Hepatorenal syndrome
| Hepatorenal syndrome | |
|---|---|
| Classification and external resources | |
| DiseasesDB | 5810 |
| MedlinePlus | [1] |
| eMedicine | med/1001 article/907429 |
| MeSH | D006530 |
Hepatorenal syndrome (often abbreviated HRS) is a life-threatening medical condition that consists of
HRS can affect individuals with cirrhosis, severe
The risk of death in hepatorenal syndrome is very high; the mortality of individuals with type 1 HRS is over 50% over the short term, as determined by historical
Classification

Hepatorenal syndrome is a particular and common type of
Type 1 hepatorenal syndrome
Type 1 HRS is characterized by rapidly progressive kidney failure, with a doubling of serum
In 2015, the International Club of Ascites updated their definition of HRS Type 1 in light of recent studies. Termed HRS-AKI, no minimum creatinine value is needed , that is, HRS-AKI can be diagnosed even when the serum creatinine is below 2.5mg/dl (221umol/L).
Requirement for HRS-AKI are:
- Increase in serum creatinine >0.3mg/L 26umol/L within 48 hrs OR increase by >1.5 times from baseline (reading from the last 3 months)
- No response to withdrawal of diuretics or administration of 1g/kg of albumin 20% over the last 2 days
- Cirrhosis with ascites
- Absence of
- Shock state
- Current or recent use of nephrotoxins (eg. NSAIDS, contrast dyes
- Signs of structural kidney disease
- proteinuria
- haematuria
- Normal findings on renal US
Type 2 hepatorenal syndrome
In contrast, type 2 HRS is slower in onset and progression, and is not associated with an inciting event. It is defined by an increase in serum creatinine level to >133 μmol/L (1.5 mg/dL) or a creatinine clearance of less than 40 mL/min, and a urine sodium < 10 μmol/L.[7] It also carries a poor outlook, with a median survival of approximately six months unless the affected individual undergoes liver transplantation. Type 2 HRS is thought to be part of a spectrum of illness associated with increased pressures in the portal vein circulation, which begins with the development of fluid in the abdomen (ascites). The spectrum continues with diuretic-resistant ascites, where the kidneys are unable to excrete sufficient sodium to clear the fluid even with the use of diuretic medications. Most individuals with type 2 HRS have diuretic-resistant ascites before they develop deterioration in kidney function.[8]
Similarly to the updated HRS-AKI, functional kidney injury in patients with cirrhosis that does not meet the criteria for HRS-AKI is termed HRS-NAKI. It can be divided into two groups, HRS-AKD, defined by eGFR <60ml/min/1.72 for less than 3 months, and HRS-CKD, defined by eGFR <60ml/min/1.72 for more than 3 months.
Signs and symptoms
Both types of hepatorenal syndrome share three major components: altered liver function, abnormalities in circulation, and death. As these phenomena may not necessarily produce symptoms until late in their course, individuals with hepatorenal syndrome are typically diagnosed with the condition on the basis of altered laboratory tests. Most people who develop HRS have cirrhosis, and may have signs and symptoms of the same, which can include jaundice, altered mental status, evidence of decreased nutrition, and the presence of ascites.[2] Specifically, the production of ascites that is resistant to the use of diuretic medications is characteristic of type 2 HRS. Oliguria, which is a decrease in urine volume, may occur as a consequence of kidney failure; however, some individuals with HRS continue to produce a normal amount of urine.[3] As these signs and symptoms may not necessarily occur in HRS, they are not included in the major and minor criteria for making a diagnosis of this condition; instead HRS is diagnosed in an individual at risk for the condition on the basis of the results of laboratory tests, and the exclusion of other causes.[3]
Causes
Hepatorenal syndrome usually affects individuals with
Certain precipitants of HRS have been identified in vulnerable individuals with cirrhosis or fulminant liver failure. These include bacterial infection, acute
Diagnosis
There can be many causes of kidney failure in individuals with cirrhosis or fulminant liver failure. Consequently, it is a challenge to distinguish hepatorenal syndrome from other entities that cause kidney failure in the setting of advanced liver disease. As a result, additional major and minor criteria have been developed to assist in the diagnosis of hepatorenal syndrome.[3]
The major criteria include liver disease with
The minor criteria are the following: a
Many other diseases of the kidney are associated with liver disease and must be excluded before making a diagnosis of hepatorenal syndrome. Individuals with
Pathophysiology


The
Studies to quantify this theory have shown that there is an overall decreased
The underfill theory involves activation of the renin–angiotensin–aldosterone system, which leads to an increase in absorption of sodium from the kidney tubule (termed renal sodium avidity) mediated by aldosterone, which acts on mineralocorticoid receptors in the distal convoluted tubule.[8][12] This is believed to be a key step in the pathogenesis of ascites in cirrhotics as well. It has been hypothesized that the progression from ascites to hepatorenal syndrome is a spectrum where splanchnic vasodilation defines both resistance to diuretic medications in ascites (which is commonly seen in type 2 HRS) and the onset of kidney vasoconstriction (as described above) leading to hepatorenal syndrome.[8]
Prevention

The risk of death in hepatorenal syndrome is very high; consequently, there is a significant emphasis on the identification of patients who are at risk for HRS, and prevention of triggers for onset of HRS. As
Individuals with ascites that have become infected spontaneously (termed spontaneous bacterial peritonitis or SBP) are at an especially high risk for the development of HRS.[2] In individuals with SBP, one randomized controlled trial found that the administration of intravenous albumin on the day of admission and on the third day in hospital reduced both the rate of kidney insufficiency and the mortality rate.[22]
Treatment
Transplantation
The definitive treatment for hepatorenal syndrome is
In anticipation of liver transplantation (which may be associated with considerable in-hospital delay), several other strategies have been found to be beneficial in preserving kidney function. These include the use of intravenous
Medical therapy
Many major studies showing improvement in kidney function in patients with hepatorenal syndrome have involved expansion of the volume of the plasma with albumin given intravenously.[2][25][26] The quantity of albumin administered intravenously varies: one cited regimen is 1 gram of albumin per kilogram of body weight intravenously on the first day, followed by 20 to 40 grams daily.[27] Notably, studies have shown that treatment with albumin alone is inferior to treatment with other medications in conjunction with albumin; most studies evaluating pre-transplant therapies for HRS involve the use of albumin in conjunction with other medical or procedural treatment.[2][28]
The vasopressin analogue ornipressin was found in a number of studies to be useful in improvement of kidney function in patients with hepatorenal syndrome,[1][25][32] but has been limited in its use, as it can cause severe ischemia to major organs.[1][25] Terlipressin is a vasopressin analogue that has been found in one large study to be useful for improving kidney function in patients with hepatorenal syndrome with a lesser incidence of ischemia.[1][26] A randomized control trial led by Florence Wong demonstrated improved renal function in individuals with Type 1 HRS treated with terlipressin and albumin over placebo.[33] A key criticism of all of these medical therapies has been heterogeneity in the populations investigated and the use of kidney function, instead of mortality, as an outcome measure.[34]
Other agents that have been investigated for use in treatment of HRS include pentoxifylline,[35] acetylcysteine,[36] and misoprostol.[1][37] The evidence for all of these therapies is based on either case series, or in the case of pentoxifylline, extrapolated from a subset of patients treated for alcoholic hepatitis.[1]
Procedural treatments
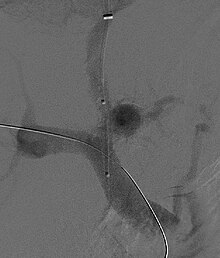
A
Renal replacement therapy may be required to bridge individuals with hepatorenal syndrome to liver transplantation, although the condition of the patient may dictate the modality used.[41] The use of dialysis, however, does not lead to recuperation or preservation of kidney function in patients with HRS, and is essentially only used to avoid complications of kidney failure until transplantation can take place. In patients who undergo hemodialysis, there may even be an increased risk of mortality due to low blood pressure in patients with HRS, although appropriate studies have yet to be performed. As a result, the role of renal replacement therapy in patients with HRS remains unclear.[2]
Epidemiology
As the majority of individuals with hepatorenal syndrome have cirrhosis, much of the epidemiological data on HRS comes from the cirrhotic population. The condition is quite common: approximately 10% of individuals admitted to hospital with ascites have HRS.[9] A retrospective case series of cirrhotic patients treated with terlipressin suggested that 20.0% of acute kidney failure in cirrhotics was due to type 1 HRS, and 6.6% was due to type 2 HRS.[18] It is estimated that 18% of individuals with cirrhosis and ascites will develop HRS within one year of their diagnosis with cirrhosis, and 39% of these individuals will develop HRS within five years of diagnosis.[9] Three independent risk factors for the development of HRS in cirrhotics have been identified: liver size, plasma renin activity, and serum sodium concentration.[9]
The prognosis of these patients is grim with untreated patients having an extremely short survival.[4][9][23] The severity of liver disease (as evidenced by the MELD score) has been shown to be a determinant of outcome.[24][42] Some patients without cirrhosis develop HRS, with an incidence of about 20% seen in one study of ill patients with alcoholic hepatitis.[35]
History
The first reports of kidney failure occurring in individuals with chronic liver diseases were from the late 19th century by Frerichs and Flint.
References
- ^ PMID 17603637.
- ^ PMID 10446954. Retrieved 17 July 2009.
- ^ S2CID 11973433.
- ^ PMID 12016430.
- ^ a b c d Mukherjee, S. Hepatorenal syndrome. emedicine.com. Retrieved on 2 August 2009
- PMID 25729433.
- PMID 3297907.
- ^ PMID 12737373.
- ^ PMID 8514039.
- PMID 15481347.
- S2CID 21358956.
- ^ S2CID 40231648.
- PMID 9709047.
- PMID 8068872.
- PMID 2676683.
- ^ PMID 1832407.
- PMID 2001805.
- ^ PMID 11910344.
- PMID 9927168.
- S2CID 21860692.
- ISBN 978-0-632-05582-1.
- PMID 10432325.
- ^ S2CID 22984489.
- ^ |intentional=yes}}.)
- ^ PMID 9425914.
- ^ S2CID 29927166.
- PMID 15084697.
- PMID 18471512.
- PMID 12830007.
- S2CID 21213418.
- S2CID 34909700.
- PMID 10498636.
- S2CID 232113995.
- S2CID 28068716.
- ^ PMID 11113085.
- S2CID 31985301.
- S2CID 208875962.
- ^ S2CID 43508937.
- PMID 15381144.
- PMID 10827226.
- S2CID 28850099.
- S2CID 205863757.
- ^ Helwig FC, Schutz CB (1932). "A liver kidney syndrome. Clinical pathological and experimental studies". Surg Gynecol Obstet. 55: 570–80.
- PMID 13377688.
- PMID 17699328.
- PMID 4890476.
47. Smith and Aitkenhead's Textbook of Anaesthesia 7th edition
