclic AMP content in the human eye in vitro". Investigative Ophthalmology & Visual Science. 33 (9): 2672–2678.
- PMID 8818013.
- PMID 6805416.
- PMID 6248784.
- PMID 16993040.
- .
- S2CID 4214745.
- PMID 3004549.
- PMID 6795164.
- PMID 7009527.
- .
- PMID 6147094.
- PMID 3524257.
- .
- PMID 12985406.
- PMID 24537959.
- PMID 7001177.
- PMID 1110246.
- PMID 701121.
- S2CID 30270788.
- PMID 6690194.
- S2CID 38894042.
- PMID 6831836.
- PMID 6389647.
- ^ Grossman M (1887). "Das muscarin-lungen-odem". Zeitschrift für klinische Medizin. 12: 550–591.
- ^ Jackson DE (1912). "The pulmonary action of the adrenal glands". Journal of Pharmacology and Experimental Therapeutics. 4: 59–74.
- PMID 5413299.
- PMID 6228370.
- PMID 2957350.
- ^ .
- ^ PMID 23268986.
- S2CID 12099979.
- ^ S2CID 27697668.
- PMID 22122145.
- PMID 20465834.
- PMID 10366644.
- PMID 16994544.
- PMID 14777865.
- PMID 13019029.
- PMID 486283.
- PMID 495400.
- PMID 190674.
- S2CID 36267406.
- PMID 4117970.
- S2CID 36742705.
- PMID 13052791.
- ^ PMID 10678871.
- ^ European Pharmacopoeia 7.0 07/2008:2303
- ^ "Has adrenaline become a generic trademark?". genericides.org. Archived from the original on 1 May 2021.
- ^ "Naming human medicines – GOV.UK". www.mhra.gov.uk. 6 June 2019.
- ^ S2CID 144207341.
- ISBN 978-1-59541-101-3.
- PMID 3521311.
- PMID 1900669.
- ^ ISBN 978-3-13-144061-7.
- PMID 22041711.
- ISBN 0-7167-3051-0.
- ^ "Guideline 11.5: Medications in Adult Cardiac Arrest" (PDF). Australian Resuscitation Council. December 2010. Retrieved 7 March 2015.
- PMID 29984678.
- PMID 22445865.
- S2CID 12713291.
- ISBN 978-0-9626523-7-0.
- ISBN 978-3-527-31307-5.
- PMID 13436503.
- PMID 13863458.
- PMID 19948186.
- PMID 15860375.
- PMID 24374199.
- ISBN 0-7167-4339-6.
- ^ "SLC18 family of vesicular amine transporters". Guide to Pharmacology. IUPHAR/BPS. Retrieved 21 August 2015.
- S2CID 5491090.
- ISBN 9781608051892.
- PMID 16766800.
- ^ Bates WH (16 May 1896). "The Use of Extract of Suprarenal Capsule in the Eye". New York Medical Journal: 647–650. Retrieved 7 March 2015.
Read before the Section in Ophthalmology of the New York Academy of Medicine, 20 April 1896
- ^ Takamine J (1901). The isolation of the active principle of the suprarenal gland. Great Britain: Cambridge University Press. pp. xxix–xxx.
{{cite book}}:|work=ignored (help) - S2CID 20999106.
- ^ PMID 28486885.
- PMID 25969360.
- ISBN 9781591477389.
- ^ ISBN 9780521845182.
- ISBN 9783662131329.
- PMID 13701421.
- ^ Wise J (28 December 2009). "When Fear Makes Us Superhuman". Scientific American. Retrieved 25 August 2015.
- ISBN 9780230101807.
External links
 Media related to Epinephrine at Wikimedia Commons
Media related to Epinephrine at Wikimedia Commons- "U.S. National Library of Medicine: Drug Information Portal – Epinephrine". Archived from the original on 14 December 2019.