Haematopoiesis
Haematopoiesis (/hɪˌmætəpɔɪˈiːsɪs, ˌhiːmətoʊ-, ˌhɛmə-/,[1][2] from Greek αἷμα, 'blood' and ποιεῖν 'to make'; also hematopoiesis in American English; sometimes also h(a)emopoiesis) is the formation of blood cellular components. All cellular blood components are derived from haematopoietic stem cells.[3] In a healthy adult human, roughly ten billion (1010) to a hundred billion (1011) new blood cells are produced per day, in order to maintain steady state levels in the peripheral circulation.[4][5][page needed]
Process
Haematopoietic stem cells (HSCs)
Cell types
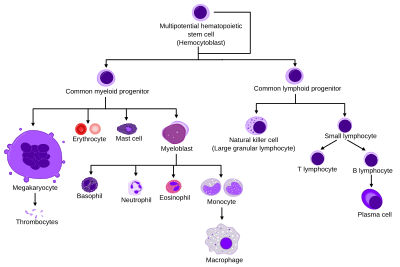
All blood cells are divided into three lineages.[9]
- Erythrocytes are functional, and are released into the blood. The number of reticulocytes, which are immature red blood cells, gives an estimate of the rate of erythropoiesis.
- natural killer cells. This is lymphopoiesis.
- Cells of the myeloid lineage, which include blood clotting. This is myelopoiesis.
Granulopoiesis (or granulocytopoiesis) is haematopoiesis of granulocytes, except mast cells which are granulocytes but with an extramedullar maturation.[10]
Thrombopoiesis is haematopoiesis of thrombocytes (platelets).
Terminology
Between 1948 and 1950, the Committee for Clarification of the Nomenclature of Cells and Diseases of the Blood and Blood-forming Organs issued reports on the nomenclature of blood cells.[11][12] An overview of the terminology is shown below, from earliest to final stage of development:
- [root]blast
- pro[root]cyte
- [root]cyte
- meta[root]cyte
- mature cell name
The root for erythrocyte colony-forming units (CFU-E) is "rubri", for granulocyte-monocyte colony-forming units (CFU-GM) is "granulo" or "myelo" and "mono", for lymphocyte colony-forming units (CFU-L) is "lympho" and for megakaryocyte colony-forming units (CFU-Meg) is "megakaryo". According to this terminology, the stages of red blood cell formation would be: rubriblast, prorubricyte, rubricyte, metarubricyte, and erythrocyte. However, the following nomenclature seems to be, at present, the most prevalent:
| Committee | "lympho" | "rubri" | "granulo" or "myelo" | "mono" | "megakaryo" |
|---|---|---|---|---|---|
| Lineage | Lymphoid |
Myeloid |
Myeloid | Myeloid | Myeloid |
| CFU | CFU-L |
CFU-GEMM→CFU-E | CFU-GEMM→ CFU-G |
CFU-GEMM→ CFU-M |
CFU-GEMM→CFU-Meg |
| Process | lymphocytopoiesis |
erythropoiesis | granulocytopoiesis |
monocytopoiesis | thrombocytopoiesis
|
| [root]blast | Lymphoblast | Proerythroblast | Myeloblast | Monoblast | Megakaryoblast |
| pro[root]cyte | Prolymphocyte | Polychromatophilic erythrocyte |
Promyelocyte | Promonocyte | Promegakaryocyte |
| [root]cyte | – | Normoblast |
basophilic myelocyte |
Megakaryocyte | |
| meta[root]cyte | Large lymphocyte | Reticulocyte | Eosinophilic/neutrophilic/basophilic metamyelocyte, Eosinophilic/neutrophilic/basophilic band cell | Early monocyte | - |
| mature cell name | Small lymphocyte | Erythrocyte |
) | Monocyte | Platelets )
|
Osteoclasts also arise from hemopoietic cells of the monocyte/neutrophil lineage, specifically CFU-GM.
Location

In developing embryos, blood formation occurs in aggregates of blood cells in the yolk sac, called
Extramedullary
In some cases, the liver, thymus, and spleen may resume their haematopoietic function, if necessary. This is called
Maturation
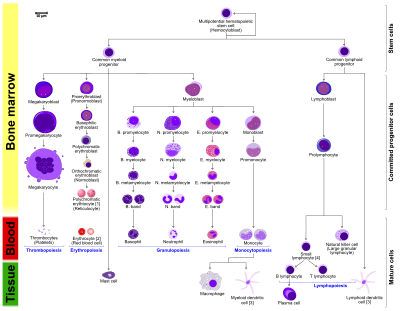
- The morphological characteristics of the hematopoietic cells are shown as seen in a Wright's stain, May-Giemsa stain or May-Grünwald-Giemsa stain. Alternative names of certain cells are indicated between parentheses.
- Certain cells may have more than one characteristic appearance. In these cases, more than one representation of the same cell has been included.
- Together, the monocyte and the lymphocytes comprise the agranulocytes, as opposed to the granulocytes (basophil, neutrophil and eosinophil) that are produced during granulopoiesis.
- B., N. and E. stand for Basophilic, Neutrophilic and Eosinophilic, respectively – as in Basophilic promyelocyte. For lymphocytes, the T and B are actual designations.
- The polychromatic erythrocyte (reticulocyte) at the right shows its characteristic appearance when stained with methylene blue or Azure B.
- The erythrocyte at the right is a more accurate representation of its appearance in reality when viewed through a microscope.
- Other cells that arise from the monocyte: osteoclast, microglia (central nervous system), Langerhans cell (epidermis), Kupffer cell (liver).
- For clarity, the T and B lymphocyte are split to better indicate that the plasma cell arises from the B-cell. Note that there is no difference in the appearance of B- and T-cells unless specific staining is applied.
As a stem cell matures it undergoes changes in gene expression that limit the cell types that it can become and moves it closer to a specific cell type (cellular differentiation). These changes can often be tracked by monitoring the presence of proteins on the surface of the cell. Each successive change moves the cell closer to the final cell type and further limits its potential to become a different cell type.[citation needed]
Cell fate determination
Two models for haematopoiesis have been proposed: determinism and stochastic theory.[20] For the stem cells and other undifferentiated blood cells in the bone marrow, the determination is generally explained by the determinism theory of haematopoiesis, saying that colony stimulating factors and other factors of the haematopoietic microenvironment determine the cells to follow a certain path of cell differentiation.[3] This is the classical way of describing haematopoiesis. In stochastic theory, undifferentiated blood cells differentiate to specific cell types by randomness. This theory has been supported by experiments showing that within a population of mouse haematopoietic progenitor cells, underlying stochastic variability in the distribution of Sca-1, a stem cell factor, subdivides the population into groups exhibiting variable rates of cellular differentiation. For example, under the influence of erythropoietin (an erythrocyte-differentiation factor), a subpopulation of cells (as defined by the levels of Sca-1) differentiated into erythrocytes at a sevenfold higher rate than the rest of the population.[21] Furthermore, it was shown that if allowed to grow, this subpopulation re-established the original subpopulation of cells, supporting the theory that this is a stochastic, reversible process. Another level at which stochasticity may be important is in the process of apoptosis and self-renewal. In this case, the haematopoietic microenvironment prevails upon some of the cells to survive and some, on the other hand, to perform apoptosis and die.[3] By regulating this balance between different cell types, the bone marrow can alter the quantity of different cells to ultimately be produced.[22]
Growth factors
Red and white blood cell production is regulated with great precision in healthy humans, and the production of leukocytes is rapidly increased during infection. The proliferation and self-renewal of these cells depend on growth factors. One of the key players in self-renewal and development of haematopoietic cells is
Transcription factors
Growth factors initiate
The first key player of differentiation from HSC to a multipotent progenitor (MPP) is transcription factor CCAAT-enhancer binding protein α (
Other transcription factors include Ikaros
An example is PAX5 factor, which is important in B cell development and associated with lymphomas.[35] Surprisingly, pax5 conditional knock out mice allowed peripheral mature B cells to de-differentiate to early bone marrow progenitors. These findings show that transcription factors act as caretakers of differentiation level and not only as initiators.[36]
Other animals
In some
Unlike eutherian mammals, the liver of newborn marsupials is actively haematopoietic.[41][42][43][44]
See also
- Clonal hematopoiesis
- Erythropoiesis-stimulating agents
- Haematopoietic stimulants:
- Granulocyte colony-stimulating factor
- Granulocyte macrophage colony-stimulating factor
- Leukocyte extravasation
References
- ^ a b "hematopoiesis". Merriam-Webster.com Dictionary. Retrieved 16 May 2022.
- ^ "haematopoiesis". Dictionary.com Unabridged (Online). n.d. Retrieved 16 October 2019.
- ^ PMID 27015419.
- ^ Semester 4 medical lectures at Uppsala University 2008 by Leif Jansson
- ISBN 978-0-8385-6278-9.
- PMID 35265979.
- S2CID 715049.
- PMID 7541305.
- ^ "Hematopoiesis from Pluripotent Stem Cells". Antibodies Resource Library. ThermoFisher Scientific. Retrieved 25 April 2020.
- ISBN 978-0-12-415759-0.
- PMID 18913573.
- PMID 15432355.
- PMID 31334965. Retrieved 4 September 2022.
- PMID 24237971.
- PMID 12388506.
- PMID 17200719.
- PMID 19644120.
- PMID 25800955.
- PMID 27470513.
- PMID 25480640.
- PMID 18497826.
- PMID 19325941.
- ^ ISBN 0-7167-4366-3
Lodish H, Berk A, Zipursky SL, Matsudaira P, Baltimore D, Darnell J (2000). "Cancers Originate in Proliferating Cells". Molecular Cell Biology (4th ed.). New York: W. H. Freeman. Figure 24-8: Formation of differentiated blood cells from hematopoietic stem cells in the bone marrow.ISBN 0-7167-3136-3– via NCBI Bookshelf. - ISBN 978-0-443-06911-6.
- PMID 9269751.
- PMID 9156123.
- .
- PMID 10508690.
- PMID 22224773.
- PMID 19304957.
- S2CID 206939258.
- PMID 17363301.
- PMID 26749286.
- PMID 26972050.
- PMID 22127921.
- S2CID 4414856.
- PMID 8986714.
- PMID 8895580.
- PMID 24013668.
- PMID 7579378.
- ^ Old JM (2016). Haematopoiesis in marsupials. Developmental and Comparative Immunology. 58, 40-46. DOI: 10.1016/j.dci.2015.11.009
- ^ Old JM, Deane EM (2000). Development of the immune system and immunological protection in marsupial pouch young. Developmental and Comparative Immunology. 24(5), 445-454. DOI: 10.1016/S0145-305X(00)00008-2
- ^ Old JM, Deane EM (2003). The lymphoid and immunohaematopoietic tissues of the embryonic brushtail possum (Trichosurus vulpecula). Anatomy and Embryology (now called Brain Structure and Function). 206(3), 193-197. DOI: 10.1007/s00429-002-0285-2
- ^ Old JM, Selwood L, Deane EM (2003). A histological investigation of the lymphoid and immunohaematopoietic tissues of the adult stripe-faced dunnart (Sminthopsis macroura). Cells Tissues Organs. 173(2), 115-121. DOI: 10.1159/000068946
Further reading
- Godin, Isabelle; Cumano, Ana, eds. (2006). Hematopoietic stem cell development. Springer. ISBN 978-0-306-47872-7.
