Lacunar stroke
| Lacunar stroke | |
|---|---|
 | |
| CT scan of two lacunar strokes. | |
| Specialty | Neurology |
Lacunar stroke or lacunar cerebral infarct (LACI) is the most common type of
that provide blood to the brain's deep structures. Patients who present with symptoms of a lacunar stroke, but who have not yet had diagnostic imaging performed, may be described as having lacunar stroke syndrome (LACS).Much of the current knowledge of lacunar strokes comes from C. Miller Fisher's cadaver dissections of post-mortem stroke patients. He observed "lacunae" (empty spaces) in the deep brain structures after occlusion of 200–800 μm penetrating arteries and connected them with five classic syndromes. These syndromes are still noted today, though lacunar infarcts are diagnosed based on clinical judgment and radiologic imaging.
Signs and symptoms
This article needs additional citations for verification. (March 2022) |
Each of the five classical lacunar syndromes has a relatively distinct symptom complex. Symptoms may occur suddenly, progressively, or in a fluctuating (e.g., the capsular warning syndrome) manner. Occasionally, cortical infarcts and intracranial hemorrhages can mimic lacunar infarcts, but true cortical signs (aphasia,[1] visuospatial neglect, gaze deviation, and visual field defects) are always absent in lacunar strokes. The classic syndromes are as follows:[2][3]
| Name | Location of infarct | Presentation |
|---|---|---|
| Pure motor stroke/hemiparesis (most common lacunar syndrome: 33–50%) | posterior limb of the internal capsule, basilar part of pons , corona radiata
|
It is marked by hemiplegia that typically affects the face, arm, or leg of the side of the body opposite the location of the infarct. Dysarthria, dysphagia , and transient sensory symptoms may also be present.
|
| Ataxic hemiparesis (second most frequent lacunar syndrome) | posterior limb of the internal capsule, basilar part of pons, and corona radiata, red nucleus, lentiform nucleus, superior cerebellar artery infarcts, anterior cerebral artery infarcts
|
It displays a combination of cerebellar and motor symptoms, including weakness and clumsiness, on the ipsilateral side of the body.[4] It usually affects the leg more than it does the arm; hence, it is known also as homolateral ataxia and crural paresis. The onset of symptoms is often over hours or days. |
| Dysarthria/clumsy hand (sometimes considered a variant of ataxic hemiparesis, but usually still is classified as a separate lacunar syndrome) | basilar part of pons, anterior limb or genu of internal capsule, corona radiata, basal ganglia, thalamus, cerebral peduncle | The main symptoms are dysarthria and clumsiness (i.e., weakness) of the hand, which often are most prominent when the patient is writing; but dysarthria or involuntary movement can also be seen in legs.[5] |
| Pure sensory stroke | contralateral thalamus (VPL), internal capsule, corona radiata, midbrain | Marked by numbness (loss of sensation) on one side of the body; can later develop tingling, pain, burning, or another unpleasant sensation on one side of the body. |
| Mixed sensorimotor stroke | thalamus and adjacent posterior internal capsule, lateral pons | This lacunar syndrome involves hemiparesis or hemiplegia (weakness) with sensory impairment in the contralateral side.[6] |
Silent lacunar infarction

A silent lacunar infarction (SLI) is one type of
Pathophysiology
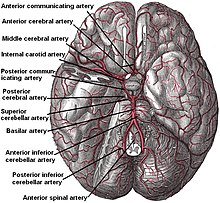
According to Koffler et al., lacunes are derived from an "occlusion of a single deep penetrating artery that arises directly from the constituents of the
The two proposed mechanisms are microatheroma and
More recent advances have also suggested these mechanisms may play a combined role in the aetiology of lacunar infarction. The most current theory indicates endothelial dysfunction and increased permeability of the blood-brain barrier first allow leakage of blood contents, promoting gliosis and white matter hyper-intensities on magnetic resonance imaging. Moreover, focal narrowing of brain vessels and impairment of their ability to dilate in response to various stimuli may lead to a decreased cerebral blood flow and ultimately lacunar stroke.[11]
Advanced age, chronic
Treatment and prognosis
Typically,
Patients who have lacunar strokes have a greater chance of surviving beyond thirty days (96%) than those with other types of stroke (85%), and better survival beyond a year (87% versus 65-70%). Between 70% and 80% are functionally independent at 1 year, compared with fewer than 50% otherwise.[12][13]
Occupational therapy and physical therapy interventions are used in the rehabilitation of lacunar stroke. A physiotherapy program will improve joint range of motion of the paretic limb using passive range of motion exercises. When increases in activity are tolerated, and stability improvements are made, patients will progress from rolling to side-lying, to standing (with progressions to prone, quadruped, bridging, long-sitting and kneeling for example) and learn to transfer safely (from their bed to a chair or from a wheel chair to a car for example). Assistance and ambulation aids are used as required as the patient begins walking and lessened as function increases. Furthermore, splints and braces can be used to support limbs and joints to prevent or treat complications such as contractures and spasticity.[14] The rehabilitation healthcare team should also educate the patient and their family on common stroke symptoms and how to manage an onset of stroke. Continuing follow-up with a physician is essential so that the physician may monitor medication dosage and risk factors.[14]
Epidemiology
It is estimated that lacunar infarcts account for 25% of all
References
- PMID 33591414.
- S2CID 202641797.
- PMID 21804774.
- ^ a b Lacunar Syndrome at eMedicine
- S2CID 53713034.
- PMID 22377873.
- S2CID 2768316.
- PMID 9740116.
- OCLC 1078637067.)
{{cite book}}: CS1 maint: location missing publisher (link) CS1 maint: others (link - PMID 25692102.
- PMID 30167649.
- PMID 3590244.
- PMID 18436869.
- ^ a b Lacunar Stroke at eMedicine
- S2CID 494869.
- S2CID 33602657.
