Listeria monocytogenes
| Listeria monocytogenes | |
|---|---|
| |
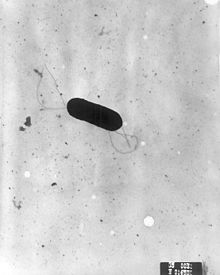
| Scanning electron micrograph of Listeria monocytogenes. | |
| Scientific classification | |
| Domain: | Bacteria |
| Phylum: | Bacillota |
| Class: | Bacilli |
| Order: | Bacillales |
| Family: | Listeriaceae |
| Genus: | Listeria |
| Species: | L. monocytogenes
|
| Binomial name | |
| Listeria monocytogenes (E. Murray et al. 1926) Pirie 1940
| |
Listeria monocytogenes is the species of pathogenic bacteria that causes the infection listeriosis. It is a facultative anaerobic bacterium, capable of surviving in the presence or absence of oxygen. It can grow and reproduce inside the host's cells and is one of the most virulent foodborne pathogens: 20 to 30% of foodborne listeriosis infections in high-risk individuals may be fatal.[1][2][3] In the European Union, listeriosis follows an upward trend that began in 2008, causing 2,161 confirmed cases and 210 reported deaths in 2014, 16% more than in 2013. Listeriosis mortality rates are also higher in the EU than for other foodborne pathogens.[4][5] Responsible for an estimated 1,600 illnesses and 260 deaths in the United States annually, listeriosis ranks third in total number of deaths among foodborne bacterial pathogens, with fatality rates exceeding even Salmonella spp. and Clostridium botulinum.
Listeria monocytogenes is a
Studies suggest up to 10% of human gastrointestinal tracts may be colonized by L. monocytogenes.[1] Nevertheless, clinical diseases due to L. monocytogenes are more frequently recognized by veterinarians, especially as meningoencephalitis in ruminants. See: listeriosis in animals.
Due to its frequent
Classification
L. monocytogenes is a Gram-positive, non-spore-forming, motile, facultatively anaerobic, rod-shaped bacterium. It is catalase-positive and oxidase-negative, and expresses a beta hemolysin, which causes destruction of red blood cells. This bacterium exhibits characteristic tumbling motility when viewed with light microscopy.[11] Although L. monocytogenes is actively motile by means of peritrichous flagella at room temperature (20−25 °C), the organism does not synthesize flagella at body temperatures (37 °C).[12]
The genus Listeria belongs to the class Bacilli and the order Bacillales, which also includes Bacillus and Staphylococcus. Listeria currently contains 27 species: Listeria aquatica, Listeria booriae, Listeria cornellensis, Listeria cossartiae, Listeria costaricensis, Listeria farberi, Listeria fleischmannii, Listeria floridensis, Listeria goaensis, Listeria grandensis, Listeria grayi, Listeria immobilis, Listeria innocua, Listeria ivanovii, Listeria marthii, Listeria monocytogenes, Listeria murrayi, Listeria newyorkensis, Listeria portnoyi, Listeria riparia, Listeria rocourtiae, Listeria rustica, Listeria seeligeri, Listeria thailandensis, Listeria valentina, Listeria weihenstephanensis, Listeria welshimeri. L. denitrificans, previously thought to be part of the genus Listeria, was reclassified into the new genus Jonesia.[13] Both L. ivanovii and L. monocytogenes are pathogenic in mice, but only L. monocytogenes is consistently associated with human illness.[14] The 13 serotypes of L. monocytogenes can cause disease, but more than 90% of human isolates belong to only three serotypes: 1/2a, 1/2b, and 4b. L. monocytogenes serotype 4b strains are responsible for 33 to 35% of sporadic human cases worldwide and for all major foodborne outbreaks in Europe and North America since the 1980s.[15]
History
L. monocytogenes was first described by E.G.D. Murray (Everitt George Dunne Murray) in 1924 based on six cases of sudden death in young rabbits, and published a description with his colleagues in 1926 .[16] Murray referred to the organism as Bacterium monocytogenes before
L. monocytogenes was not identified as a cause of foodborne illness until 1981, however. An outbreak of listeriosis in
Pathogenesis

Invasive
L. monocytogenes has D-galactose residues on its surface that can attach to D-galactose receptors on the host cell walls. These host cells are generally
The infective dose of L. monocytogenes varies with the strain and with the susceptibility of the victim. From cases contracted through raw or supposedly pasteurized milk, one may safely assume that, in susceptible persons, fewer than 1,000 total organisms may cause disease. L. monocytogenes may invade the gastrointestinal epithelium. Once the bacterium enters the host's
Regulation of pathogenesis
L. monocytogenes can act as a
Pathogenicity of lineages
L. monocytogenes has three distinct lineages, with differing evolutionary histories and pathogenic potentials.[37] Lineage I strains contain the majority of human clinical isolates and all human epidemic clones, but are underrepresented in animal clinical isolates.[37] Lineage II strains are overrepresented in animal cases and underrepresented in human clinical cases, and are more prevalent in environmental and food samples.[38] Lineage III isolates are very rare, but significantly more common in animal than human isolates.[37]
Detection

The Anton test is used in the identification of L. monocytogenes; instillation of a culture into the conjunctival sac of a rabbit or guinea pig causes severe keratoconjunctivitis within 24 hours.[39][40]
Listeria species grow on media such as Mueller-Hinton agar. Identification is enhanced if the primary cultures are done on agar containing sheep blood, because the characteristic small zone of hemolysis can be observed around and under colonies. Isolation can be enhanced if the tissue is kept at 4 °C for some days before inoculation into bacteriologic media. The organism is a facultative anaerobe and is catalase-positive and motile. Listeria produces acid, but not gas, when fermenting a variety of carbohydrates.[41] The motility at room temperature and hemolysin production are primary findings that help differentiate Listeria from Corynebacterium.[42]
The methods for analysis of food are complex and time-consuming. The present U.S. FDA method, revised in September 1990, requires 24 and 48 hours of enrichment, followed by a variety of other tests. Total time to identification takes five to seven days, but the announcement of specific non-radiolabelled
Recombinant DNA technology may even permit two- to three-day positive analysis in the future. Currently, the FDA is collaborating in adapting its methodology to quantitate very low numbers of the organisms in foods.[citation needed]
Treatment
When listeric meningitis occurs, the overall
A bacteriophage,
Use as a transfection vector
Because L. monocytogenes is an intracellular bacterium, some studies have used this bacterium as a vector to deliver genes in vitro. Current transfection efficiency remains poor. One example of the successful use of L. monocytogenes in in vitro transfer technologies is in the delivery of gene therapies for cystic fibrosis cases.[47]
Cancer treatment
Listeria monocytogenes is being investigated as a cancer immunotherapy for several types of cancer.[48][49]
A live attenuated Listeria monocytogenes
Epidemiology
Researchers have found Listeria monocytogenes in at least 37
Routes of infection
Listeria monocytogenes has been associated with such foods as raw
Infectious cycle
The primary site of infection is the intestinal epithelium, where the bacteria invade nonphagocytic cells via the "zipper" mechanism. Uptake is stimulated by the binding of listerial internalins (Inl) to
Following internalization, the bacterium must escape from the vacuole/phagosome before fusion with a lysosome can occur. Three main virulence factors that allow the bacterium to escape are listeriolysin O (LLO encoded by hly) phospholipase A (encoded by plcA) and phospholipase B (plcB).[54][55] Secretion of LLO and PlcA disrupts the vacuolar membrane and allows the bacterium to escape into the cytoplasm, where it may proliferate.[citation needed]
Once in the cytoplasm, L. monocytogenes exploits host actin for the second time. ActA proteins associated with the old bacterial cell pole (being a bacillus, L. monocytogenes septates in the middle of the cell, thus has one new pole and one old pole) are capable of binding the Arp2/3 complex, thereby inducing actin nucleation at a specific area of the bacterial cell surface. Actin polymerization then propels the bacterium unidirectionally into the host cell membrane. The protrusion formed may then be internalized by a neighboring cell, forming a double-membrane vacuole from which the bacterium must escape using LLO and PlcB. This mode of direct cell-to-cell spread involves a cellular mechanism known as paracytophagy.[56]
The ability of L. monocytogenes to successfully infect depends on its resistance to the high concentrations of
References
- ^ PMID 17332901. Archived from the original(PDF) on 2020-03-31. Retrieved 2010-09-05.
- PMID 31124782.
- ^ S2CID 163166441.
- ^ "Campylobacter and Listeria infections still rising in the EU – say EFSA and ECDC - European Food Safety Authority". www.efsa.europa.eu. 2015-12-17.
- .
- PMID 15302931.
- PMID 17661688. Retrieved 26 June 2006.
- PMID 31051570.
- ^ "Listeriosis (Listeria infection)". www.health.ny.gov. Retrieved 2015-11-16.
- ^ "CDC - Sources - Listeriosis". www.cdc.gov. Retrieved 2015-11-16.
- PMID 1943998.
- ^ Todar K (2008). "Listeria monocytogenes". Todar's Online Textbook of Bacteriology. Retrieved 28 January 2009.
- PMID 1713054.
- ^ "Chapter 15: Listeria monocytogenes". Compendium of Fish and Fishery Product Processes, Hazards, and Controls. Seafood Network Information Center. Seafood HACCP Alliance. 2007. Archived from the original on 23 June 2009. Retrieved 28 January 2009.
- PMID 15262937.
- .
- doi:10.1038/145264a0.
- PMID 14959337.
- PMID 11017828.
- PMID 6401354.
- ^ Ryser ET, Marth EH, eds. (1999). Listeria, Listeriosis, and Food. Safety (2nd ed.). New York: Marcel Dekker.
- ^ PMID 4956900.
- PMID 8507761.
- PMID 3608514.
- PMID 2919343.
- S2CID 248414580.
- PMID 110684.
- S2CID 43624806.
- PMID 1943998.
- PMID 11901162.
- PMID 2507553.
- S2CID 22599174.
- PMID 2122460.
- PMID 16428730.
- PMID 16102006.
- PMID 28114430.
- ^ PMID 11320113.
- PMID 15466521.
- ^ "Anton test - definition of Anton test in the Medical dictionary - by the Free Online Medical Dictionary, Thesaurus and Encyclopedia". Medical-dictionary.thefreedictionary.com. Retrieved 2013-08-05.
- ^ "Anton's eye test". Whonamedit. Retrieved 2013-08-05.
- ^ Brooks G, Carroll KC, Butel J, Morse S. "Chapter 13. Non-Spore-Forming Gram-Positive Bacilli: Corynebacterium, Propionibacterium, Listeria, Erysipelothrix, Actinomycetes, & Related Pathogens". Jawetz, Melnick, & Adelberg's Medical Microbiology (24th ed.). The McGraw-Hill Companies.
- PMID 8993861.
- ^ "103051F-EN-RevC" (PDF). Hologic. Archived from the original (PDF) on 6 September 2015. Retrieved 16 June 2016.
- ^ S2CID 11352292.
- PMID 16188359.
- ^ U.S. FDA/CFSAN: Agency Response Letter, GRAS Notice No. 000198
- S2CID 25275795.
- PMID 25623216.
- S2CID 45237800.
- ^ Lowry F (2008-05-15). "Live Listeria Vaccine Proves Safe Against End-Stage Cervical Ca in Human Trial". Ob. Gyn. News. 43 (10): 2.
- PMID 3918263.
- ^ "Outbreak of Listeria Infections Linked to Hard-boiled Eggs". 4 March 2020. Retrieved 14 March 2020.
- S2CID 31902805.
- PMID 15709360.
- PMID 12949110.
- PMID 10491395.
- ^ Merritt ME, Donaldson JR. Effect of bile salts on the DNA and membrane integrity of enteric bacteria. J Med Microbiol. 2009 Dec;58(Pt 12):1533-1541. doi: 10.1099/jmm.0.014092-0. Epub 2009 Sep 17. PMID 19762477
- ^ Kim SH, Gorski L, Reynolds J, Orozco E, Fielding S, Park YH, Borucki MK. Role of uvrA in the growth and survival of Listeria monocytogenes under UV radiation and acid and bile stress. J Food Prot. 2006 Dec;69(12):3031-6. doi: 10.4315/0362-028x-69.12.3031. PMID 17186676
External links
 Data related to Listeria monocytogenes at Wikispecies
Data related to Listeria monocytogenes at Wikispecies Media related to Listeria monocytogenes at Wikimedia Commons
Media related to Listeria monocytogenes at Wikimedia Commons- U.S. Food and Drug Administration. Foodborne Pathogenic Microorganisms and Natural Toxins Handbook: Listeria monocytogenes
- Public Health Agency of Canada
- Type strain of Listeria monocytogenes at BacDive - the Bacterial Diversity Metadatabase
