High-density lipoprotein
High-density lipoprotein (HDL) is one of the five major groups of
Overview
Lipoproteins are divided into five subgroups, by density/size (an inverse relationship), which also correlates with function and incidence of cardiovascular events. Unlike the larger lipoprotein particles, which deliver fat molecules to cells, HDL particles remove fat molecules from cells. The lipids carried include
Increasing concentrations of HDL particles are associated with decreasing accumulation of atherosclerosis within the walls of arteries,[4] reducing the risk of sudden plaque ruptures, cardiovascular disease, stroke and other vascular diseases.[2] HDL particles are commonly referred to as "good cholesterol", because they transport fat molecules out of artery walls, reduce macrophage accumulation, and thus help prevent or even regress atherosclerosis.[5] However, recent investigations have shown that very high concentrations of HDL particles can be associated with an increased mortality risk[6] and an increased cardiovascular risk, especially in hypertensive patients.[7]
Testing
Because of the high cost of directly measuring HDL and LDL (
The remainder of the serum cholesterol after subtracting the HDL is the non-HDL cholesterol. The concentration of these other components, which may cause atheroma, is known as the non-HDL-C. This is now preferred to LDL-C as a secondary marker as it has been shown to be a better predictor and it is more easily calculated.[10]
Structure and function
This section needs more primary sources. (May 2021) |  |
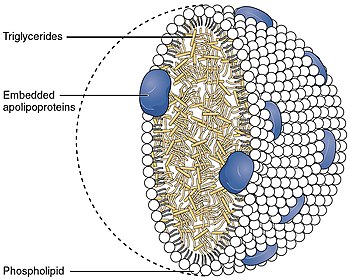
With a size ranging from 5 to 17 nm, HDL is the smallest of the
The liver synthesizes these lipoproteins as complexes of apolipoproteins and phospholipid, which resemble cholesterol-free flattened spherical lipoprotein particles,
HDL transports cholesterol mostly to the
The cholesterol delivered to the liver is excreted into the
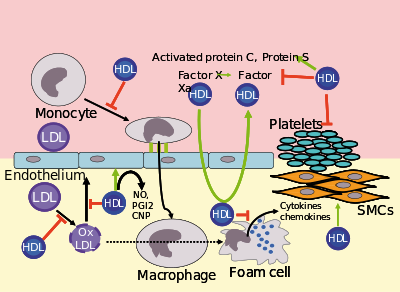
Several steps in the metabolism of HDL can participate in the transport of cholesterol from lipid-laden
HDL carries many lipid and protein species, several of which have very low concentrations but are biologically very active. For example, HDL and its protein and lipid constituents help to inhibit
In the
It has been postulated that the concentration of large HDL particles more accurately reflects protective action, as opposed to the concentration of total HDL particles.
Subfractions
Five subfractions of HDL have been identified. From largest (and most effective in cholesterol removal) to smallest (and least effective), the types are 2a, 2b, 3a, 3b, and 3c.[15]
Epidemiology
Men tend to have noticeably lower HDL concentrations, with smaller size and lower cholesterol content, than women. Men also have a greater incidence of atherosclerotic heart disease. Recent studies confirm the fact that HDL has a buffering role in balancing the effects of the hypercoagulable state in type 2 diabetics and decreases the high risk of cardiovascular complications in these patients. Also, the results obtained in this study revealed that there was a significant negative correlation between HDL and activated partial thromboplastin time (APTT).[citation needed]
Epidemiological studies have shown that high concentrations of HDL (over 60 mg/dL) have protective value against
Data from the landmark Framingham Heart Study showed that, for a given level of LDL, the risk of heart disease increases 10-fold as the HDL varies from high to low. On the converse, however, for a fixed level of HDL, the risk increases 3-fold as LDL varies from low to high.[16][17]
Even people with very low LDL levels under statins treatment are exposed to increased risk if their HDL levels are not high enough.[18]
Estimating HDL via associated cholesterol
Clinical laboratories formerly measured HDL cholesterol by separating other lipoprotein fractions using either ultracentrifugation or chemical precipitation with divalent ions such as Mg2+, then coupling the products of a cholesterol oxidase reaction to an indicator reaction. The reference method still uses a combination of these techniques.[19] Most laboratories now use automated homogeneous analytical methods in which lipoproteins containing apo B are blocked using antibodies to apo B, then a colorimetric enzyme reaction measures cholesterol in the non-blocked HDL particles.[20] HPLC can also be used.[21] Subfractions (HDL-2C, HDL-3C) can be measured,[22] but clinical significance of these subfractions has not been determined.[23] The measurement of apo-A reactive capacity can be used to measure HDL cholesterol but is thought to be less accurate.[citation needed]
Recommended ranges
The
| Level mg/dL | Level mmol/L | Interpretation |
|---|---|---|
| <40/50 men/women | <1.03 | Low HDL cholesterol, heightened risk considered correlated for heart disease |
| 40–59 | 1.03–1.55 | Medium HDL level |
| >59 | >1.55 | High HDL level, optimal condition considered correlated against heart disease |
High LDL with low HDL level is an additional risk factor for cardiovascular disease.[27]
Measuring HDL concentration and sizes
As technology has reduced costs and clinical trials have continued to demonstrate the importance of HDL, methods for directly measuring HDL concentrations and size (which indicates function) at lower costs have become more widely available and increasingly regarded as important for assessing individual risk for progressive arterial disease and treatment methods.[citation needed]
Electrophoresis measurements
Since the HDL particles have a net negative charge and vary by density & size, ultracentrifugation combined with electrophoresis have been utilized since before 1950 to enumerate the concentration of HDL particles and sort them by size with a specific volume of blood plasma. Larger HDL particles are carrying more cholesterol.
NMR measurements
Concentration and sizes of lipoprotein particles can be estimated using nuclear magnetic resonance fingerprinting.[28]
Optimal total and large HDL concentrations
The HDL particle concentrations are typically categorized by event rate percentiles based on the people participating and being tracked in the MESA[29] trial, a medical research study sponsored by the United States National Heart, Lung, and Blood Institute.
| MESA Percentile | Total HDL particles μmol/L | Interpretation |
|---|---|---|
| >75% | >34.9 | Those with highest (Optimal) total HDL particle concentrations & lowest rates of cardiovascular disease events |
| 50–75% | 30.5–34.5 | Those with moderately high total HDL particle concentrations & moderate rates of cardiovascular disease events |
| 25–50% | 26.7–30.5 | Those with lower total HDL particle concentrations & Borderline-High rates of cardiovascular disease |
| 0–25% | <26.7 | Those with lowest total HDL particle concentrations & Highest rates of cardiovascular disease events |
| MESA Percentile | Large HDL particles μmol/L | Interpretation |
|---|---|---|
| >75% | >7.3 | Those with highest (Optimal) Large HDL particle concentrations & lowest rates of cardiovascular disease events |
| 50–75% | 4.8–7.3 | Those with moderately high Large HDL particle concentrations & moderate rates of cardiovascular disease events |
| 25–50% | 3.1–4.8 | Those with lower Large HDL particle concentrations & Borderline-High rates of cardiovascular disease |
| 0–25% | <3.1 | Those with lowest Large HDL particle concentrations & Highest rates of cardiovascular disease events |
The lowest incidence of atherosclerotic events over time occurs within those with both the highest concentrations of total HDL particles (the top quarter, >75%) and the highest concentrations of large HDL particles. Multiple additional measures, including LDL particle concentrations, small LDL particle concentrations, VLDL concentrations, estimations of insulin resistance and standard cholesterol lipid measurements (for comparison of the plasma data with the estimation methods discussed above) are routinely provided in clinical testing.
Increasing HDL levels
While higher HDL levels are correlated with lower risk of cardiovascular diseases, no medication used to increase HDL has been proven to improve health.[2][30] As of 2017, numerous lifestyle changes and drugs to increase HDL levels were under study.[2]
HDL lipoprotein particles that bear
Diet and exercise
Certain changes in diet and exercise may have a positive impact on raising HDL levels:[32]
- Decreased intake of
- Aerobic exercise[37]
- Weight loss[38]
- Avocado consumption[39]
- Magnesium supplements raise HDL-C.[40]
- Addition of soluble fiber to diet[41]
- Consumption of
- Increased intake of unsaturated fats[44]
- Removal of trans fatty acids from the diet[45]
Most
Recreational drugs
HDL levels can be increased by smoking cessation,[38] or mild to moderate alcohol intake.[47][48][49][50][51][52]
Cannabis in unadjusted analyses, past and current cannabis use was not associated with higher HDL-C levels.[53] A study performed in 4635 patients demonstrated no effect on the HDL-C levels (P=0.78) [the mean (standard error) HDL-C values in control subjects (never used), past users and current users were 53.4 (0.4), 53.9 (0.6) and 53.9 (0.7) mg/dL, respectively].[53]
Exogenous
Pharmaceutical drugs and niacin
Pharmacologic (1- to 3-gram/day) niacin doses increase HDL levels by 10–30%,[59] making it the most powerful agent to increase HDL-cholesterol.[60][61] A randomized clinical trial demonstrated that treatment with niacin can significantly reduce atherosclerosis progression and cardiovascular events.[62] Niacin products sold as "no-flush", i.e. not having side-effects such as "niacin flush", do not, however, contain free nicotinic acid and are therefore ineffective at raising HDL, while products sold as "sustained-release" may contain free nicotinic acid, but "some brands are hepatotoxic"; therefore the recommended form of niacin for raising HDL is the cheapest, immediate-release preparation.[63] Both fibrates and niacin increase artery toxic homocysteine, an effect that can be counteracted by also consuming a multivitamin with relatively high amounts of the B-vitamins, but multiple European trials of the most popular B-vitamin cocktails, trial showing 30% average reduction in homocysteine, while not showing problems have also not shown any benefit in reducing cardiovascular event rates. A 2011 extended-release niacin (Niaspan) study was halted early because patients adding niacin to their statin treatment showed no increase in heart health, but did experience an increase in the risk of stroke.[64]
In contrast, while the use of statins is effective against high levels of LDL cholesterol, most have little or no effect in raising HDL cholesterol.[60] Rosuvastatin and pitavastatin, however, have been demonstrated to significantly raise HDL levels.[65]
The PPAR modulator GW501516 has shown a positive effect on HDL-C[67] and an antiatherogenic where LDL is an issue.[68] However, research on the drug has been discontinued after it was discovered to cause rapid cancer development in several organs in rats.[69][70]
See also
- Asymmetric dimethylarginine
- Cardiovascular disease
- Cholesteryl ester storage disease
- Endothelium
- Lipid profile
- Lysosomal acid lipase deficiency
References
- ^ "LDL and HDL: Bad and Good Cholesterol". Centers for Disease Control and Prevention. CDC. Archived from the original on 12 September 2017. Retrieved 11 September 2017.
- ^ PMID 35575917.
- PMID 25522985.
- PMID 34440638.
- ^ a b "HDL (Good), LDL (Bad) Cholesterol and Triglycerides". American Heart Association. 2021. Archived from the original on 28 July 2018. Retrieved 31 May 2021.
- PMID 28419274.
- PMID 35968698.
- from the original on 2011-05-29. Retrieved 2011-06-02.
- ^ Sirtori, Cesare R. (October 2006). "HDL and the progression of atherosclerosis: new insights". European Heart Journal Supplements. Archived from the original on 2015-02-01.
- ISBN 978-1-60327-502-6
- S2CID 27875177
- PMID 24016265.
- PMID 23059119.
- PMID 11374859.
- ^ "HDL, HDL2, and HDL3 subfractions, and the risk of acute myocardial infarction. A prospective population study in eastern Finnish men". Archived from the original on 2012-06-18. Retrieved 2012-06-11.
- PMID 21296318.
- PMID 12456232.
- S2CID 44794291.
- ^ "National Reference System for Cholesterol – Cholesterol Reference Method Laboratory Network – HDL Cholesterol Certification Protocol for Manufacturers" (PDF). CDC. Archived (PDF) from the original on 10 November 2013. Retrieved 10 November 2013.
- PMID 11514391. Archived from the originalon 2014-03-13. Retrieved 2013-11-10.
- PMID 9342008. Archived from the originalon 2008-07-24. Retrieved 2009-10-08.
- PMID 18223297.
- PMID 23312047.
- ^ "Cholesterol Levels". American Heart Association. Archived from the original on 8 February 2010. Retrieved 14 November 2009.
- ^ "What Do My Cholesterol Levels Mean?" (PDF). American Heart Association. September 2007. Archived from the original (PDF) on 3 December 2008. Retrieved 14 November 2009.
- ^ "Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Executive Summary" (PDF). National Heart, Lung, and Blood Institute (NHLBI). National Institutes of Health. May 2001. Archived (PDF) from the original on 2009-08-02. Retrieved 2009-12-03.
- ^ ASHWOOD, E. R., BURTIS, C. A., & BRUNS, D. E. (2008). Tietz fundamentals of clinical chemistry. (6th ed., p. 415). St. Louis, MO: Saunders Elsevier.
- PMID 17110242.
- ^ "mesa-nhlbi.org". Archived from the original on 2016-12-15. Retrieved 2016-12-07.
- PMID 25038074.
- PMID 21421846.
- About.com. Archivedfrom the original on 14 July 2006. Retrieved 8 October 2009.
- ^ "Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials". Ajcn.org. Archived from the original on 2012-08-14. Retrieved 2015-11-05.
- PMID 16582033. Archived from the originalon 2012-01-15. Retrieved 2012-09-01.
- PMID 20089734.
- PMID 16685042.
- PMID 10378497.
- ^ S2CID 743920.
- PMID 29635493.
- S2CID 13156080. Archived from the originalon 2010-08-31. Retrieved 2010-12-13.
HMG CoA Reductase is an important enzyme in lipid and cholesterol metabolism, but it is not the only one. The statins act by inhibiting, temporarily, the enzyme, in a dose response relationship whereas the magnesium ion (Mg2+) is an important part of a complex control and regulation of this important pathway. Both lower LDL-C, some statins can raise HDL-C and lower triglycerides, but Mg supplements do both quite reliably.
- S2CID 41025973.
- ^ "The Power of Fish". The Cleveland Clinic Heart and Vascular Institute. Archived from the original on 17 September 2009. Retrieved 8 October 2009.
- ^ "Vitamins and Supplements Lifestyle Guide – Flaxseed". WebMD. Archived from the original on 9 June 2016. Retrieved 12 August 2013.
- PMID 12716665.
- ^ "Trans fat: Avoid this cholesterol double whammy". Mayo Foundation for Medical Education and Research (MFMER). Archived from the original on 6 January 2014. Retrieved 25 June 2010.
- ISBN 978-3-540-22569-0. Archived from the originalon 2019-10-25.
- PMID 11864868.
- PMID 11734581.
- PMID 9719399.
- PMID 7749823.
- PMID 3987006.
- PMID 3772283.
- ^ PMID 23684393.
- PMID 23043194.
- S2CID 8104778.
- PMID 17853928. Archived from the originalon 2009-07-06. Retrieved 2009-04-29.
- PMID 15529025.
- S2CID 20876888.
- ^ Rader, Daniel J. (2004). "Raising HDL in Clinical Practice". Raising HDL in Clinical Practice: Clinical Strategies to Elevate HDL. Archived from the original on 12 September 2019. Retrieved 8 October 2009.
- ^ a b Brewer, H. Bryan (27 December 2005). "Raising HDL-Cholesterol and Reducing Cardiovascular Risk: An Expert Interview With H. Bryan Brewer, Jr, MD". Archived from the original on 12 September 2019. Retrieved 8 October 2009.
- S2CID 1009560.
- .
- S2CID 23980567.
- ^ "Study: Boosting Good Cholesterol With Niacin Did Not Cut Heart Risks : Shots – Health News". NPR. 2011-05-26. Archived from the original on 2015-03-27. Retrieved 2015-11-05.
- ^ "When is treatment indicated for high cholesterol level?". Archived from the original on 30 July 2012.
- ^ [1] Archived 1 March 2012 at the Wayback Machine
- PMID 15716581.
- PMID 27573670.
- ^ Geiger LE, Dunsford WS, Lewis DJ, Brennan C, Liu KC, Newsholme SJ (2009). PS 895 - Rat carcinogenicity study with GW501516, a PPAR delta agonist (PDF). 48th Annual Meeting of the Society of Toxicology. Baltimore: Society of Toxicology. p. 105. Archived from the original (PDF) on 2015-05-04.
- ^ Newsholme SJ, Dunsford WS, Brodie T, Brennan C, Brown M, Geiger LE (2009). PS 896 - Mouse carcinogenicity study with GW501516, a PPAR delta agonist (PDF). 48th Annual Meeting of the Society of Toxicology. Baltimore: Society of Toxicology. p. 105. Archived from the original (PDF) on 2015-05-04.