Granulomatosis with polyangiitis
| Granulomatosis with polyangiitis | |
|---|---|
| Other names | Wegener's granulomatosis (WG) (formerly) |
 | |
| Micrograph showing features characteristic of granulomatosis with polyangiitis – a vasculitis and granulomas with multi-nucleated giant cells. H&E stain. | |
| Specialty | Immunology, rheumatology |
| Causes | Autoimmune disease |
Granulomatosis with polyangiitis (GPA), also known as Wegener's granulomatosis (WG),
The cause of GPA is unknown. Genetics have been found to play a role in GPA though the risk of inheritance appears to be low.[7]
GPA treatment depends on the severity of the disease.
The
Signs and symptoms

Initial signs are highly variable, and diagnosis can be severely delayed due to the nonspecific nature of the
- Kidney: rapidly progressive glomerulonephritis (75%), leading to chronic kidney disease
- Upper airway, eye and ear disease:
- Ears: conductive auditory tubedysfunction, sensorineural hearing loss (unclear mechanism)
- Oral cavity: strawberry gingivitis, underlying bone destruction with loosening of teeth, non-specific ulcerations throughout the lining of the mouth[17]
- Ears: conductive
- Trachea: subglottal stenosis
- Lungs: pulmonary nodules (referred to as "coin lesions"), infiltrates (often interpreted as pneumonia), cavitary lesions, bleeding in the lungs causing a person to cough up blood, and rarely bronchial stenosis.
- Arthritis: Pain or swelling (60%), often initially diagnosed as rheumatoid arthritis
- cutaneous vasculitis)
- mononeuritis multiplex
- Heart, gastrointestinal tract, brain, other organs: rarely affected.
Causes
The cause of GPA is unknown, although microbes, such as bacteria and viruses, as well as genetics have been implicated in its pathogenesis.[13][18]
Pathophysiology
Classic microscopic features of GPA include inflammation of blood vessels associated with poorly formed
It is now widely presumed that the
Diagnosis
Granulomatosis with polyangiitis is usually suspected only when a person has had unexplained symptoms for a long period of time. Determination of
If the person has signs of kidney involvement or
Classification
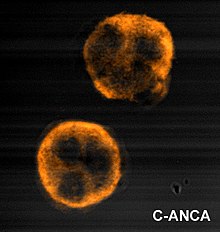
Granulomatosis with polyangiitis is part of a larger group of vasculitic syndromes called systemic vasculitides or necrotizing vasculopathies, all of which feature an autoimmune attack by an abnormal type of circulating antibody termed ANCAs (antineutrophil cytoplasmic antibodies) against small and medium-size blood vessels. Apart from GPA, this category includes eosinophilic granulomatosis with polyangiitis (EGPA) and microscopic polyangiitis.[1] Although GPA affects small- and medium-size vessels,[20] it is formally classified as one of the small vessel vasculitides in the Chapel Hill system.[2]
Criteria
In 1990, the American College of Rheumatology accepted classification criteria for GPA. These criteria were not intended for diagnosis, but for inclusion in randomized controlled trials. Two or more positive criteria have a sensitivity of 88.2% and a specificity of 92.0% of describing GPA.[14][21]

- Nasal or oral inflammation:
- painful or painless oral ulcers or
- purulentor bloody nasal discharge
- Lungs: abnormal chest X-ray with:
- nodules,
- infiltrates or
- cavities
- Kidneys: urinary sediment with:
- microscopic hematuriaor
- red cell casts
- Biopsy: granulomatous inflammation
According to the Chapel Hill Consensus Conference (CHCC) on the nomenclature of systemic vasculitis (1992), establishing the diagnosis of GPA demands:[22]
- a granulomatousinflammation involving the respiratory tract, and
- a vasculitis of small to medium-size vessels.
Several investigators have compared the ACR and Chapel Hill criteria.[23]
In 2022, American College of Rheumatology and the European Alliance of Associations for Rheumatology updated the classification criteria for GPA.[24]
Treatment
GPA treatment depends on its severity and whether it has caused organ damage.[8]
Severe disease
The standard treatment for severe GPA is to induce remission with immunosuppressants such as
Oral and intravenous cyclophosphamide are both effective for induction of GPA remission. Oral cyclophosphamide at a dose of 2 mg/kg/day was the standard treatment for many years; this regimen resulted in complete remission in more than 75% of people with GPA but is associated with significant toxicities including
Rituximab may be substituted for cyclophosphamide to induce remission since it is similarly effective and has a comparable side effect profile.
Limited disease
In generalized non-organ-threatening disease, remission can be achieved with a combination of methotrexate and corticosteroids, where the steroid dose is reduced after a remission has been achieved and methotrexate is used as maintenance therapy. Treatment measures for localised GPA of the nose and sinuses includes nasal irrigation, nasal corticosteroids, and antibiotics if infection occurs.[14] If perforation of the nasal septum occurs (or saddle nose deformity), then surgical repair is recommended.[14]
Prognosis
Before modern treatments, the 2-year survival was under 10% and average survival five months.[13][28] Death usually resulted from uremia or respiratory failure.[13] The revised Five-factor score is associated with 5-year mortality from GPA and is based on the following criteria: age greater than 65 years, cardiac symptoms, gastrointestinal involvement, chronic kidney disease, and the absence of ears, nose, and throat symptoms.[7]
With corticosteroids and
Today, medication toxicity is managed more carefully and long-term remissions are possible. Some affected individuals are able to lead relatively normal lives and remain in remission for 20+ years after treatment.[29]
Epidemiology
The incidence is 10–20 cases per million per year.[30][31] It is exceedingly rare in Japan and in African Americans.[31]
History
The full clinical picture was first presented by
See also
References
- ^ S2CID 35805200.
- ^ S2CID 21560794.
- ^ PMID 28148583.
- PMID 25399936.
- ^ PMID 26611553.
- ^ S2CID 36254262.
- ^ S2CID 206849855.
- ^ PMID 25341007.
- ^ PMID 31927782.
- ^ PMID 26587951.
- PMID 1914353.
- ^ PMID 15210387.
- ^ S2CID 206894936.
- ^ PMID 27888918.
- PMID 30521217. Retrieved 10 January 2024.
- PMID 36536738. Art. No. 104908.
- PMID 25791629.
- ^ Tracy, CL; Papadopoulos, PJ; Bye, MR; Connolly, H; Goldberg, E; O'Brian, RJ; Sharma, GD; Talavera, F; Toder, DS; Valentini, RP; Windle, ML; Wolf, RE (10 February 2014). Diamond, HS (ed.). "Granulomatosis with Polyangiitis". Medscape Reference. WebMD. Retrieved 16 March 2014.
- ^ PMID 28506361.
- ^ Gota, CE (May 2013). "Granulomatosis with Polyangiitis (GPA): Vasculitis". Merck Manual Professional. Merck Sharp & Dohme Corp. Retrieved 16 March 2014.
- PMID 2202308.
- PMID 8129773.
- PMID 9159539.
- PMID 35110333.
- ^ S2CID 8483900.
- PMID 20647199.
- ^ Tracy, CL; Papadopoulos, PJ; Bye, MR; Connolly, H; Goldberg, E; O'Brian, RJ; Sharma, GD; Talavera, F; Toder, DS; Valentini, RP; Windle, ML; Wolf, RE (10 February 2014). Diamond, HS (ed.). "Granulomatosis with Polyangiitis Treatment & Management". Medscape Reference. WebMD. Retrieved 16 March 2014.
- PMID 22569190.
- ^ "Vasculitis Foundation " Granulomatosis with Polyangiitis (GPA/Wegener's)". www.vasculitisfoundation.org. Archived from the original on 2014-09-14. Retrieved 2016-03-16.
- PMID 17684188.
- ^ S2CID 12082375.
- S2CID 222321164.
- PMID 13275478.
- S2CID 25978459.
- S2CID 12409848.

