Kidd antigen system
The Kidd antigen system (also known as Jk antigen) are proteins found in the Kidd's blood group, which act as antigens, i.e., they have the ability to produce antibodies under certain circumstances. The Jk antigen is found on a protein responsible for urea transport in the red blood cells and the kidney.[1] They are important in transfusion medicine. People with two Jk(a) antigens, for instance, may form antibodies against donated blood containing two Jk(b) antigens (and thus no Jk(a) antigens). This can lead to hemolytic anemia, in which the body destroys the transfused blood, leading to low red blood cell counts. Another disease associated with the Jk antigen is hemolytic disease of the newborn, in which a pregnant woman's body creates antibodies against the blood of her fetus, leading to destruction of the fetal blood cells. Hemolytic disease of the newborn associated with Jk antibodies is typically mild, though fatal cases have been reported.[2]
The gene encoding this protein is found on chromosome 18.[3] Three Jk alleles are Jk (a), Jk (b)and Jk3. Jk (a) was discovered by Allen et al. in 1951 and is named after a patient (Mrs Kidd delivered a baby with a haemolytic disease of the newborn associated with an antibody directed against a new antigen Jk (a). Whereas Jk (b) was discovered by Plant et al. in 1953, individuals who lack the Jk antigen (Jk null) are unable to maximally concentrate their urine.[4]
Genetics and biochemistry
Kidd comprises three antigens on a
Kidd antigens
Jka (JK1) and Jkb (JK2)
Jka and Jkb are the products of alleles with Asp280 and Asn280 in the fourth external loop of the Kidd glycoprotein. Jka and Jkb have similar prevalences in White and Asian populations but Jka is more common in Black populations than Jkb.[5]
Kidd antigens are enhanced by enzymes[citation needed]
Jk(a-b-) and Jk3
Jk(a-b-) represents the null phenotype and usually results from homozygosity for a silent gene at the JK locus.[5] The null phenotype is rare in most populations but does have increased prevalence in Polynesians (one in 400) and Niueans (1.4%).[5]
In Polynesians the null allele contains a splice site mutation in intron 5 causing a loss of exon 6 from the mRNA product.[citation needed]
In Finns (null phenotype less rare than in other European populations), the null phenotype results from a mutation encoding a Ser291Pro substitution.[citation needed]
A rare null phenotype in Japanese individuals results from heterozygosity for an inhibitor gene. In(Jk) in analogy with the In(Lu) dominant inhibitor of Lutheran and other antigens.[5]
Immunized individuals with the Jk(a-b-) phenotype may produce anti-Jk3.[citation needed]
Very weak expression of Jka and/or Jkb can be detected on In(Jk) red blood cells in adsorption/elution tests.[5]
Kidd antibodies and clinical significance
Antibody subtypes and complement fixation
Anti-Jka and -Jkb are not common. They are usually warm-reacting IgG1 and IgG3 but may also include IgG2, IgG4 or IgM. Approximately 50% of anti-Jka and -Jkb antibodies are capable of binding complement.[6]
Dosage
Kidd antibodies display dosage: red cells from
Laboratory detection
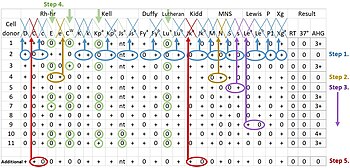
Kidd antibodies can be difficult to detect by direct agglutination testing and generally require addition of antihuman globulin after a warm incubation period.[citation needed]
Clinical significance
Kidd antibodies are dangerous as they are capable of causing severe acute
Kidd glycoprotein as urea transporter
Kidd antigens are located on a red blood cell urea transporter (human urea transporter 11- HUT11 or UT-B1).[8] As red blood cells approach the renal medulla (where there is a high concentration of urea), the urea transporter allows for rapid uptake of urea and prevents cell shrinkage in the hypertonic environment of the medulla.[5] As the red cell leaves the medulla, the urea is transported back out of the cell, preventing cellular swelling and preventing the urea from being carried away from the kidney.[5] HUT11 was detected on endothelial cells of the vasa recta (vascular supply of the renal medulla) but it is not present in renal tubules.[5]
Due to absence of the urea transporter, Jk(a-b-) cells are not hemolyzed by 2M urea. This can be used as a screening test for Jk(a-b-) donors.[citation needed]
The Jk(a-b-) phenotype has no clinical defect, although two individuals with this phenotype have been reported to have mild urine-concentrating defects.[4]
Kidd antibodies in transplant patients
Kidd antibodies are capable of behaving as histocompatibility antigens in renal transplants and may be responsible for allograft rejection in some cases.[9]
References
- Online Mendelian Inheritance in Man (OMIM): 111000 – OMIM page on the Kidd antigen system protein
- PMID 7797558
- PMID 16479082
- PMID 2890568
- ^ PMID 1498276
- ^ a b c d e f g h i j k Roback et al. AABB Technical Manual, 16th Ed. Bethesda, AABB Press, 2008.
- ^ Klein HG, Anstee DJ. Mollison's Blood Transfusion in Clinical Medicine. 11th Ed. Oxford: Blackwell Publishing, 2005.
- ^ a b Mais DD. ASCP Quick Compendium of Clinical Pathology, 2nd Ed. Chicago: ASCP Press, 2009.
- ^ Sands JM. Molecular Mechanisms of Urea Transport. Journal of Membrane Biology. 2003; 191: 149-63.
- ^ Hold S, Donaldson H, Hazelhurst G, et al. Acute Transplant Rejection Induced By Blood Transfusion Reaction to the Kidd Blood Group System. Nephrology Dialysis Transplantation. 2004; 19: 2403-6.
