Hysterosalpingography
This article has multiple issues. Please help improve it or discuss these issues on the talk page. (Learn how and when to remove these template messages)
|
| Hysterosalpingography | |
|---|---|
contrast medium filling the uterine cavity (small triangle in the center). | |
| Other names | Uterosalpingography |
| ICD-9-CM | 87.8 |
| MeSH | D007047 |
| MedlinePlus | 003404 |
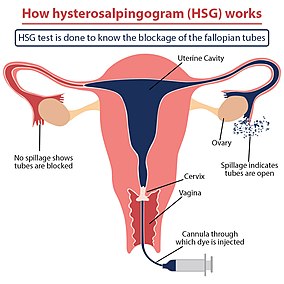
Hysterosalpingography (HSG), also known as uterosalpingography,
Uses
HSG is considered a
Occasionally, HSG may also have
HSG is contraindicated during menstruation, suspected cancer, pregnancy, unprotected sexual intercourse during the menstrual cycle, any purulent discharge from the vagina, or if the individual was diagnosed with pelvic inflammatory disease six months previously. For those with hypersensitivity to contrast, HSG is relatively contraindicated.
Procedure
Either high osmolar contrast material (HOCM) or low osmolar contrast material (LOCM) can be used. 10 to 20 ml of LOCM can be used at a concentration of 270 to 300 mg/ml. The contrast media should be prewarmed to room temperature before administered into the cervix, so as to prevent spasm of
The subject lies down on table in supine position with legs flexed and
The procedure involves x-rays (
Complications
Possible complications of the procedure include
History
For the first HSG, Carey used collergol in 1914. Lipiodol was introduced by Sicard and Forestier in 1924, and remained a popular contrast medium for many decades.[8] Later, water-soluble contrast material was generally preferred as it avoided the possible complication of oil embolism.
Follow up
If the HSG indicates further investigations are warranted, a laparoscopy, assisted by hysteroscopy, may be advised to visualize the area in three dimensions, with the potential to resolve minor issues within the same procedure.[citation needed]
See also
References
- ^ "Hysterosalpingography (Uterosalpingography)". RadiologyInfo. June 8, 2016.
- ^ a b c "Hysterosalpingography: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2019-05-06.
- ^ ISBN 9780702071669.
- PMID 28520519.
- S2CID 222421134.
- S2CID 238249552.
- ^ PMID 15950625.
- PMID 20265114.
External links
- HSG Test Archived 2018-12-21 at the Wayback Machine - HSG Test : Cost, Results, Expert Advice, Preparation
- HSG Archived 2020-10-27 at the Wayback Machine - HSG Test -HSG Film Advice, Preparation
