Hypercholesterolemia
| Hypercholesterolemia | |
|---|---|
| Other names | Hypercholesterolaemia, high cholesterol |
coronary heart disease | |
| Causes | Poor diet, junk food, fast food, diabetes, alcoholism, monoclonal gammopathy, dialysis therapy, nephrotic syndrome, hypothyroidism, Cushing's syndrome, anorexia nervosa |
| Differential diagnosis | Hyperlipidemia, hypertriglyceridemia |
Hypercholesterolemia, also called high cholesterol, is the presence of high levels of cholesterol in the blood.[1] It is a form of hyperlipidemia (high levels of lipids in the blood), hyperlipoproteinemia (high levels of lipoproteins in the blood), and dyslipidemia (any abnormalities of lipid and lipoprotein levels in the blood).[1]
Elevated levels of non-HDL cholesterol and LDL in the blood may be a consequence of
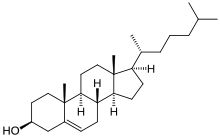
Cholesterol is one of three major classes of lipids produced and used by all animal cells to form membranes. Plant cells manufacture phytosterols (similar to cholesterol), but in rather small quantities.
Avoiding
Signs and symptoms
Although hypercholesterolemia itself is
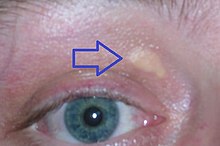
Some types of hypercholesterolemia lead to specific physical findings. For example, familial hypercholesterolemia (Type IIa hyperlipoproteinemia) may be associated with xanthelasma palpebrarum (yellowish patches underneath the skin around the eyelids),[13] arcus senilis (white or gray discoloration of the peripheral cornea),[14] and xanthomata (deposition of yellowish cholesterol-rich material) of the tendons, especially of the fingers.[15][16] Type III hyperlipidemia may be associated with xanthomata of the palms, knees and elbows.[15]
Causes
Hypercholesterolemia is typically due to a combination of environmental and genetic factors.[10] Environmental factors include weight, diet, and stress.[10][17] Loneliness is also a risk factor.[18]
Diet
Diet has an effect on blood cholesterol, but the size of this effect varies between individuals.[19][20]
A diet high in sugar or saturated fats increases total cholesterol and LDL.
A 2016 review found tentative evidence that dietary cholesterol is associated with higher blood cholesterol.[23] As of 2018 there appears to be a modest positive, dose-related relationship between cholesterol intake and LDL cholesterol.[24]
Medical conditions and treatments
A number of other conditions can also increase cholesterol levels including
Genetics
Genetic contributions typically arise from the combined effects of multiple genes, known as "polygenic," although in certain cases, they may stem from a single gene defect, as seen in
The Lithuanian Jewish population may exhibit a genetic founder effect.[28] One variation, G197del LDLR which is implicated in familial hypercholesterolemia, has been dated to the 14th century.[29] The utility[clarification needed] of these variations has been the subject of debate.[30]
Diagnosis
| Cholesterol type | mmol/L | mg/dL | Interpretation |
|---|---|---|---|
| total cholesterol | <5.2 | <200 | Desirable[31] |
| 5.2–6.2 | 200–239 | Borderline[31] | |
| >6.2 | >240 | High[31] | |
| LDL cholesterol | <2.6 | <100 | Most desirable[31] |
| 2.6–3.3 | 100–129 | Good[31] | |
| 3.4–4.1 | 130–159 | Borderline high[31] | |
| 4.1–4.9 | 160–189 | High and undesirable[31] | |
| >4.9 | >190 | Very high[31] | |
| HDL cholesterol | <1.0 | <40 | Undesirable; risk increased[31] |
| 1.0–1.5 | 41–59 | Okay, but not optimal[31] | |
| >1.55 | >60 | Good; risk lowered[31] |
Cholesterol is measured in milligrams per deciliter (mg/dL) of blood in the United States and some other countries. In the United Kingdom, most European countries and Canada, millimoles per liter of blood (mmol/L) is the measure.[32]
For healthy adults, the UK National Health Service recommends upper limits of total cholesterol of 5 mmol/L, and low-density lipoprotein cholesterol (LDL) of 3 mmol/L. For people at high risk of cardiovascular disease, the recommended limit for total cholesterol is 4 mmol/L, and 2 mmol/L for LDL.[33]
In the United States, the National Heart, Lung, and Blood Institute within the National Institutes of Health classifies total cholesterol of less than 200 mg/dL as "desirable", 200 to 239 mg/dL as "borderline high", and 240 mg/dL or more as "high".[34]
There is no absolute cutoff between normal and abnormal cholesterol levels, and values must be considered in relation to other health conditions and risk factors.[35][36][37]
Higher levels of total cholesterol increase the risk of cardiovascular disease, particularly coronary heart disease.[38] Levels of LDL or non-HDL cholesterol both predict future coronary heart disease; which is the better predictor is disputed.[39] High levels of small dense LDL may be particularly adverse, although measurement of small dense LDL is not advocated for risk prediction.[39] In the past, LDL and VLDL levels were rarely measured directly due to cost.[40][41][42]
Levels of fasting triglycerides were taken as an indicator of VLDL levels (generally about 45% of fasting triglycerides is composed of VLDL), while LDL was usually estimated by the Friedewald formula:
LDL total cholesterol – HDL – (0.2 x fasting triglycerides).[43]
However, this equation is not valid on nonfasting blood samples or if fasting triglycerides are elevated (>4.5 mmol/L or >~400 mg/dL). Recent guidelines have, therefore, advocated the use of direct methods for measurement of LDL wherever possible.
Classification
Classically, hypercholesterolemia was categorized by lipoprotein electrophoresis and the Fredrickson classification. Newer methods, such as "lipoprotein subclass analysis", have offered significant improvements in understanding the connection with atherosclerosis progression and clinical consequences. If the hypercholesterolemia is hereditary (familial hypercholesterolemia), more often a family history of premature, earlier onset atherosclerosis is found.[44]
Screening method
The
In Canada, screening is recommended for men 40 and older and women 50 and older.[48] In those with normal cholesterol levels, screening is recommended once every five years.[49] Once people are on a statin further testing provides little benefit except possibly to determine compliance with treatment.[50]
Treatment
Treatment recommendations have been based on four risk levels for heart disease.[51] For each risk level, LDL cholesterol levels representing goals and thresholds for treatment and other action are made.[51] The higher the risk category, the lower the cholesterol thresholds.[51]
| Risk category | Criteria for risk category | Consider lifestyle modifications | Consider medication | ||||
|---|---|---|---|---|---|---|---|
| No. of risk factors† | 10-year risk of myocardial ischemia
|
mmol/litre | mg/dL | mmol/litre | mg/dL | ||
| High | Prior heart disease | OR | >20% | >2.6[52] | >100 | >2.6 | >100 |
| Moderately high | 2 or more | AND | 10–20% | >3.4 | >130 | >3.4 | >130 |
| Moderate | 2 or more | AND | <10% | >3.4 | >130 | >4.1 | >160 |
| Low | 0 or 1 | >4.1 | >160 | >4.9 | >190 | ||
| †Risk factors include cigarette smoking, hypertension (BP ≥140/90 mm Hg or on antihypertensive medication), low HDL cholesterol (<40 mg/dL), family history of premature heart disease, and age (men ≥45 years; women ≥55 years). | |||||||
For those at high risk, a combination of lifestyle modification and
Lifestyle
Lifestyle changes recommended for those with high cholesterol include: smoking cessation, limiting alcohol consumption, increasing physical activity, and maintaining a healthy weight.[19]
Overweight or obese individuals can lower blood cholesterol by losing weight – on average a kilogram of weight loss can reduce LDL cholesterol by 0.8 mg/dl.[8]
Diet
Eating a diet with a high proportion of vegetables, fruit, dietary fibre, and low in fats results in a modest decrease in total cholesterol.[53][54][8]
Eating dietary cholesterol causes a small rise in serum cholesterol,
A 2020 Cochrane review found replacing
The National Lipid Association recommends that people with familial hypercholesterolemia restrict intakes of total fat to 25–35% of energy intake, saturated fat to less than 7% of energy intake, and cholesterol to less than 200 mg per day.[8] Changes in total fat intake in low calorie diets do not appear to affect blood cholesterol.[62]
Increasing soluble fiber consumption has been shown to reduce levels of LDL cholesterol, with each additional gram of soluble fiber reducing LDL by an average of 2.2 mg/dL (0.057 mmol/L).
Medication
Statins are the typically used medications, in addition to healthy lifestyle interventions.[66] Statins can reduce total cholesterol by about 50% in the majority of people,[39] and are effective in reducing the risk of cardiovascular disease in both people with[67] and without pre-existing cardiovascular disease.[68][69][70][71] In people without cardiovascular disease, statins have been shown to reduce all-cause mortality, fatal and non-fatal coronary heart disease, and strokes.[72] Greater benefit is observed with the use of high-intensity statin therapy.[73] Statins may improve quality of life when used in people without existing cardiovascular disease (i.e. for primary prevention).[72] Statins decrease cholesterol in children with hypercholesterolemia, but no studies as of 2010 show improved outcomes[74] and diet is the mainstay of therapy in childhood.[39]
Other agents that may be used include
Guidelines
In the US, guidelines exist from the National Cholesterol Education Program (2004)[77] and a joint body of professional societies led by the American Heart Association.[78]
In the UK, the
The Task Force for the management of dyslipidaemias of the European Society of Cardiology and the European Atherosclerosis Society published guidelines for the management of dyslipidaemias in 2011.[39]
Specific populations
Among people whose life expectancy is relatively short, hypercholesterolemia is not a risk factor for death by any cause including coronary heart disease.[80] Among people older than 70, hypercholesterolemia is not a risk factor for being hospitalized with myocardial infarction or angina.[80] There are also increased risks in people older than 85 in the use of statin drugs.[80] Because of this, medications which lower lipid levels should not be routinely used among people with limited life expectancy.[80]
The American College of Physicians recommends for hypercholesterolemia in people with diabetes:[81]
- Lipid-lowering therapy should be used for secondary prevention of cardiovascular mortality and morbidity for all adults with known coronary artery disease and type 2 diabetes.
- Statins should be used for primary prevention against macrovascular (coronary artery disease, cerebrovascular disease, or peripheral vascular disease) complications in adults with type 2 diabetes and other cardiovascular risk factors.
- Once lipid-lowering therapy is initiated, people with type 2 diabetes mellitus should be taking at least moderate doses of a statin.[82]
- For those people with type 2 diabetes who are taking statins, routine monitoring of liver function tests or muscle enzymes is not recommended except in specific circumstances.
Alternative medicine
A 2002 survey found that 1.1% of U.S. adults who used alternative medicine did so to treat high cholesterol. Consistent with previous surveys, this one found the majority of individuals (55%) used it in conjunction with
Epidemiology
Rates of high total cholesterol in the United States in 2010 are just over 13%, down from 17% in 2000.[87]
Average total cholesterol in the United Kingdom is 5.9 mmol/L, while in rural China and Japan, average total cholesterol is 4 mmol/L.[10] Rates of coronary artery disease are high in Great Britain, but low in rural China and Japan.[10]
Research directions
Gene therapy is being studied as a potential treatment.[88][89]
References
- ^ S2CID 208792416.
- ISSN 0021-9584.
- S2CID 30197456.
- PMID 15198959.
- S2CID 27738163.
- ^ "Healthy diet – Fact sheet N°394". World Health Organization. September 2015. Retrieved July 6, 2016.
- ^ PMID 26268692.
- ^ PMID 21600528.
- ^ "Hypercholesterolemia". Genetics Home Reference. Retrieved 16 May 2016.
- ^ S2CID 5339837.
- PMID 20554950.
- PMID 9603549.
- ISBN 978-0-7817-7578-6.
- PMID 18331643.
- ^ ISBN 978-0-7216-2921-6.
- ISBN 978-1-4160-2999-1.
- PMID 10600068.
- PMID 20652462.
- ^ PMID 22998604.
- PMID 9174470.
- PMID 26586275.
- PMID 9322581.
- S2CID 30969287.
- PMID 30596814.
- PMID 26561699.
- ^ "Hypercholesterolemia". Genetics Home Reference. U.S. National Institutes of Health. Retrieved 5 December 2013.
- PMID 28864697.
- PMID 15208782.
- PMID 11309683
- ^ "Jewish Genetics, Part 3: Jewish Genetic Diseases (Mediterranean Fever, Tay–Sachs, pemphigus vulgaris, Mutations)". www.khazaria.com. Retrieved 18 October 2018.
- ^ a b c d e f g h i j k Consumer Reports; Drug Effectiveness Review Project (March 2013). "Evaluating statin drugs to treat High Cholesterol and Heart Disease: Comparing Effectiveness, Safety, and Price" (PDF). Best Buy Drugs. Consumer Reports: 9. Retrieved 27 March 2013. which cites
- United States Department of Health and Human Services; National Heart Lung and Blood Institute; National Institutes of Health (June 2005). "NHLBI, High Blood Cholesterol: What You Need to Know". nhlbi.nih.gov. Archived from the original on 1 April 2013. Retrieved 27 March 2013.
- ^ "Diagnosis and treatment". Mayo Clinic. 2023-01-11. Archived from the original on 2024-03-13. Retrieved 2024-03-16.
- ^ Diagnosing High Cholesterol, NHS Choices. Retrieved 2013-03-09.
- ^ ATP III Guidelines At-A-Glance Quick Desk Reference, National Cholesterol Education Program. Retrieved 2013-03-09.
- ^
Davidson, Michael H.; Pradeep, Pallavi (2023-07-03). "Hormonal and Metabolic Disorders". MSD Manual Consumer Version. Archived from the original on 2023-11-14. Retrieved 2024-03-16.
Although there is no natural cutoff between normal and abnormal cholesterol levels, ...
- ^
"What Your Cholesterol Levels Mean". www.heart.org. 2017-11-16. Archived from the original on 2024-02-26. Retrieved 2024-03-16.
While cholesterol levels above "normal ranges" are important in your overall cardiovascular risk, like HDL and LDL cholesterol levels, your total blood cholesterol level should be considered in context with your other known risk factors.
- ^
Nantsupawat, Nopakoon; Booncharoen, Apaputch; Wisetborisut, Anawat; Jiraporncharoen, Wichuda; et al. (2019-01-26). "Appropriate Total cholesterol cut-offs for detection of abnormal LDL cholesterol and non-HDL cholesterol among low cardiovascular risk population". Lipids in Health and Disease. 18 (1): 28. PMID 30684968.
The current appropriate TC cutoff to determine whether patients need further investigation and assessment is between 200 and 240 mg/dL [1, 17, 18]. However, the appropriate cut-off point for the younger population who may have low cardiovascular risk have not been examined extensively in the literature. A recent study suggests that a TC cut of point of between 200 and 240 may not be appropriate in identifying high LDL-C levels in apparently healthy people.
- PMID 27016614.
- ^ PMID 21712404.
- ^
Superko, H. Robert (2009-05-05). "Advanced Lipoprotein Testing and Subfractionation Are Clinically Useful". Circulation. 119 (17): 2383–2395. PMID 19414656.
- ^ "New Information on Accuracy of LDL-C Estimation". American College of Cardiology. 2020-03-20. Archived from the original on 2023-12-06. Retrieved 2024-03-16.
- ^ "Friedewald equation for calculating VLDL and LDL - All About Cardiovascular System and Disorders". Johnson's Techworld - Reliving my hobbies. 2017-11-04. Archived from the original on 2023-09-28. Retrieved 2024-03-16.
- PMID 4337382.
- PMID 24404629. Retrieved 2021-01-04.
- ^ U.S. Preventive Services Task Force. "Screening for Lipid Disorders: Recommendations and Rationale". Archived from the original on 2015-02-10. Retrieved 2010-11-04.
- S2CID 20592431.
- PMID 27532917.
- PMID 14581310.
- PMID 12485966.
- PMID 21228612.
- ^ PMID 15249516.
- ^ Consumer Reports; Drug Effectiveness Review Project (March 2013). "Evaluating statin drugs to treat High Cholesterol and Heart Disease: Comparing Effectiveness, Safety, and Price" (PDF). Best Buy Drugs. Consumer Reports: 9. Retrieved 27 March 2013.
- PMID 24355095.
- PMID 23736950.
- ^ PMID 20536780.
- PMID 26109578.
- PMID 25286466.
- PMID 5846902.
- ^ "Scientific Report of the 2015 Dietary Guidelines Advisory Committee" (PDF). health.gov. 2015. p. 17. Retrieved 16 May 2016.
The 2015 DGAC will not bring forward this recommendation 644 because available evidence shows no appreciable relationship between consumption of dietary cholesterol and serum cholesterol, consistent with the conclusions of the AHA/ACC report.
- PMID 32827219.
- PMID 24723079.
- PMID 24139973.
Including only hypocaloric diets, the effects of low-fat vs high-fat diets on total cholesterol and LDL cholesterol levels were abolished.
- PMID 9925120.
- PMID 26269373.
- PMID 19403705.
- PMID 30586774.
- PMID 29069377.
- PMID 21989464.
- PMID 20934984.
- PMID 22607822.
- PMID 27838722.
- ^ PMID 23440795.
- S2CID 539314.
- S2CID 24263653.
- ^ National Institute for Health and Clinical Excellence. Clinical guideline 67: Lipid modification. London, 2008.
- S2CID 54525085.
- PMID 30565953.
- ^ National Institute for Health and Clinical Excellence (18 July 2014). "Cardiovascular disease: risk assessment and reduction, including lipid modification". NICE. Retrieved 27 May 2019.
- ^ ABIM Foundation, AMDA – The Society for Post-Acute and Long-Term Care Medicine, retrieved 20 April 2015
- S2CID 6744974.
- S2CID 25448635.
- PMID 15188733.
- PMID 21735427.
- PMID 19091798.
- PMID 19158117.
- ^ Carrol, Margaret (April 2012). "Total and High-density Lipoprotein Cholesterol in Adults: National Health and Nutrition Examination Survey, 2009–2010" (PDF). CDC.
- PMID 21774774.
- PMID 21144047.

