Hepatitis B
| Hepatitis B | |
|---|---|
| Frequency | 296 million (2019)[1] |
| Deaths | 820,000 resulting from hepatitis B (2019)[1] |
Hepatitis B is an
Many people have no symptoms during an initial infection. For others, symptoms may appear 30 to 180 days after becoming infected and can include a rapid onset of sickness with nausea, vomiting, yellowish skin, fatigue, dark urine, and abdominal pain.[1] Symptoms during acute infection typically last for a few weeks, though some people may feel sick for up to six months.[8] Deaths resulting from acute stage HBV infections are rare.[9] An HBV infection lasting longer than six months is usually considered chronic.[1] The likelihood of developing chronic hepatitis B is higher for those who are infected with HBV at a younger age. About 90% of those infected during or shortly after birth develop chronic hepatitis B,[8] while less than 10% of those infected after the age of five develop chronic cases.[5] Most of those with chronic disease have no symptoms; however, cirrhosis and liver cancer eventually develop[2] in about 25% of those with chronic HBV.[4]
The virus is transmitted by exposure to infectious
Hepatitis B infection has been preventable by
An estimated 296 million people, or 3.8% of the global population, had chronic hepatitis B infections as of 2019. Another 1.5 million developed acute infections that year, and 820,000 deaths occurred as a result of HBV.[1] Cirrhosis and liver cancer are responsible for most HBV-related deaths.[18] The disease is most prevalent in Africa (affecting 7.5% of the continent's population) and in the Western Pacific region (5.9%).[19] Infection rates are 1.5% in Europe and 0.5% in the Americas.[19] According to some estimates, about a third of the world's population has been infected with hepatitis B at one point in their lives.[18] Hepatitis B was originally known as "serum hepatitis".[20]
Signs and symptoms
Acute infection with hepatitis B virus is associated with acute viral
Chronic infection with hepatitis B virus may be asymptomatic or may be associated with chronic inflammation of the liver (chronic hepatitis), leading to cirrhosis over a period of several years. This type of infection dramatically increases the incidence of hepatocellular carcinoma (HCC; liver cancer). Across Europe, hepatitis B and C cause approximately 50% of hepatocellular carcinomas.[22][23] Chronic carriers are encouraged to avoid consuming alcohol as it increases their risk for cirrhosis and liver cancer. Hepatitis B virus has been linked to the development of membranous glomerulonephritis (MGN).[24]
Symptoms outside of the liver are present in 1–10% of HBV-infected people and include
Cause
Transmission
Transmission of hepatitis B virus results from exposure to infectious blood or body fluids containing blood. HBV is 50 to 100 times more infectious than human immunodeficiency virus (HIV).[32] HBV can be transmitted through several routes of infection. In vertical transmission, HBV is passed from mother to child (MTCT) during childbirth.[1] Without intervention, a mother who is positive for HBsAg has a 20% risk of passing the infection to her offspring at the time of birth. This risk is as high as 90% if the mother is also positive for HBeAg.[citation needed]
Early life horizontal transmission can occur through bites, lesions, certain sanitary habits, or other contact with secretions or saliva containing HBV.[33][34] Adult horizontal transmission is known to occur through sexual contact,[35] blood transfusions and transfusion with other human blood products,[36] re-use of contaminated needles and syringes.[37] Breastfeeding after proper immunoprophylaxis does not appear to contribute to mother-to-child-transmission (MTCT) of HBV.[38]
Virology
Structure
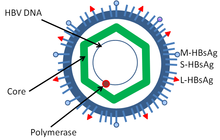
Hepatitis B virus (HBV) is a member of the
Genome
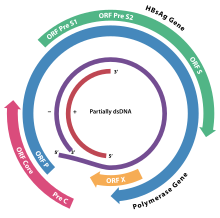
The
The function of the protein coded for by gene X is not fully understood but it is associated with the development of liver cancer. It stimulates genes that promote cell growth and inactivates growth regulating molecules.[49]
Pathogenesis

The life cycle of hepatitis B virus is complex. Hepatitis B is one of a few known
Serotypes and genotypes
The virus is divided into four major serotypes (adr, adw, ayr, ayw) based on antigenic epitopes presented on its envelope proteins, and into eight major genotypes (A–H). The genotypes have a distinct geographical distribution and are used in tracing the evolution and transmission of the virus. Differences between genotypes affect the disease severity, course and likelihood of complications, and response to treatment and possibly vaccination.[52][53] There are two other genotypes I and J but they are not universally accepted as of 2015.[54] The diversity of genotypes is not shown equally in the world. For example, A, D, and E genotypes have been seen in Africa prevalently while B and C genotypes are observed in Asia as widespread.[55]
Genotypes differ by at least 8% of their sequence and were first reported in 1988 when six were initially described (A–F).[56] Two further types have since been described (G and H).[57] Most genotypes are now divided into subgenotypes with distinct properties.[58]
Mechanisms
Hepatitis B virus primarily interferes with the functions of the liver by replicating in
During HBV infection, the host
Diagnosis
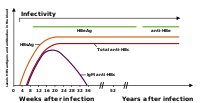
The tests, called assays, for detection of hepatitis B virus infection involve serum or blood tests that detect either viral antigens (proteins produced by the virus) or antibodies produced by the host. Interpretation of these assays is complex.[64]
The hepatitis B surface antigen (
Shortly after the appearance of the HBsAg, another antigen called hepatitis B e antigen (HBeAg) will appear. Traditionally, the presence of HBeAg in a host's serum is associated with much higher rates of viral replication and enhanced infectivity; however, variants of the hepatitis B virus do not produce the 'e' antigen, so this rule does not always hold true.[66] During the natural course of an infection, the HBeAg may be cleared, and antibodies to the 'e' antigen (anti-HBe) will arise immediately afterwards. This conversion is usually associated with a dramatic decline in viral replication.
If the host is able to clear the infection, eventually the HBsAg will become undetectable and will be followed by IgG antibodies to the hepatitis B surface antigen and core antigen (anti-HBs and anti HBc IgG).[39] The time between the removal of the HBsAg and the appearance of anti-HBs is called the window period. A person negative for HBsAg but positive for anti-HBs either has cleared an infection or has been vaccinated previously.
Individuals who remain HBsAg positive for at least six months are considered to be hepatitis B carriers.

PCR tests have been developed to detect and measure the amount of HBV DNA, called the viral load, in clinical specimens. These tests are used to assess a person's infection status and to monitor treatment.[69] Individuals with high viral loads, characteristically have ground glass hepatocytes on biopsy.
Prevention
Vaccine
Vaccines for the prevention of hepatitis B have been routinely recommended for babies since 1991 in the United States.[70] The first dose is generally recommended within a day of birth.[71] The hepatitis B vaccine was the first vaccine capable of preventing cancer, specifically liver cancer.[72]
Most vaccines are given in three doses over a course of days. A protective response to the vaccine is defined as an anti-HBs antibody concentration of at least 10 mIU/ml in the recipient's serum. The vaccine is more effective in children and 95 percent of those vaccinated have protective levels of antibody. This drops to around 90% at 40 years of age and to around 75 percent in those over 60 years. The protection afforded by vaccination is long lasting even after antibody levels fall below 10 mIU/ml. For newborns of HBsAg-positive mothers: hepatitis B vaccine alone, hepatitis B immunoglobulin alone, or the combination of vaccine plus hepatitis B immunoglobulin, all prevent hepatitis B occurrence.[73] Furthermore, the combination of vaccine plus hepatitis B immunoglobulin is superior to vaccine alone.[73] This combination prevents HBV transmission around the time of birth in 86% to 99% of cases.[74]
All those with a risk of exposure to body fluids such as blood should be vaccinated, if not already.[70] Testing to verify effective immunization is recommended and further doses of vaccine are given to those who are not sufficiently immunized.[70]
In 10- to 22-year follow-up studies there were no cases of hepatitis B among those with a normal immune system who were vaccinated. Only rare chronic infections have been documented.[78] Vaccination is particularly recommended for high risk groups including: health workers, people with chronic kidney failure, and men who have sex with men.[79][80][81]
Both types of the hepatitis B vaccine, the plasma-derived vaccine (PDV) and recombinant vaccine (RV) are of similar effectiveness in preventing the infection in both healthcare workers and chronic kidney failure groups.[79][80] With one difference noticed among health worker group, that the RV intramuscular route is significantly more effective compared with RV intradermal route of administration.[79]
Other
In assisted reproductive technology, sperm washing is not necessary for males with hepatitis B to prevent transmission, unless the female partner has not been effectively vaccinated.[82] In females with hepatitis B, the risk of transmission from mother to child with IVF is no different from the risk in spontaneous conception.[82]
Those at high risk of infection should be tested as there is effective treatment for those who have the disease.[83] Groups that screening is recommended for include those who have not been vaccinated and one of the following: people from areas of the world where hepatitis B occurs in more than 2%, those with HIV, intravenous drug users, men who have sex with men, and those who live with someone with hepatitis B.[83] Screening during pregnancy is recommended in the United States.[84]
Treatment
Acute hepatitis B infection does not usually require treatment and most adults clear the infection spontaneously.
Although none of the available medications can clear the infection, they can stop the virus from replicating, thus minimizing liver damage. As of 2018, there are eight medications licensed for the treatment of hepatitis B infection in the United States. These include antiviral medications lamivudine, adefovir, tenofovir disoproxil, tenofovir alafenamide, telbivudine, and entecavir, and the two immune system modulators interferon alpha-2a and PEGylated interferon alpha-2a. In 2015, the World Health Organization recommended tenofovir or entecavir as first-line agents.[90] Those with current cirrhosis are in most need of treatment.[90]
The use of interferon, which requires injections daily or thrice weekly, has been supplanted by long-acting PEGylated interferon, which is injected only once weekly.[91] However, some individuals are much more likely to respond than others, and this might be because of the genotype of the infecting virus or the person's heredity. The treatment reduces viral replication in the liver, thereby reducing the viral load (the amount of virus particles as measured in the blood).[92] Response to treatment differs between the genotypes. Interferon treatment may produce an e antigen seroconversion rate of 37% in genotype A but only a 6% seroconversion in type D. Genotype B has similar seroconversion rates to type A while type C seroconverts only in 15% of cases. Sustained e antigen loss after treatment is ~45% in types A and B but only 25–30% in types C and D.[93]
It seems unlikely that the disease will be eliminated by 2030, the goal set in 2016 by WHO. However, progress is being made in developing therapeutic treatments. In 2010, the Hepatitis B Foundation reported that 3 preclinical and 11 clinical-stage drugs were under development, based on largely similar mechanisms. In 2020, they reported that there were 17 preclinical- and 32 clinical-stage drugs under development, using diverse mechanisms.[15]
Prognosis

| no data <10 10–20 20–40 40–60 60–80 80–100 | 100–125 125–150 150–200 200–250 250–500 >500 |
Hepatitis B virus infection may be either acute (self-limiting) or chronic (long-standing). Persons with self-limiting infection clear the infection spontaneously within weeks to months.
Children are less likely than adults to clear the infection. More than 95% of people who become infected as adults or older children will stage a full recovery and develop protective immunity to the virus. However, this drops to 30% for younger children, and only 5% of newborns that acquire the infection from their mother at birth will clear the infection.[94] This population has a 40% lifetime risk of death from cirrhosis or hepatocellular carcinoma.[91] Of those infected between the age of one to six, 70% will clear the infection.[95]
Hepatitis D (HDV) can occur only with a concomitant hepatitis B infection, because HDV uses the HBV surface antigen to form a capsid.[96] Co-infection with hepatitis D increases the risk of liver cirrhosis and liver cancer.[97] Polyarteritis nodosa is more common in people with hepatitis B infection.
Cirrhosis
A number of different tests are available to determine the degree of cirrhosis present.
Reactivation
Hepatitis B virus DNA remains in the body after infection, and in some people, including those that do not have detectable HBsAg, the disease recurs.
Epidemiology

At least 296 million people, or 3.8% of the world's population, had chronic HBV infection as of 2019. Another 1.5 million cases of acute HBV infection also occurred that year.[1] Regional prevalences across the globe range from around 7.5% in Africa to 0.5% in the Americas.[19]
The primary method of HBV transmission and the prevalence of chronic HBV infection in specific regions often correspond with one another. In populations where HBV infection rates are 8% or higher, which are classified as high prevalence, vertical transmission (usually occurring during birth) is most common, though rates of early childhood transmission can also be significant among these populations.[106] In 2021, 19 African countries had infection rates ranging between 8-19%, placing them in the high prevalence category.[107]
In moderate prevalence areas where 2–7% of the population is chronically infected, the disease is predominantly spread horizontally, often among children, or vertically.[108] China's HBV infection rate is at the higher end of the moderate prevalence classification with an infection rate of 6.89% as of 2019.[109] HBV prevalence in India is also moderate, with studies placing India's infection rate between 2-4%.[110]
Countries with low HBV prevalence include Australia (0.9%),[111] those in the WHO European Region (which average 1.5%),[19] and most countries in North and South America (which average 0.28%).[112][113] In the United States, an estimated 0.26% of the population was living with HBV infection as of 2018.[114]
History
Findings of HBV DNA in ancient human remains have shown that HBV has infected humans for at least ten millennia, both in Eurasia and in the Americas.[115][116][117] This disproved the belief that hepatitis B originated in the New World and spread to Europe around 16th century.[117] Hepatitis B virus subgenotype C4 is exclusively present in Australian aborigines, suggesting an ancient origin as much as 50,000 years old.[118][119][120] However, analyses of ancient HBV genomes suggested that the most recent common ancestor of all known human HBV strains was dated to between 20,000 and 12,000 years ago,[115] pointing to a more recent origin for all HBV genotypes. The evolution of HBV in humans was shown to reflect known events of human history such as the first peopling of the Americas during the late Pleistocene and the Neolithic transition in Europe.[115] Ancient DNA studies have also showed that some ancient hepatitis viral strains still infect humans, while other strains became extinct.[115][116]
The earliest record of an epidemic caused by hepatitis B virus was made by Lurman in 1885..
The largest outbreak of Hepatitis B ever recorded was the infection of up to 330,000 American soldiers during World War II. The outbreak has been blamed on a yellow fever vaccine made with contaminated human blood serum, and after receiving the vaccinations about 50,000 soldiers developed jaundice.[122]
The virus was not discovered until 1966 when
Society and culture
World Hepatitis Day, observed 28 July, aims to raise global awareness of hepatitis B and hepatitis C and encourage prevention, diagnosis, and treatment. It has been led by the World Hepatitis Alliance since 2007 and in May 2010, it received global endorsement from the World Health Organization.[129]
See also
References
- ^ a b c d e f g h i j k l m n o p q r "Hepatitis B Fact Sheet". World Health Organization. 24 June 2022. Archived from the original on 9 August 2022. Retrieved 9 August 2022.
- ^ PMID 17336170.
- PMID 27733282.
- ^ a b c d e f g h i j k l m "Hepatitis B Fact sheet N°204". who.int. July 2014. Archived from the original on 9 November 2014. Retrieved 4 November 2014.
- ^ a b c d "Hepatitis B FAQs for the Public – Transmission". U.S. Centers for Disease Control and Prevention (CDC). Archived from the original on 11 December 2011. Retrieved 29 November 2011.
- ISBN 0-397-54589-4.
- ^ "Hepatitis MedlinePlus". U.S. National Library of Medicine. Retrieved 19 June 2020.
- ^ a b Centers for Disease Control and Prevention (30 March 2022). "Hepatitis B Questions and Answers for the Public - Symptoms". Archived from the original on 9 August 2022. Retrieved 9 August 2022.
- ISBN 9780781795166.
- ISBN 9781118637302.
- ISBN 978-92-4-156545-5.
- PMID 17673066.
- ^ "Immunization coverage- Global immunization coverage 2021". World Health Organization. 14 July 2022. Archived from the original on 10 August 2022. Retrieved 10 August 2022.
- S2CID 23924901.
- ^ PMID 34586871.
- PMID 32704164.
- ^ COMBATING HEPATITIS B AND C TO REACH ELIMINATION BY 2030. Geneva, Switzerland: World Health Organization. May 2016. Retrieved 6 January 2022.
- ^ PMID 27742003.
- ^ a b c d World Health Organization (2021). "Global progress report on HIV, viral hepatitis and sexually transmitted infections, 2021" (PDF). World Health Organization. Web Annex 1: Key data at a glance. Retrieved 10 August 2022.
{{cite web}}: CS1 maint: location (link) - PMID 8769597.
- S2CID 19746065.
- PMID 17570226.
- PMID 21992124.
- PMID 16247526.
- S2CID 9699144.
- PMID 11334492.
- PMID 4996611.
- ^ PMID 19399811.
- PMID 4098431.
- PMID 2023605.
- S2CID 28633855.
- ^ "Hepatitis B FAQs for the Public". Centers for Disease Control and Prevention. Archived from the original on 20 August 2015. Retrieved 24 August 2015.
- ^ "Hepatitis B – the facts: IDEAS –Victorian Government Health Information, Australia". State of Victoria. 28 July 2009. Archived from the original on 18 September 2011. Retrieved 19 September 2009.
- S2CID 39206739.
- S2CID 13524636.
- PMID 18831300. Archived from the original(PDF) on 7 August 2020. Retrieved 17 December 2018.
- S2CID 45638523.
- PMID 21536948.
- ^ from the original on 14 July 2009.
- S2CID 260320531.
- ISBN 978-0-12-375146-1.
- PMID 3014045.
- PMID 17383765.
- PMID 16461229.
- PMID 17206752.
- ^ PMID 17206754.
- PMID 26238794.
- OCLC 865013042.
- PMID 20170530.
- ^ PMID 23150796.
- PMID 17206755.
- PMID 15752827.
- PMID 8666521.
- PMID 26299884.
- S2CID 209577328.
- PMID 8291231.
- S2CID 25288772.
- PMID 17206751.
- PMID 10482623.
- PMID 17206752.
- S2CID 206211853.
- PMID 17316876.
- PMID 16258538.
- PMID 3331068.
- ISBN 978-0-12-375147-8.
- S2CID 25592461.
- S2CID 8713169.
- PMID 17935720.
- S2CID 260317291.
- ^ from the original on 19 June 2017.
- PMID 28847980.
- PMID 26578611.
- ^ PMID 16625613.
- PMID 24552860.
- S2CID 23620357.
- PMID 28188612.
- PMID 25385500.
- PMID 16754644.
- ^ PMID 16235273.
- ^ PMID 15266500.
- ^ "Men Who Have Sex with Men | Populations and Settings | Division of Viral Hepatitis | CDC". www.cdc.gov. 31 May 2015. Retrieved 13 December 2017.
- ^ PMID 19625309.
- ^ S2CID 9394711.
- PMID 31334800.
- )
- ^ HBV FAQs for Health Professionals | Division of Viral Hepatitis | CDC Archived 20 August 2017 at the Wayback Machine
- S2CID 40746103.
- PMID 21195373.
- PMID 26566064.
- ^ ISBN 978924154905-9. Archived(PDF) from the original on 19 March 2015.
- ^ PMID 18832247.
- S2CID 26270129.(subscription required)
- PMID 19998495.
- .
- S2CID 6437448.
- PMID 16364738.
- PMID 1661197.
- PMID 30641484.
- PMID 17981227.
- PMID 21195374.
- S2CID 37659362.
- S2CID 19400774.
- ^ PMID 22025876.
- ^ Bonacini, Maurizio, MD. "Hepatitis B Reactivation". University of Southern California Department of Surgery. Archived from the original on 27 November 2008. Retrieved 24 January 2009.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ "Hepatitis B incidence rate". Our World in Data. Retrieved 5 March 2020.
- PMID 25934461.
- ^ World Health Organization (2021). "Viral Hepatitis Scorecard 2021: African Region". WHO Regional Office for Africa. Archived from the original (PDF) on 10 August 2022. Retrieved 12 August 2022.
- S2CID 25088865.
- PMID 31533643.
- PMID 34691396.
- ^ Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine. "GESA Australian Consensus Recommendations". B Positive - Hepatitis B for Primary Care. Prevalence and epidemiology of hepatitis B. Archived from the original on 11 August 2022. Retrieved 11 August 2022.
- ^ Pan American Health Organization (December 2016). "Hepatitis B and C in the Spotlight. A public health response in the Americas, 2016" (PDF). IRIS PAHO. Retrieved 11 August 2022.
- ^ "Global hepatitis report, 2017". World Health Organization. 19 April 2017. Archived from the original on 11 August 2022. Retrieved 11 August 2022.
- S2CID 235371274. Retrieved 11 August 2022.
- ^ S2CID 238475573.
- ^ S2CID 13684815.
- ^ a b Ben Guarino (9 May 2018). "New strains of hepatitis B virus discovered in ancient human remains". The Washington Post. Retrieved 9 January 2018.
- S2CID 5208526.
- PMID 23870415.
- S2CID 25933906.
- ^ Lurman A (1885). "Eine icterus epidemic". Berl Klin Woschenschr (in German). 22: 20–3.
- ^ "World War II Hepatitis Outbreak Was Biggest in History". Associated Press. Boston. 16 April 1987. Retrieved 8 November 2020.
- PMID 5930797.
- .
- PMID 4190997.
- ^ "Hepatitis B Vaccine History". Hepatitis B Foundation. Retrieved 8 November 2020.
- PMID 399327.
- S2CID 43614988.
- ^ "Viral hepatitis" (PDF). World Health Organization. Archived (PDF) from the original on 11 August 2011.
External links
- Hepatitis B at Curlie
- GUIDELINES FOR THE PREVENTION, CARE AND TREATMENT OF PERSONS WITH CHRONIC HEPATITIS B INFECTION (PDF). World Health Organization. March 2015. ISBN 978924154905-9.
- "Hepatitis B virus". NCBI Taxonomy Browser. 10407.