Innate immune system
This article needs to be updated. (March 2024) |
This article needs additional citations for verification. (March 2024) |

The innate immune system or nonspecific immune system
The major functions of the innate immune system are to:
- recruit immune cells to infection sites by producing chemical factors, including chemical mediators called cytokines
- activate the complement cascade to identify bacteria, activate cells, and promote clearance of antibody complexesor dead cells
- identify and remove foreign substances present in organs, tissues, blood and white blood cells
- activate the adaptive immune system through antigen presentation
- act as a physical and chemical barrier to infectious agents; via physical measures such as skin and mucus, and chemical measures such as host defence peptides.
Anatomical barriers
Anatomical barriers include physical, chemical and biological barriers. The epithelial surfaces form a physical barrier that is impermeable to most infectious agents, acting as the first line of defense against invading organisms.
| Anatomical barrier | Additional defense mechanisms |
|---|---|
| Skin | Sweat (including |
| Gastrointestinal tract | |
lungs |
Mucociliary escalator, defensins[3]
|
Nasopharynx |
Mucus, saliva, lysozyme[3] |
| Eyes | Tears[3] |
| Blood–brain barrier | endothelial cells (via passive diffusion/ osmosis & active selection). P-glycoprotein (mechanism by which active transportation is mediated)
|
Inflammation
Inflammation is one of the first responses of the immune system to infection or irritation. Inflammation is stimulated by chemical factors released by injured cells. It establishes a physical barrier against the spread of infection and promotes healing of any damaged tissue following pathogen clearance.[5]
The process of acute inflammation is initiated by cells already present in all tissues, mainly resident
Chemical factors produced during inflammation (
The inflammatory response is characterized by the following symptoms:
- redness of the skin, due to locally increased blood circulation;
- heat, either increased local temperature, such as a warm feeling around a localized infection, or a systemic fever;
- swelling of affected tissues, such as the upper throat during the common cold or joints affected by rheumatoid arthritis;
- increased production of mucus, which can cause symptoms like a productive cough;
- pain, either local pain, such as body aches; and
- possible dysfunction of involved organs/tissues.
Complement system
The
- trigger the recruitment of inflammatory cells
- "tag" pathogens for destruction by other cells by opsonizing, or coating, the surface of the pathogen
- form holes in the plasma membrane of the pathogen, resulting in cytolysis of the pathogen cell, causing its death
- rid the body of neutralised antigen-antibody complexes.
The three different complement systems are classical, alternative and lectin.
- Classical: starts when antibody binds to bacteria
- Alternative: starts "spontaneously"
- Lectin: starts when lectins bind to mannose on bacteria
Elements of the complement cascade can be found in many non-mammalian species including plants, birds, fish, and some species of invertebrates.[7]
White blood cells

White blood cells (WBCs) are also known as
The innate leukocytes include:
Mast cells
Mast cells are a type of innate immune cell that resides in connective tissue and in mucous membranes. They are intimately associated with wound healing and defense against pathogens, but are also often associated with allergy and anaphylaxis.[5] When activated, mast cells rapidly release characteristic granules, rich in histamine and heparin, along with various hormonal mediators and chemokines, or chemotactic cytokines into the environment. Histamine dilates blood vessels, causing the characteristic signs of inflammation, and recruits neutrophils and macrophages.[5]
Phagocytes
The word 'phagocyte' literally means 'eating cell'. These are immune cells that engulf, or '
Phagocytosis of the hosts' own cells is common as part of regular tissue development and maintenance. When host cells die, either by apoptosis or by cell injury due to an infection, phagocytic cells are responsible for their removal from the affected site.[9] By helping to remove dead cells preceding growth and development of new healthy cells, phagocytosis is an important part of the healing process following tissue injury.

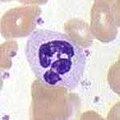
Macrophages
Macrophages, from the Greek, meaning "large eaters", are large phagocytic leukocytes, which are able to move beyond the vascular system by migrating through the walls of capillary vessels and entering the areas between cells in pursuit of invading pathogens. In tissues, organ-specific macrophages are differentiated from phagocytic cells present in the blood called monocytes. Macrophages are the most efficient phagocytes and can phagocytose substantial numbers of bacteria or other cells or microbes.[2] The binding of bacterial molecules to receptors on the surface of a macrophage triggers it to engulf and destroy the bacteria through the generation of a "respiratory burst", causing the release of reactive oxygen species. Pathogens also stimulate the macrophage to produce chemokines, which summon other cells to the site of infection.[2]
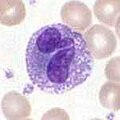
Neutrophils
Neutrophils, along with
Dendritic cells
Dendritic cells (DCs) are phagocytic cells present in tissues that are in contact with the external environment, mainly the
Basophils and eosinophils
Basophils and eosinophils are cells related to the neutrophil. When activated by a pathogen encounter,
Natural killer cells
γδ T cells
Like other 'unconventional' T cell subsets bearing invariant
Other vertebrate mechanisms
The
Increased levels of lactoferrin and transferrin inhibit bacterial growth by binding iron, an essential bacterial nutrient.[3]
Neural regulation
The innate immune response to infectious and sterile injury is modulated by neural circuits that control cytokine production period. The inflammatory reflex is a prototypical neural circuit that controls cytokine production in the spleen.[15] Action potentials transmitted via the vagus nerve to the spleen mediate the release of acetylcholine, the neurotransmitter that inhibits cytokine release by interacting with alpha7 nicotinic acetylcholine receptors (CHRNA7) expressed on cytokine-producing cells.[16] The motor arc of the inflammatory reflex is termed the cholinergic anti-inflammatory pathway.
Pathogen-specificity
The parts of the innate immune system display specificity for different pathogens.
| Pathogen | Main examples[17] | Phagocytosis[17] | complement[17] | NK cells[17]
|
|---|---|---|---|---|
| Intracellular and cytoplasmic virus | yes | yes[18] | yes | |
| Intracellular bacteria | yes (specifically neutrophils ) |
yes[19] | yes | |
| no | yes | yes | ||
| Extracellular bacteria |
|
yes | yes | no |
| Intracellular protozoa | no | no | yes | |
| Extracellular protozoa |
|
yes | yes | no/yes |
| Extracellular fungi |
|
no | yes | yes[20] |
Immune evasion
Innate immune system cells prevent free growth of microorganisms within the body, but many pathogens have evolved mechanisms to evade it.[21][22]
One strategy is intracellular replication, as practised by
Bacteria and fungi may form complex biofilms, protecting them from immune cells and proteins; biofilms are present in the chronic Pseudomonas aeruginosa and Burkholderia cenocepacia infections characteristic of cystic fibrosis.[25]
Viruses
Type I
Some viruses evade this by producing molecules that interfere with IFN production. For example, the
Beyond vertebrates
Prokaryotes
Invertebrates
Proteolytic cascades
In invertebrates, PRRs trigger proteolytic cascades that degrade proteins and control many of the mechanisms of the innate immune system of invertebrates—including hemolymph coagulation and melanization. Proteolytic cascades are important components of the invertebrate immune system because they are turned on more rapidly than other innate immune reactions because they do not rely on gene changes. Proteolytic cascades function in both vertebrate and invertebrates, even though different proteins are used throughout the cascades.[36]
Clotting mechanisms
In the hemolymph, which makes up the fluid in the circulatory system of
Plants
Members of every class of pathogen that infect humans also infect plants. Although the exact pathogenic species vary with the infected species, bacteria, fungi, viruses, nematodes, and insects can all cause
Like invertebrates, plants neither generate antibody or T-cell responses nor possess mobile cells that detect and attack pathogens. In addition, in case of infection, parts of some plants are treated as disposable and replaceable, in ways that few animals can. Walling off or discarding a part of a plant helps stop infection spread.[37]
Most plant immune responses involve systemic chemical signals sent throughout a plant. Plants use PRRs to recognize conserved microbial signatures. This recognition triggers an immune response. The first plant receptors of conserved microbial signatures were identified in rice (
"Resistance" (R) proteins, encoded by
See also
References
- ^ "Immune response: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 7 November 2021.
- ^ ISBN 0-8153-4101-6..
- ^ a b c d e f g h i j k l m n o p q Mayer G. "Innate (Non-Specific) Immunity". Immunology Section of Microbiology and Immunology On-line. University of South Carolina.
- ^ "Mucociliary escalator". Saunders Comprehensive Veterinary Dictionary (3rd ed.). Elsevier, Inc. 2007. Retrieved 11 June 2018.
- ^ a b c d e f g Stvrtinová V, Jakubovský J, Hulín I (1995). "Inflammation and Fever". Pathophysiology: Principles of Disease. Computing Centre, Slovak Academy of Sciences: Academic Electronic Press. Archived from the original on 18 June 2007.
- S2CID 27691169.
- ISBN 0-443-07310-4.
- PMID 35265979.
- ^ ISBN 0815332181.
- ISBN 0-443-07310-4.
- PMID 18836917.
- PMID 11522236.
- PMID 8152260.
- ^ Klingemann HG (2010). "Development and testing of NK cell lines". In Lotze MT, Thompson AW (eds.). Natural killer cells - Basic Science and Clinical applications. pp. 169–175.
- PMID 17273548.
- PMID 19461672.
- ^ ISBN 978-0-7817-9543-2.
- PMID 28670306.
- PMID 8225590.
- S2CID 43258057.
- ^ Kennedy A. "Immune Evasion by bacteria". Crohnie. Archived from the original on 10 October 2006. Retrieved 25 October 2006.
- S2CID 15418509.
- PMID 9184008.
- ISBN 0-7216-0146-4.
- S2CID 31788349.
- PMID 12088676.
- ^ S2CID 14357403.
- PMID 19882216.
- PMID 26712804.
- PMID 9878611.
- PMID 20660196.
- ^ Peters P. "Restriction Enzymes". Access Excellence Classic Collection Background Paper.
- PMID 25120263.
- ^ PMID 8875808.
- PMID 11413042.
- ^ PMID 20541942.
- ^ a b c Schneider D (2005). "Plant immune responses". Stanford University Department of Microbiology and Immunology. Archived from the original on 9 June 2007.
- S2CID 10548988.
- S2CID 18311102.
- PMID 10911994.
- S2CID 3231431.
- ^ Chitosan#Agricultural and horticultural use
- ^ Linden JC, Stoner RJ, Knutson KW, Gardner-Hughes CA (2000). "Organic disease control elicitors" (PDF). Agro Food Industry Hi-Tech. 11 (5): 32–34. Archived from the original (PDF) on 6 July 2007.
- S2CID 4421274.
External links
- Breuer K, Foroushani AK, Laird MR, Chen C, Sribnaia A, Lo R, Winsor GL, Hancock RE, Brinkman FS, Lynn DJ. "InnateDB".
database of proteins and their interactions in innate immune
system - Innate Immune System Animation XVIVO Scientific Animation
