Gait deviations
| Abnormal gait | |
|---|---|
| Other names | Orthopedics
PM&R
Spinocerebellar Ataxia |
Gait deviations are nominally referred to as any variation of
Presentation and causes
Patients with
Patients who have
Lower-limb amputations

Over 185,000 amputations occur annually, with approximately 86% of incidents being lower-limb amputations.[4] The majority of cases are reportedly caused by vascular disease (54%) and trauma (45%).[5] Lower-limb amputees are further categorized by where the amputation occurs with respect to the knee joint. However, 34.5% of individuals with an initial foot or ankle amputation experience a progression of symptoms leading to subsequent amputations at higher levels of limb loss.[6] Out of these reamputation cases, diabetic patients had a higher likelihood of requiring further amputations, regardless of initial amputation location.[6] The rate of amputation has decreased significantly with the introduction and optimization of revascularization to combat vascular disease.[7] An increasingly studied trend in amputation rates is the gender disparity of women receiving more surgical revascularization treatments and less amputations than male counterparts.[8][9]
Transtibial
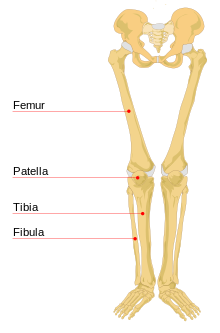
An amputation between the knee and ankle joints transecting the
Transfemoral
Unlike transtibial amputations, transfemoral amputations occur between the hip and the knee joints, along the length the femur. Therefore, the patient's residual limb is controlled solely by the hip joint. Implementing a prosthetic leg requires the user to mechanically control the behaviors of the prosthetic knee and ankle joints through gross adjustments of the hip, rather than the finer and more precise movements of the missing joints.[11] Simple tasks such as walking on level ground, sit-to-stand transfers, and climbing stairs[12] require complex alternative muscle activation patterns[13] because the amputee cannot generate a moment about the prosthetic knee.[14] This poses a problem when knee flexion is required, especially during the transition from the stance phase to the swing phase. Transfemoral amputees, on average, have more variability in stride length and walking speed, more asymmetry in temporal measures between limbs, and have an overall slower walking speed than transtibial amputees.[15]
Compensatory Behaviors

Unimpaired
Bodily involvement
Before microprocessor-controlled prosthetic joints, the major findings were that the most noticeable movements could be seen in the
Stride length
Stride length refers to the distance in the direction of forward motion that is between heel strikes of successive footfalls or steps. During the gait cycle, amputees have characteristically shorter time spent in the stance phase on the prosthetic limb compared to the intact limb.[23][24][25] Stride length is arguably the most visible of the changes in amputee gait because it creates such an asymmetry between the intact and impaired limbs. However, the shorter stance time may help the amputee compensate for the greater margin of error of the prosthetic limb, and several sources suggest the shorter strides are beneficial towards maintaining a straight walking path.[25]
Step width
Step
Gait Deviations

The compensatory behaviors listed above describe the observable differences in ambulation between amputees and able-bodied individuals. The following gait deviation measurements quantify differences using gait analysis and other tests that typically necessitate specialized instrumentation or clinical environments.
Metabolic cost
Energy expenditure is commonly used as a measure of gait quality and efficiency. Human metabolic rates are usually recorded via measuring the maximal oxygen consumption (VO2 max) during controlled incremental exercise under observation. Treadmills are used for gait analysis and standard walking tests. Able-bodied and athletic individuals on average have smaller metabolic costs than impaired individuals performing identical tasks.[39][40]
The values from a theoretical model[41] and experimental analyses[38][42][43][44][45] are listed below:
- Transtibial amputees experience 9-33% increase
- Transfemoral amputees experience 66-100% increase
Another source[46] compiled a list of average metabolic cost increases categorized by amputation location and by cause of amputation:
- Transtibial (traumatic) amputees experience 25% increase[47][48][49]
- Transtibial (vascular) amputees experience 40% increase[47][48][49]
- Transfemoral (traumatic) amputees experience 68% increase[50][18]
- Transfemoral (vascular) amputees experience 100% increase[50][18]
Comfortable walking speed
Although heavily related to the metabolic cost and overall
Mechanical work
To compensate for the amputated segment of the limb, the residual joints are used for behaviors such as foot placement and general balance on the prosthetic limb. This increases the
Other deviations
- Lateral sway
- Step variability
- Internal rotation
Similar to decreased stride length and increased step width, lateral sway is generally postulated to be an indication of gait instability. The gait naturally widens to account for a greater instability or external perturbations to balance. Step variability is also related to balance and lateral stability. The variability in length and width of steps can be attributed to a level of responsiveness to external factors and perturbations, or an indication of inherent instability and lack of control.[56] This has been a common discussion in analysis of elderly gait as well.[30][29] Internal rotation is a culmination of measures of the hip and knee joints as well as the pelvic rotation and obliquity during gait. Typically, this has to be measured through motion capture and ground reaction force. Individual parameters can be calculated with inverse kinematics.[18]
Influential Factors
Across the field of research, many studies are focused on assessing how different factors can influence the overall gait of amputee subjects. The following list shows examples of factors that are believed to influence the gait characteristics of lower-limb amputees:
- Weight of prosthesis
- Distribution of weight
- Alignment of components
- Overall fit of prosthesis
Prosthetic weight and distribution
A common trend in modern technology is the push to create lightweight devices. A 1981 collection of studies on amputees showed a 30% increase in metabolic cost of walking for an able-bodied subject with 2-kg weights fixed to each foot.[57] Correspondingly, transfemoral prostheses are on average only about one third of the weight of the limb they are replacing. However, the effect of added mass appears to be less significant for amputees. Small increases in mass (4-oz and 8-oz) of a prosthetic foot had no significant effect[58] and, similarly, adding 0.68-kg and 1.34-kg masses to the center of the shank of transfemoral prostheses did not alter metabolic cost at any of the tested walking speeds (0.6, 1.0, and 1.5 m/s).[59] In another study, muscular efforts were significantly increased with added mass, yet there was no significant impact on walking speeds and over half of the subjects preferred a prosthetic that was loaded to match 75% weight of the sound leg.[60] In fact, it has been reported in several articles that test subjects actually prefer heavier prostheses, even when the load is completely superficial.[61]
Alignment and fit
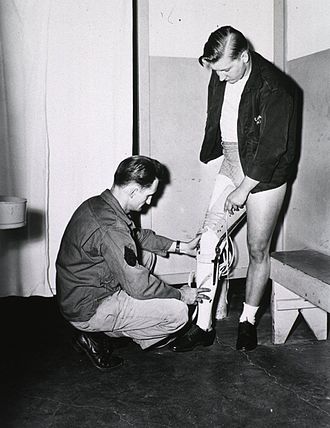
Initial alignment of a prosthetic leg is conducted by a
Transtibial
In transtibial amputees, the adjustment of the foot is highly influential to gait changes. Proper alignment of the prosthetic foot about the ankle joint causes metabolic cost[48] and gait symmetry at the anatomical hip and knee joints to improve, with hip flexion-extension motion being the most sensitive to alignment.[62] Excessive rotational misalignment of the foot is compensated by internal rotation of the residual hip joint.[63] Proper alignment of the transtibial prosthesis socket significantly reduced the loading on the intact limb during an 11-meter walk test, indicating that a misaligned limb could have drastic long-term consequences on the sound side of the body.[64]
Transfemoral
Systematic changes to transfemoral prosthetic alignment altered the flexion-extension behavior of the hip, changing fore-aft ground reaction forces and the antero-posterior moments at the knee and ankle joints.
See also
References
- PMID 19784714.
- ^ "Gait Abnormality Coding Checklist by Jun Mapili, PT, MA13212503469Ed". Selmanholman.com. Archived from the original on 2014-07-14. Retrieved 2014-06-10.
- ^ ICD-9-cm Chrisenders Archived May 21, 2005, at the Wayback Machine
- ^ "Amputation Statistics: Fact Sheet" (PDF). Center for Orthotic & Prosthetic Care.
- PMID 18295618.
- ^ PMID 15759232.
- PMID 20045618.
- PMID 24080134.
- PMID 21161738.
- ^ Smith, Douglas G (Jul–Aug 2003). "Transtibial Amputations: Successes and Challenges" (PDF). InMotion. 13 (4): 57–63.
- ISBN 978-0-6152-6870-5.
- S2CID 684443.
- PMID 23914785.
- ^ Smith, Douglas G (Mar–Apr 2004). "The Transfemoral Amputation Level, Part 1" (PDF). InMotion. 14 (2): 54–58.
- S2CID 57442354.
- ^
Tazawa, E (Aug 1997). "Analysis of torso movement of trans-femoral amputees during level walking". Prosthetics and Orthotics International. 21 (2): 129–140. PMID 9285957.
- ^
Gaunaurd, Ignacio; Gailey, Robert; Hafner, Brian J; Gomez-Marin, Orlando; Kirk-Sanchez, Neva (June 2011). "Postural asymmetries in transfemoral amputees". Prosthet Orthot Int. 35 (2): 171–180. S2CID 10632865.
- ^ a b c d
Sjodahl, C; Jarnlo, GB; Soderberg, B; Persson, BM (Dec 2003). "Pelvic motion in trans-femoral amputees in the frontal and transverse plane before and after special gait re-education". Prosthet Orthot Int. 27 (3): 227–237. PMID 14727704.
- ^ a b
Goujon-Pillet, Helene; Sapin, Emilie; Fode, Pascale; Lavaste, Francois (Jan 2008). "Three-Dimensional Motions of Trunk and Pelvis During Transfemoral Amputee Gait". Arch Phys Med Rehabil. 89 (1): 87–94. PMID 18164336.
- ^ a b
Williams, Matthew R; D'Andrea, Susan; Herr, Hugh M (June 2016). "Impact on gait biomechanics of using an active variable impedance prosthetic knee". J Neuroeng Rehabil. 13 (1): 54–64. PMID 27283318.
- ^ PMID 7632129.
- PMID 26186283.
- PMID 12633775.
- .
- ^ PMID 16740390.
- ^
Dingwell, JB; Marin, LC (2006). "Kinematic variability and local dynamic stability of upper body motions when walking at different speeds". J Biomech. 39 (3): 444–452. PMID 16389084.
- PMID 22464635.
- PMID 16982195.
- ^ PMID 17079750.
- ^ S2CID 25700608.
- S2CID 9365122.
- PMID 17805097.
- PMID 21820902.
- PMID 25108664.
- PMID 23916618.
- PMID 15519333.
- PMID 15111070.
- ^ PMID 25108643.
- PMID 10575082.
- ^ PMID 19321343.
- S2CID 9410648.
- PMID 1249111.
- ^ PMID 23466292.
- PMID 7991365.
- PMID 12443950.
- ^ Kishner, Stephen (2018-12-12). "Gait Analysis After Amputation". Medscape.
- ^ S2CID 38149995.
- ^ S2CID 25107336.
- ^ PMID 12528576.
- ^ PMID 14667949.
- PMID 26353775.
- PMID 9143432.
- S2CID 7976761.
- PMID 8931539.
- PMID 22248566.
- PMID 25590634.
- ISBN 978-0-8016-0209-2.
- PMID 860910.
- S2CID 32713979.
- PMID 2095530.
- PMID 14639566.
- PMID 6712431.
- PMID 12812324.
- ProQuest 215298715.
- PMID 1761584.
- S2CID 26966757.
External links
- Limb Loss Task Force, Amputee Coalition, Roadmap for Preventing Limb Loss in America.pdf, Knoxville, TN; 2012
- Advanced Prosthetics Center, Prosthetic Rehabilitation Manual: Transtibial (Below Knee) Amputation, Omaha, NE; 2013
- Research for this Wikipedia entry was conducted as a part of a Locomotion Neuromechanics course (APPH 6232) offered in the School of Applied Physiology at Georgia Tech
