Epithelioid sarcoma
| Epithelioid sarcoma | |
|---|---|
 | |
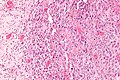
| Micrograph of an epithelioid sarcoma. H&E stain. | |
| Specialty | Oncology |
Epithelioid sarcoma is a rare
Histologically, epithelioid sarcoma forms nodules with central necrosis surrounded by bland, polygonal cells with eosinophilic cytoplasm and peripheral spindling.
Epithelioid sarcoma most commonly strikes young adults, yet no age group is immune. The disease has a tendency to develop local recurrences and metastasis thereafter to regional lymph nodes, lung, bone, brain, and other locations.[3] Generally speaking, epithelioid sarcoma has a high rate of relapse after initial treatment and tends to recur locally or regionally (at or near the original tumor site). Epithelioid sarcoma also demonstrates lymphatic spread (in 22-48% of cases), and metastasis (in 21-63% of cases).[5] These events, as well as advanced stage (progression) and grade (aggressiveness), are predictive of an overall worse outcome. Associated with a more positive outcome are younger age, female vs. male sex, distal vs. proximal location, smaller tumor size, and negative margins upon tumor resection.[1][6][7]
Signs and symptoms
Epithelioid sarcoma is a slow-growing and relatively painless tumor, often resulting in a lengthy period of time between presentation and diagnosis.
Genetics
The most common genetic mutation (found in 80-90% of epithelioid sarcomas) is the inactivation of the SMARCB1 gene, or the loss of protein INI1 function,.[10][11] Epithelioid sarcoma typically contains chromosome 22q11.2 mutations or deletions and 8q gains. Aberrations of 18q as well as recurrent gains at 11q13, have also been observed.[12][13][14]
The SMARCB1 gene (whose protein product is termed BAF47, INI1, or hSNF5) is located on chromosome
Molecular biology
A number of important proteins appear to be active in epithelioid sarcoma. Some of these are described below.
VEGF
MET
MET (mesenchymal to epithelial transition) is a biological pathway that appears to be important for the development and progression of epithelioid sarcoma.[18][19] MET is a tyrosine kinase oncogene, and its signaling pathway has been implicated in a variety of malignancies, including many cancers.[20]
Sonic hedgehog and Notch
The
mTOR
The frequent overactivation of
EGFR
The over-expression of
CD109
CD109, usually found on lymphocytes, is also expressed in epithelioid sarcoma, and is thought to mark the cancer stem cell (or cancer initiating cell) of the disease.[25] Its expression has also been shown to be predictive of outcome. Cancer stem cells are a small population of tumor cells characterized by general chemo-resistance, the ability to self-renew, multi-differentiation potential, dormancy capabilities, and tumorigenesis. In this way, cancer stem cells are thought to play key roles in the progression and relapse of cancer.
Cyclin D1
Diagnosis
Tissue
Staging
The staging for epithelioid sarcoma takes into account size and location of the primary tumor, lymph node involvement, presence and location of metastasis, and histologic grade (a measure of disease aggressiveness)[26]
Treatment
Surgery, radiation, and systemic therapy such as chemotherapy are all used at various times in the treatment of patients who have epitheloid sarcoma. Since sarcomas are considered very rare, it is not surprising that outcomes for patients with this type of cancer are better when patients are evaluated in expert centers, and when possible, treated there.[27]
Surgical resection of epithelioid sarcoma with wide margins remains the preferred method of treatment,[28] and as of 2023, remains the only curative approach for the cancer, sometimes in concert with radiation or chemotherapy.[28][29][30] Limb-sparing surgery is the standard of care for treating all sarcomas, and is used wherever possible for treatment of epithelioid sarcoma as well.[31]
In cases of advanced, recurrent, or metastasized disease, or if the tumor is inoperable, chemotherapy and radiation are the standard of care.[32] The benefit for standard medications such as doxorubicin, ifosfamide, and combinations involving gemcitabine is generally measured in months, not years.[33]
In January 2020, The U.S. Food and Drug Administration approved the oral medication tazemetostat (trade name Tazverik), a drug that blocks the EZH2 methyltransferase, for the treatment of epithelioid sarcoma in patients aged 16 years and older with either metastatic or locally advanced (unable to be completely removed surgically) disease.[34] The data that led to the drug's authorization have been supported by post-marketing studies. As with standard chemotherapy, the effectiveness of tazemetostat is generally measured in months, though some patients will fare better for a longer period of time.
Prognosis
The 5-year survival rate for epithelioid sarcoma patients is usually quoted as 50-70%, with the 10-year survival rate is 42-55%. Children with epithelioid sarcoma may have somewhat better outcomes than adults, with 5 year survival rates around 65%.
Radiation therapy is also a treatment option when tumors are deemed inoperable or wide surgical margins are not achievable. Radiation therapy in combination with chemotherapy has so far resulted in only minimal improvements to response rates. Trials with brachytherapy (an internal radiation treatment that delivers a high dose of radiation directly to the tumor and is thought to have fewer long-term side effects) have produced some positive results.[citation needed]
Research
Epithelioid sarcoma (especially advanced stage, recurrent, or metastasized disease) has been shown to become resistant to traditional cancer therapies, necessitating further exploration of novel treatment methods and techniques. Because of the relatively poor duration of the benefit of treatment of epithelioid sarcoma using traditional cancer treatments (such as chemotherapy and radiation), new treatment strategies are being examined.
Chemotherapy
New chemotherapies are being explored in current clinical trials for epithelioid sarcoma, although, thus far, none has shown significant improvement over the efficacy of doxorubicin and/or ifosfamide. Newer agents include gemcitabine, taxanes, vinorelbine and pazopanib.[32]
Aldoxorubicin was designed to safely deliver a higher dose of the drug directly to the tumor, resulting in less toxicity. Phase I and II studies of aldoxorubicin were undertaken and little cardiac toxicity was observed. While usefulness was seen in some patients, the place of aldoxorubicin in treatment of patients with epithelioid sarcoma or other sarcomas, in particular compared to doxorubicin, has not been defined.Immunotherapies
Anti-angiogenic therapies
Several
"Targeted" therapies
Given the multiple genetic abnormalities and disrupted biological pathways observed in epithelioid sarcoma, drugs targeting unique tumor characteristics are being examine for more effective treatments.
Tyrosine kinase inhibitors
It functions as an “on” or “off” switch for many cellular functions, including signaling within the cell, and cell division.Tyrosine kinases can contain mutations that cause them to become constitutively active,[49] or stuck in the “on” position, resulting in unregulated cell division (a hallmark of cancer). Tyrosine kinase Inhibitors block the action of these enzymes. Tyrosine kinase inhibitors have been shown to inhibit the VEGF, EGFR, and MET,[48] pathways that are frequently over-expressed in epithelioid sarcoma. They also can be used against the KIT and JAK-STAT signaling pathways,[48] which are involved in many cancers and may be involved in epithelioid sarcoma. Temsirolimus is a tyrosine kinase inhibitor that blocks the effects of the mTOR protein and inhibits the mTOR pathway. Because of crosstalk between cell signaling pathways, it has been shown that, while interfering with the mTOR pathway alone produces only limited results in halting tumorigenesis, inhibiting both the mTOR and the EGFR pathways concurrently shows an increased effect.[22]
SINE
Selective inhibitors of nuclear export (
HDAC inhibitors
Histone deacetylase (
CDK inhibitors
Because of the association (see above) with cyclin D1 CDK inhibitors are being studied in a variety of cancers. Palbociclib is a CDK inhibitor (approved for some breast cancer by virtue of its blockade of CDK4 and CDK6). Other experimental CDK4/6 inhibitors include abemaciclib and ribociclib.
Targeting the cancer stem cell
Oncolytic viral therapy
It has been noted that the therapeutic potential of
Telomelysin (OBP-301) is an adenovirus that targets telomerase,[56] an enzyme that is expressed in practically all cancer cells but not in normal cells. OBP-301 is not approved for use in cancer patients, but it has been studied in epithelioid sarcoma and shown to promote apoptosis and cell death in the laboratory.[56]
Additional images
-
Intermed. mag.
-
High mag.
-
High mag. (SMARCB1)
See also
- Soft tissue sarcoma
- Sarcoma
- Malignant rhabdoid tumour
- Atypical teratoid/rhabdoid tumour
References
- ^ PMID 5476785.
- PMID 9042279.
- ^ PMID 19415960.
- PMID 15078911.
- S2CID 21163484.
- ^ S2CID 25321347.
- PMID 19224301.
- ^ a b c d Lev, Dina. "Epigenetic reprogramming of epitheliold sarcoma: a role for INI1-HDAC crosstalk". Archived from the original on 2015-04-22.
- ^ PMID 3392084. Archived from the originalon 2020-03-28. Retrieved 2015-10-06.
- ^ S2CID 5167769.
- ^ PMID 15899790.
- S2CID 23521276.
- PMID 16010416.
- ^ S2CID 24821026.
- PMID 24913006.
- ^ S2CID 21613610.
- ^ PMID 22701332.
- S2CID 30726514.
- ^ PMID 25098767.
- PMID 25098767.
- ^ Clinical trial number NCT01154452 for "Vismodegib and Gamma-Secretase/Notch Signalling Pathway Inhibitor RO4929097 in Treating Patients With Advanced or Metastatic Sarcoma" at ClinicalTrials.gov
- ^ PMID 21821699.
- ^ S2CID 11592703.
- PMID 16524687.
- ^ PMID 24376795.
- ^ Soft Tissue Sarcoma Staging at eMedicine
- PMID 31081028.
- ^ S2CID 25833518.
- PMID 14595726.
- PMID 21145727.
- ^ DeGroot, Henry; Ellison, Bruce. "Limb Salvage Surgery for Extremity Sarcomas". Archived from the original on 2015-02-08. Retrieved 2015-04-23.[unreliable medical source?]
- ^ a b Soft Tissue Sarcoma. Clinical Practice Guidelines in Oncology. National Comprehensive Cancer Network. Archived from the original on 2018-08-05. Retrieved 2015-10-06.[page needed]
- PMID 18436180.
- ^ "FDA approves first treatment option specifically for patients with epithelioid sarcoma, a rare soft tissue cancer" (Press release). FDA. January 23, 2020. Retrieved 2020-03-03.
- ^ S2CID 36504524.
- S2CID 41537913.
- PMID 1997853.
- S2CID 11701323.
- PMID 25185097.
- ^ PMID 24759624.
- ^ a b c Hu, James S; Skeate, Joseph G; Kast, Wijbe Martin (2014). "Immunotherapy in sarcoma: A brief review". Sarcoma Research International. 1 (1): id1003.
- ^ PMID 21716856.
- PMID 23761810.
- PMID 16760272.
- PMID 11980649.
- S2CID 4419118.
- PMID 12528773.
- ^ S2CID 33720.
- PMID 17311534.
- PMID 25281264.
- S2CID 16936188.
- PMID 22498582.
- PMID 22247744.
- ^ .
- ^ PMID 24551478.
- ^ S2CID 33300842.
- S2CID 22657446.
- ^ "CTG Labs - NCBI". clinicaltrials.gov. Retrieved 2023-11-12.
Further reading
- Laskin, William B.; Miettinen, Markku (2003). "Epithelioid sarcoma: new insights based on an extended immunohistochemical analysis". Archives of Pathology & Laboratory Medicine. 127 (9): 1161–8. PMID 12946229.